
Successful management of a combined cardiopulmonary penetrating injury: a case report
Introduction
Penetrating thoracic injury is a complex and serious injury that often results in hemorrhagic shock. When combined with cardiac and great vessel injury, the condition is critical, the development is rapid, and the fatality rate is extremely high. Penetrating cardiac injuries are highly deadly; most patients die before reaching the hospital, and the prehospital mortality rate has been reported to be as high as 94% (1). Penetrating cardiac injury is highly lethal with mortality rates of 70–80% (2). Cardiac injury occurs in about 20–30% of cases of major chest trauma (3). Penetrating chest injury can cause intracardiac injury at various sites, of which the right ventricle (43%) is the most common, followed by the left ventricle (33%), right atrium (15%), left atrium (6%), and intrapericardial great vessels (6%) (3). The incidence of a traumatic ventricular septal defect is 1–5% (3). The 2 most common causes of death in individuals with penetrating cardiac trauma are hemorrhagic shock and cardiac tamponade (4). As time is extremely crucial in almost all of traumatic injuries, early yet focused and careful evaluation is the key to early intervention and can improve mortality and morbidity. We present the following article in accordance with the CARE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3866/rc).
Case presentation
The patient, a male, aged 50 years, was admitted to the hospital following “a fall from a height [that] caused the steel bar[s] to penetrate the chest cavity for 7 hours before he arrived at the hospital”. The patient fell from a height of 3meters at a construction site, which caused 2 steel bars to penetrate his chest. The patient presented with symptoms such as chest pain, dyspnea, and apathy. The patient was in good health and had no family history of the disease. Of the 2 steel bars, 1 penetrated the chest by the right back and exited by the left anterior chest, while the other obliquely penetrated from the right back to the left back of the chest wall. The patient was lying in a bed when admitted to hospital.
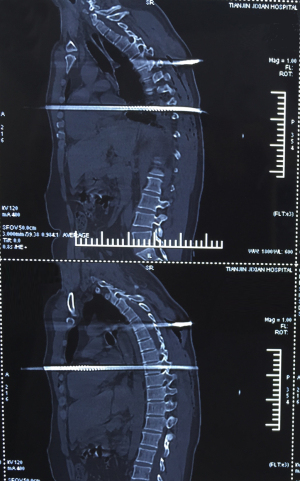
A physical examination revealed 3 bleeding wounds, but there was no clear bleeding tendency. The steel bar that vertically inserted and penetrated the chest formed a 110-degree angle with the body (see Figures 1,2). The steel bar was swinged with heartbeat very obviously. The preliminary diagnosis was a penetrating chest injury, a penetrating heart injury, and lung injury.
The patient was conscious, and his blood pressure was maintained at 110 mmHg. His heart rate was stable at 100 beats per minute with a normal oxygen saturation, and his central venous pressure was not high. Enhanced computed tomography (CT) scans showed that the steel bar pierced the heart near the left atrium and exited beside aortic root and thus was very likely causing damage to the ventricles (see Figures 3,4).

An emergency thoracotomy was not considered, as the patient was stable. A multidisciplinary team formulated the treatment plan. The preparation of the surgical treatment in the operation room was done very quickly, and at the same time, the patient’s blood was typed and cross-matched.
As the steel bar forms a certain angle inside and outside of body, it could not just be pulled out from the chest, and we could only pull it out from the back side. Taking into account the need for surgery, we cut off the part of bar outside the body very close to the chest wall, paying continual attention to any wound bleeding in the cutting process. Next, the patient placed in the supine position for the general anesthesia and placed on an esophageal ultrasound.
A median incision was chosen because of the position of the bars. Additionally, as a cardiopulmonary bypass (CPB) by the aorta to the inferior vena cava and the superior vena cava was not viable, we used a femoral artery and femoral vein in the CPB operation. After the CPB was performed, we opened the chest and pulled the chest very slowly under the guidance of esophageal ultrasound to prevent a cardiac rupture being caused by removing the bar.
