
The clinical efficacy and safety of double reverse traction repositor and traction table in the reduction of unstable intertrochanteric fractures in elderly patients: a retrospective comparative study
Introduction
Femoral intertrochanteric fracture is one of the most common fractures in orthopedics, accounting for about 3.1% of all fractures. It mostly occurs in elderly patients over 60 years old and is a serious hip fracture (1,2). With the progress of social aging, the incidence of the disease is increasing (3). Currently, for unstable intertrochanteric fractures, proximal femoral anti-rotation intramedullary nail (PFNA) is usually used after reduction in an orthopedic traction table (TT) to obtain satisfactory bone healing (4). However, prolonged traction in an orthopedic TT can lead to complications such as pudendal nerve palsy and traction injury in the foot and ankle (5-7). To overcome these limitations, Zhao and colleagues from the Third Hospital of Hebei Medical University proposed the homeopathic reduction theory based on biomechanical principles, a systematic understanding of fracture anatomy, and clinical research, and developed the homeopathic double reverse traction repositor (DRTR) (8). Its working principle is to exert traction force on both ends of the fracture through bone-to-bone homeopathic traction, so as to conduct two-way and reverse traction. Since this is highly consistent with the mechanical axis of the limbs, and the traction force of the joints and soft tissue and the natural axis of the human body are used for reduction, the reduction quality is significantly improved, and its traction force is also significantly enhanced (9). Current studies indicated that DRTR enjoyed significant advantages, such as its continuous and stable reduction effect and simple operation, compared with TT in treatment of unstable femoral intertrochanteric fractures (8,10), femoral shaft fractures (9), distal femur fractures (11) and tibial plateau fractures (12), which has attracted extensive attention from orthopedic doctors. However, the clinical safety and efficacy of DRTR in treatment of elderly patients with unstable intertrochanteric fractures remains unknown. Therefore, this current retrospective study analyzed the clinical data of 42 elderly patients with unstable intertrochanteric fractures who were successfully followed up from October 2018 to December 2020. The effects of minimally invasive reduction with DRTR and orthopedic traditional reduction with TT on the postoperative outcomes were analyzed and compared. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4658/rc).
Methods
The patient inclusion and exclusion criteria
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (ethics approval No. [2021]-0162) and informed consent was taken from all the patients.
The following inclusion criteria were applied: (I) patients with a history of trauma, and unstable intertrochanteric fracture of the femur was diagnosed by X-ray (Figure 1) or computed tomography (CT) after injury; (II) patients with closed unilateral fractures; and (III) the PFNA was used for treatment.
The following exclusion criteria were applied: (I) patients with a pathological fracture; (II) patients with serious cardiovascular and cerebrovascular diseases, coagulation dysfunction, or other diseases that affect postoperative recovery; (III) patients were complicated with important organ injuries; and (IV) presentation of multiple fractures all over the body.
General information
From October 2018 to December 2020, a total of 42 elderly patients with unstable intertrochanteric fractures met the inclusion criteria of this study, and they were randomized to the DRTR group and TT group. There were 20 patients in DRTR group, including 15 males and 5 females, aged 62–85 years old, with an average age of 72.1±6.6 years (Table 1). The Arbeitsgemeinschaft fur Osteosynthesefragen (AO) classification of the fractures (Figure 2) in DRTR group was as follows: 5 cases with type 31-A2.2, 9 cases with type 31-A2.3, 4 cases with type 31-A3.1, and 2 cases with type 31-A3.2 (Table 1).
Table 1
| Groups | Number of cases | Sex (male/female) | Age (years), mean ± SD | Cause of injury (traffic accident/high fall injury/fall injury) | AO classification (31-A2.2/A2.3/A3.1/A3.2) |
|---|---|---|---|---|---|
| DRTR | 20 | 15/5 | 72.1±6.6 | 7/8/5 | 5/9/4/2 |
| TT | 22 | 16/6 | 70.8±6.1 | 6/10/6 | 6/10/3/3 |
| P value | 0.614 | 0.518 | 0.863 | 0.942 |
DRTR, double reverse traction repositor; TT, traction table; AO, Arbeitsgemeinschaft für Osteosynthesefragen.