After the chest was opened, we discovered that the steel bar pierced the heart from the left atrium close to the pulmonary vein side to the ventricular septum beside the right ventricular outflow tract (see Figure 5). This was further confirmed by a cardiac exploration that was performed after the right atrium and atrial septum were cut open. Next, we pulled the steel bar out very slowly from the left chest and confirmed that the bar did not injure the mitral valve, tricuspid valve, or any other important structure of the heart. The reparation of heart damage proceeded smoothly, but we observed that the left ventricular movement was reduced when stopping the CPB. It was highly possible that this was caused by the steel bar injuring the septal branch of the left anterior descending branch. Thus, we performed coronary artery bypass grafting (CABG) from the aorta to the left anterior descending branch with the great saphenous vein.
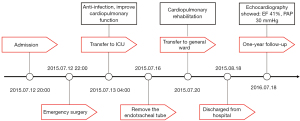
The wounds on both sides of the lung, chest and back were fixed after the CPB was completed. We then closed the chest and sent the patient back to the intensive care unit. The total operation time was 6 hours. The CPB time was 165 min, and the aortic occlusion time was 55 min. Postoperative treatment was given to prevent against infection and improve cardiopulmonary function. The patient recovered well, the reexamination results were satisfactory, and he was discharged from the hospital. The results of the follow-up 1 year after surgery were normal. The patient was followed up by telephone and said that the operation was successful. He basically returned to normal work and life after the operation. The timeline of the patient diagnosis and treatment process is shown in Figure 6.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Penetrating cardiac injuries are emergencies that require prompt surgical management. These injuries commonly require operative management. Patients who have unstable presentations may be temporized treated with a pericardial drain or fluid resuscitation, and when in extremis, may require an emergency room thoracotomy. Patients who are stable enough require a prompt transfer to a center with cardiothoracic and trauma expertise (5). The clinical manifestations of cardiac penetrating injury include the complete instability of the hemodynamics, acute hemorrhagic shock, complete respiratory, and cardiac arrest. In addition, its clinical manifestations are related to several factors, including the trauma mechanism, the length of time before arrival at the trauma center, the extent of injury, and whether there is lung injury. Regardless of whether the amount of blood loss is more than 40–50% or whether there is cardiac filling, penetrating heart wounds lead to the occurrence of cardiac shock in patients (6,7).
Penetrating cardiac injury requires urgent treatment, and the main causes of death of such patients are cardiac filling or bleeding caused by shock. Only 10–25% of such patients are still alive when they arrive at the hospital, and only 20% of such patients are stable (8,9), which is mainly due to the wound being sealed off by the foreign body (10). If this occurs, surgical treatment can have good results and the survival rate can be as high as 89% (10).
The localization of cardiac foreign bodies can be assisted by multiple imaging modalities including transthoracic echocardiogram (TTE), fluoroscopy, and CT as appropriate. TTE is a very useful tool for detecting cardiac injuries and represents the primary screening tool in unstable patients with chest trauma. CT is currently recommended as the initial imaging modality for hemodynamically stable patients (11). CT scans provide more information compared to X-ray about the cardiac wound and the presence of pericardial blood effusion and better display the position of the foreign body. In this case the performance of cardiac tamponade was not found but the steel penetration through the heart was observed on CT examination.
In cases of penetrating cardiac injuries, the foreign body should never be pulled out in an emergency department in any situation. These foreign bodies should be removed in a fully equipped operating room where an immediate thoracotomy can be done, as the foreign body may occlude the entrance site of major cardiovascular structures, thereby preventing bleeding (12,13). Median sternotomy is widely used, as it provides a clear view of frontal injuries and permits the repair of the majority of lesions as it did in this case (14).
The use of CPB is very necessary in patients with a clear heart injury. It can accurately and clearly repair heart damage and can repair the damage of the coronary artery at the same time (15). In this case, the CABG from the aorta to the left anterior descending branch improved the blood supply of the heart. This definitive repair can be realized with continuous or separate stitches, with 3-0 diameter polypropylene sutures, using pledgets, preferably in ventricular wounds. The surgeon should cover as much myocardial tissue as possible, as superficial repairs can cause more injuries to the fragile tissue around the wound (16).