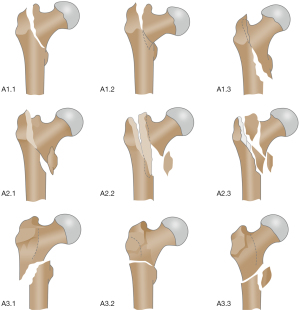
There were 22 cases in TT group, including 16 males and 6 females, aged 62–83 years old, with an average age of 70.8±6.1 years. The AO classification of the fractures in this group was as follows: 6 cases with type 31-A2.2, 10 cases with type 31-A2.3, 3 cases with type 31-A3.1, and 3 cases with type 31-A3.2 (Table 1).
Operation techniques
Operating methods
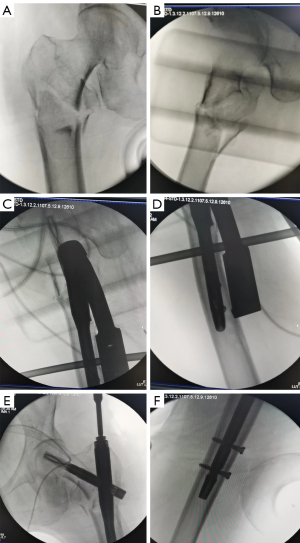
The operation began after successful general anesthesia of the patient. Patients were placed in the supine position, with the affected side elevated with padding. Preoperative preparations were performed according to the method of reduction with DRTR (Figure 3) and the conventional orthopedic TT.
For the minimally invasive reduction with DRTR, 3.0 Kirschner wires were placed in the femoral condyle. A small incision was made in the anterior superior iliac spine, and the proximal femoral traction rod was inserted to connect the traction arch and tractor of DRTR. Bone traction must be carried out along the long axis of the femur and stretched until the thigh muscles tighten (Figure 3).
For conventional orthopedic reduction with TT, the TT was installed and adjusted, and the patient was placed on his back with his limbs fixed. After traction, the affected limbs were properly retracted and rotated internally.
The C-arm X-ray fluoroscopy guided the traction reduction and adjustment of the fracture end until the fracture end reduction was satisfactory. A longitudinal incision was made from the apex of the greater trochanter with a length of 5–7 cm. The guide needle was insert at the apex of femoral trochanter, and the C-arm X-ray machine was used to confirm that the guide needle had entered the femoral medullary cavity. The medullary cavity is opened, the PFNA main nail is inserted, and the guide needle is drilled in the direction of the femoral neck on the side under the position of sight. Under the fluoroscopy of C-arm X-ray machine, the guide needle is located in the middle and lower third of femoral neck, and its lateral position is located in the center of femoral neck. The cortical bone is drilled along the guide needle, the appropriate locking nail is inserted with the spiral blade and locked after depth measurement. The guide is then used to lock the distal nail. After satisfactory fluoroscopy, the proximal tail cap of the main nail is tightened and the wound is sutured (Figure 4A-4F).
Postoperative management
After the operation, patients were administered anticoagulant drugs as per the doctor’s instructions. Depending on the postoperative drainage flow, the drainage tube may be removed at around day 2 post-surgery. Functional exercises in bed can be commenced on day 2 postoperatively to exercise the muscles and joint movements of the affected limbs. In terms of the postoperative recovery, patients were instructed to perform auxiliary training with crutches, and regular postoperative outpatient reviews were conducted to instruct functional exercises according to the recovery (Figure 5A-5F).

Observational indicators and follow-up procedures
The patient’s intraoperative conditions were monitored, including intraoperative reduction time, intraoperative blood loss, incision length, and operation time. The safety outcome was assessed by postoperative complications, and the efficacy outcomes were evaluated by the fracture healing times based on the radiographs conducted at each follow-up (1, 3, 6, 12 months after surgery) and hip function (hip flexion, Harris Hip Score) at the final follow-up (12 months after surgery). Of these, Harris Hip Score includes scores for pain, function, range of motion and deformity. The results were evaluated by two experienced doctors and averaged.
Follow-up procedures: Postoperative conditions were followed up by telephone and outpatient examination, which was performed at 1, 3, 6 and 12 months after surgery. All patients took pelvic anteroposterior and lateral X-ray films during outpatient review. The follow-up period of the study was 8–15 months, with a mean follow-up time of 12 months.
Statistical analysis
The SPSS Statistics 21 software was used for statistical analyses. Data were expressed as mean ± standard deviation. If the continuous variables were normally distributed, independent samples Welch’s t-tests were used; otherwise, Mann-Whitney U tests were used. Categorical variables were determined using the Chi-square test or Fisher’s test, as appropriate. Two-side P value <0.05 was considered statistically significant.
Results
A comparison of the intraoperative conditions between the two groups
Firstly, there were no significant differences in terms of demographics and fracture characteristics of cases enrolled (P>0.05), including sex, ages, cause of injury and AO classification of fracture, which indicated the baseline comparability of the two groups (Table 1). Subsequently, we performed the comparisons for efficacy and safety outcomes. In DRTR group, the intraoperative reduction time was 34.8±7.6 minutes, which was significantly shorter than the 56.6±9.3 minutes observed in TT group (P<0.0001; Table 2). Similarly, the average operation time of 87.1±12.2 minutes observed in DRTR group was significantly shorter than the average operation time of 123.1±15.0 minutes in TT group (P<0.0001; Table 2). However, there was no significant difference in incision length (P=0.1619) nor intraoperative bleeding volume (P=0.3941) between the 2 groups (Table 2).
Table 2
| Groups | Preoperative preparation time (min) | Operation time (min) | Length of incision (cm) | Intraoperative bleeding volume (mL) |
|---|---|---|---|---|
| DRTR | 34.8±7.6 | 87.1±12.2 | 6.4±0.9 | 152.6±22.9 |
| TT | 56.6±9.3 | 123.1±15.0 | 6.8±1.1 | 146.8±20.7 |
| P value | <0.0001 | <0.0001 | 0.1619 | 0.3941 |
Data are presented as the mean ± SD. DRTR, double reverse traction repositor; TT, traction table.
A comparison of the postoperative conditions between the two groups
During the postoperative follow-up period, no significant difference was observed in the fracture healing time (P=0.2350) nor the Harris score of hip joints (P=0.4496) between the DRTR group and the TT group at one year after the operation (Table 3).
Table 3
| Groups | Fracture healing time (weeks) | Harris score |
|---|---|---|
| DRTR | 13.8±1.5 | 84.4±6.6 |
| TT | 14.4±1.8 | 82.7±7.2 |
| P value | 0.2350 | 0.4496 |
Data are presented as the mean ± SD. DRTR, double reverse traction repositor; TT, traction table.
Discussion
This present study investigated the effects of invasive reduction with DRTR combined with PFNA internal fixation in the treatment of unstable femoral intertrochanteric fractures in the elderly and confirmed that the intraoperative reduction time and operation time were significantly shorter in patients who underwent minimally invasive reduction with DRTR compared to those who underwent conventional reduction with TT. However, there were no statistically significant differences in incision length, intraoperative blood loss, fracture healing time, nor Harris score of the hip joint function at one year after the operation, which was consistent with a previous study (10). The follow-up period of the study was 8–15 months, with a mean follow-up time of 12 months. One patient in TT group experienced lower extremity intermuscular venous thrombosis after the operation. There were no other surgery-related complications in any other patient after the operation and during follow-up.