A steel bar through the heart is very rare. Correctly diagnosing the patient and maintaining patient stability until surgical treatment can be administered are key to the survival of patients. Following the treatment of this patient, the author summarized the process by which the penetrating cardiac injury was treated at our hospital. The process was as follows: (I) a rapid diagnosis and timely surgery, which guaranteed the good prognosis of the patient; (II) a preoperative ultrasound combined with CT to confirm the diagnosis. (In the cases of stable hemodynamics, CT is the first choice); (III) the establishment of a CPB through the femoral artery and vein, which is a fast, safe and effective surgical method; and (IV) postoperative standardized and adequate anti-infective treatment.
Limitation
There were no similar cases that could be used for controlled studies. We will continue to accumulate data on similar cases.
Acknowledgments
Funding: This work was funded by the Tianjin Key Medical Discipline (Specialty) Construction Project (No. TJYXZDXK-042A).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-3866/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3866/coif). Both authors report that this work was funded by the Tianjin Key Medical Discipline (Specialty) Construction Project (No. TJYXZDXK-042A). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, including ensuring that any questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved. All the procedures performed in this study were conducted in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Agha RA, Borrelli MR, Farwana R, et al. The SCARE 2018 statement: Updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2018;60:132-6. [Crossref] [PubMed]
- Carr JA, Buterakos R, Bowling WM, et al. Long-term functional and echocardiographic assessment after penetrating cardiac injury: 5-year follow-up results. J Trauma 2011;70:701-4. [Crossref] [PubMed]
- Lee YC, Li JY. Delayed Complication of Penetrating Cardiac Injury: Traumatic VSD. Acta Cardiol Sin 2021;37:554-6. [PubMed]
- Hagiwara K, Inoue JI, Matumoto G, et al. Penetrating cardiac injury repaired under "intentional cardiac arrest" with adenosine triphosphate. Acute Med Surg 2021;8:e686. [Crossref] [PubMed]
- Eranki A, Wilson-Smith A, Villanueva C, et al. Penetrating cardiac trauma caused by a nail-gun: A case report and narrative review. Trauma Case Rep 2022;39:100649. [Crossref] [PubMed]
- Asensio JA, Stewart BM, Murray J, et al. Penetrating cardiac injuries. Surg Clin North Am 1996;76:685-724. [Crossref] [PubMed]
- Kaljusto ML, Skaga NO, Pillgram-Larsen J, et al. Survival predictor for penetrating cardiac injury; a 10-year consecutive cohort from a scandinavian trauma center. Scand J Trauma Resusc Emerg Med 2015;23:41. [Crossref] [PubMed]
- Kulshrestha P, Das B, Iyer KS, et al. Cardiac injuries--a clinical and autopsy profile. J Trauma 1990;30:203-7. [Crossref] [PubMed]
- Demetriades D, van der Veen BW. Penetrating injuries of the heart: experience over two years in South Africa. J Trauma 1983;23:1034-41. [PubMed]
- Attar S, Suter CM, Hankins JR, et al. Penetrating cardiac injuries. Ann Thorac Surg 1991;51:711-5; discussion 715-6. [Crossref] [PubMed]
- Wu W, Fang L, Yang Y, et al. Penetrating cardiac injury caused by large glass shards stabbing to the pericardium. Asian J Surg 2022;45:573-4. [Crossref] [PubMed]
- Actis Dato GM, Arslanian A, Di Marzio P, et al. Posttraumatic and iatrogenic foreign bodies in the heart: report of fourteen cases and review of the literature. J Thorac Cardiovasc Surg 2003;126:408-14. [Crossref] [PubMed]
- Søreide K, Petrone P, Asensio JA. Emergency thoracotomy in trauma: rationale, risks, and realities. Scand J Surg 2007;96:4-10. [Crossref] [PubMed]
- Jiang CL, Gu TX, Wang C. Surgical treatment of posttraumatic foreign bodies in the heart or great vessels. Chin Med J (Engl) 2006;119:2018-20. [Crossref] [PubMed]
- Chughtai TS, Gilardino MS, Fleiszer DM, et al. An expanding role for cardiopulmonary bypass in trauma. Can J Surg 2002;45:95-103. [PubMed]
- Struck GT, Nabhen JJ, Soek HA, et al. Transfixing heart injury by stab wound: Case report. Trauma Case Rep 2021;35:100518. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)