Femoral intertrochanteric fractures usually occur in the elderly patients and are associated with poor prognosis and prolonged bed rest, which can consequently lead to high rates of disability and mortality (10). With the increased incidence of intertrochanteric fractures of the femur, there has been a focus on fracture fixation modalities, particularly intramedullary and extramedullary fixation. Intramedullary fixation has some advantages over extramedullary fixation, such as increasing patient activity and reducing the operation failure rate (13-15). PFNA has been widely used in intertrochanteric fractures in recent years because of its advantages of short operation time, less trauma, quick recovery, and high fracture healing rate (16-19). Moreover, its therapeutic effect has been widely recognized (20,21). The supine position on the TT during the orthopedic operation is the conventional position for the treatment of intertrochanteric fracture of the femur with PFNA internal fixation. Its advantage is that the axial traction force is large, which is beneficial for correcting the shortening of the affected limb and maintaining fracture reduction. However, this treatment method also has some shortcomings. The TT method is time-consuming and laborious during intraoperative reduction, thereby, increasing the operation time. Furthermore, it is inconvenient to readjust the reduction of the fracture end during the operation, the surgical incision must be enlarged for obese patients to ensure operation success, and some elderly and frail patients may find it difficult to tolerate lying on the TT (22). Therefore, in this study, the DRTR was applied to the preoperative reduction of PFNA internal fixation for unstable intertrochanteric femur fractures. The study demonstrated that the DRTR had good results in minimally invasive reduction, including reducing the intraoperative reduction time, reducing the operation time, and facilitating the adjustment of the fracture end reduction intraoperatively. However, there was no significant difference between the DRTR and TT in terms of the length of incision, the bleeding volume during operation, the time of fracture healing, nor the Harris score of hip joint function at one year after the operation. In contrast, another study showed that reduction with DRTR combined with PFNA internal fixation for intertrochanteric fractures could significantly reduce the bleeding volume, the number of intraoperative fluoroscopy, and increase the scores of hip and knee joint function at 1 and 3 months after the operation, but there was no statistical difference in hip and knee joint function in long-term follow-up (23). Furthermore, compared with the TT, the DRTR is small in size, low in cost, and simple in operation, and therefore it is convenient to popularize and apply this method in more grass-roots hospitals. However, we also found that after applying the DRTR, patients may experience postoperative pain on the femoral condyle, although this usually only lasted for about a week and was relieved spontaneously (24). In contrast, when applying the TT, another professional doctor is needed to adjust the traction bed during the operation, which increases the burden on manpower. In addition, the perineal column may cause crush injury to the patient’s perineum after the operation, although this is generally mild and can be relieved spontaneously.
This study has some limitations. First, this was a single-center retrospective study and not all patient data were available for evaluation. Second, the number of cases in this study was small and some possible complications may not have been observed. In addition, the follow-up period of this study was not very long, and further long-term follow-up is warranted to assess the long-term postoperative effects.
In conclusion, compared with the traditional orthopedic TT, the intraoperative reduction of PFNA internal fixation for unstable intertrochanteric femur fractures using a DRTR with minimally invasive reduction has certain advantages and might be worthy of clinical promotion.
Acknowledgments
Funding: This work was supported by the National Key Research & Development Program of China (No. 2018YFC2001502, and 2018YFB1105705).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4658/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4658/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4658/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (ethics approval No. [2021]-0162) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Weller I, Wai EK, Jaglal S, et al. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br 2005;87:361-6. [Crossref] [PubMed]
- Li XP, Zhang P, Zhu SW, et al. All-cause mortality risk in aged femoral intertrochanteric fracture patients. J Orthop Surg Res 2021;16:727. [Crossref] [PubMed]
- Dhanwal DK, Dennison EM, Harvey NC, et al. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop 2011;45:15-22. [Crossref] [PubMed]
- Jiang X, Wang Y, Ma X, et al. Proximal Femoral Nail Antirotation Versus Reverse Less Invasive Stabilization System-distal Femur for Treating Proximal Femoral Fractures: A Meta-analysis. Medicine (Baltimore) 2016;95:e3168. [Crossref] [PubMed]
- Šmejkal K, Lochman P, Trlica J, et al. Impaired Healing after Surgery for Femoral Fractures. Acta Chir Orthop Traumatol Cech 2015;82:358-63. [PubMed]
- Kempf I, Grosse A, Beck G. Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg Am 1985;67:709-20. [Crossref] [PubMed]
- Callanan I, Choudhry V, Smith H. Perineal sloughing as a result of pressure necrosis from the traction post during prolonged bilateral femoral nailing. Injury 1994;25:472. [Crossref] [PubMed]
- Zhao K, Zhang J, Li J, et al. Treatment of Unstable Intertrochanteric Fractures with Proximal Femoral Nailing Antirotation: Traction Table or Double Reverse Traction Repositor. J Invest Surg 2021;34:1178-84. [Crossref] [PubMed]
- Zhang R, Yin Y, Li S, et al. Traction table versus double reverse traction repositor in the treatment of femoral shaft fractures. Sci Rep 2018;8:5952. [Crossref] [PubMed]
- Yan M, Kuang L, Ni J, et al. Use of a Double Reverse Traction Repositor versus a Traction Table for the Treatment of Intertrochanteric Femur Fractures: A Comparative Study. Orthop Surg 2021;13:1254-61. [Crossref] [PubMed]
- Lian X, Zhao K, Chen W, et al. Application of a double reverse traction repositor in the retrograde intramedullary nailing of distal femur fractures. J Orthop Surg Res 2021;16:168. [Crossref] [PubMed]
- Wang Z, Zheng Z, Ye P, et al. Treatment of tibial plateau fractures: A comparison of two different operation strategies with medium-term follow up. J Orthop Translat 2022;36:1-7. [Crossref] [PubMed]
- Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 2004;15:897-902. [Crossref] [PubMed]
- Parker MJ, Bowers TR, Pryor GA. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: a randomised trial of 600 fractures. J Bone Joint Surg Br 2012;94:391-7. [Crossref] [PubMed]
- Queally JM, Harris E, Handoll HH, et al. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst Rev 2014;CD004961. [Crossref] [PubMed]
- Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev 2008;CD000093. [PubMed]
- Zhang Y, He W, Liu YW, et al. Comparison of the efftec between eccentric fixation and intramedullary fixation for treatment of intertrochanteric fractures. Zhongguo Gu Shang 2015;28:117-21. [PubMed]
- Jawad MJ. Evaluation of using PFN (proximal femoral nailing) in treatment of unstable intertrochanteric fractures in elderly patients. J Pak Med Assoc 2021;71:S179-84. [PubMed]
- Singh S. Proximal Femoral Nail versus Proximal Femoral Nail Antirotation: Functional and Radiological Outcome in Intertrochanteric Fractures of Femur. Cureus 2021;13:e19093. [Crossref] [PubMed]
- Page PR, Lord R, Jawad A, et al. Changing trends in the management of intertrochanteric hip fractures - A single centre experience. Injury 2016;47:1525-9. [Crossref] [PubMed]
- Sahin S, Ertürer E, Oztürk I, et al. Radiographic and functional results of osteosynthesis using the proximal femoral nail antirotation (PFNA) in the treatment of unstable intertrochanteric femoral fractures. Acta Orthop Traumatol Turc 2010;44:127-34. [Crossref] [PubMed]
- Lenich A, Mayr E, Rüter A, et al. First results with the trochanter fixation nail (TFN): a report on 120 cases. Arch Orthop Trauma Surg 2006;126:706-12. [Crossref] [PubMed]
- Ahn J, Bernstein J. Fractures in brief: intertrochanteric hip fractures. Clin Orthop Relat Res 2010;468:1450-2. [Crossref] [PubMed]
- Cao F, Xue H, Yan C, et al. Clinical Application Study of Minimally Invasive Double-Reverse Traction in Complex Tibial Plateau Fractures. Biomed Res Int 2022;2022:5564604. [Crossref] [PubMed]
(English Language Editor: J. Teoh)




