
Clinical evaluation of corrective effect of infraorbital depression by fat granule auto-transplantation via oral mucosa incision
Introduction
As we age, the skin elasticity and glow decrease due to soft tissue atrophy, fat volume loss, and bone absorption, which are all important causes of facial contour aging (1). In recent years, autologous fat transplantation has been widely used for facial augmentation due to its low immunogenicity, simple operation, low costs, and easy access (2).
Suborbital fat filling is a common procedure to improve suborbital depression, usually with a cutaneous approach or a percutaneous nasolabial approach. If only subcutaneous fat grafting is performed during surgery, local soft tissue sagging will be promoted with the increase of fat grafting, thereby aggravating the formation of nasolabial folds, and the goal of rejuvenation of medium facial lift cannot be obtained. Therefore, the suborbital area is filled with fat, which requires the replenishment of the deep fat chamber, which requires that the injection level through the skin approach needs to reach the superficial layer of the maxillary periosteum. However, due to the skin or nasolabial sulcus approach, the above path may damage the terminal branches of the facial arteries, causing facial vascular damage, and even complications such as fat embolism, so there is a potential safety hazard. Infraorbital fat grafting is not only a supplement to the amount of soft tissue in the middle face, but also a supplement to the deep fat chamber to achieve the purpose of lifting the middle face. Therefore, in order to find a safe level and maintain the lifting effect of the mid-face, a safer and more efficient method of fat filling in the suborbital area based on anatomy is needed. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3872/rc).
Methods
Research subjects
This study comprised 107 patients who visited the plastic surgery department between January 2017 and January 2022. The patients had an age range of 28–50 years, and an average age of 38 years. To be eligible for inclusion in this study, patients had to meet the following inclusion criteria: (I) have depression in the infraorbital area; (II) have facial asymmetry; and (III) have a need for fat transplantation. Patients were excluded from the study if they met any of the following exclusion criteria: (I) had a facial, oral, or systemic skin infection; (II) had a coagulation disorder, or had recently engaged in the prolonged use of oral anticoagulant drugs; (III) had merged vital organs, such as heart, brain, liver, kidney, or other injuries; (IV) had a history of narcotic drug use or allergies; (V) had other serious systemic diseases, such as metabolic and immune system diseases; and/or (VI) had significant cognitive disabilities or mental illness, which made clinical treatment difficult. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Zhongda Hospital (No. 2016ZDKYSB031). All the patients signed the informed consent form.
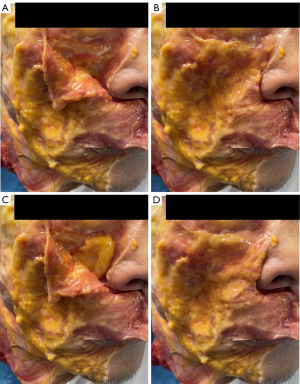
Anatomical study
To further study and clarify the safety of the anatomical level, we searched for fresh cadaver specimens. Imitating the surgical approach, the surgeon made an incision through the lips and cut a local flap along the outside of the nose, deep into the surface of the periosteum. Next, we pull open the soft tissue on the surface of the zygomatic membrane in the suborbital area, exposing the suborbital foramen and the suborbital neurovascular bundle, and a loose soft tissue gap is visible, which is the site of the fat graft in our surgery. There were no obvious nerves and blood vessels on the surface of the periosteum in the intended area, and this layer was conducive to blunt separation (see Figure 1).

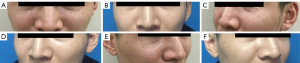
In an anatomical simulation experiment, the surgeon put the cellulite in the area to be transplanted and then repositioned the fascia flap, as the area to be transplanted was locally augmented (see Figure 2), which showed that the oral approach could achieve the effect of the local augmentation of the suborbital area.
Surgical methods
The surgeon marked the range and key parts of the fat grafting area. The surgeon then injected the swelling fluid using a 1.5-mm diameter water injection needle connected to a 50-mL screw-connected syringe until the skin of the donor site had an “orange peel” appearance. Fat was collected by liposuction performed on the abdomen or thigh region using a 16-gauge cannula attached to a 10-mL syringe. The fluid component, which included the oil layer and blood, was drained from the aspirated fat. The remaining tissue was set aside for standby.
After the routine disinfection of the face and oral surgery area, 2% lidocaine (1:200,000 epinephrine) was used to perform the nerve block anesthesia, while the area to be transplanted was simultaneously pre-swollen to prepare for the separation of this area in advance.
After achieving satisfactory anesthesia, a 3-mm incision was made on the reflex of the upper lip and buccal mucosa at the basal side of the alar nose with a puncture needle (see Figure 3A). The injection needle with an inner diameter of 3 mm is connected to a syringe containing 1 mL of normal saline for fat grafting, and then the orbicularis incision is passed through at an angle of 60° to the shallow periosteum, and moved up along the shallow periosteum to the middle facial depression. After aspirating the syringe without active bleeding, the syringe with the prepared fat was connected to the injection needle for fat transplantation and grafting (see Figure 3B). Generally, about 2–3 mL of fat was locally injected. The needle was withdrawn to confirm that there was no obvious bleeding.

To control the possibility of infection, the used injection needles for fat transplantation were discarded, and new injection needles were used for any other parts that need to be transplanted. If necessary, nano fat was used to fill the local soft tissues and tighten the skin. After ensuring that the patient had no uncomfortable reactions, the operation was completed. The oral cavity was cleaned with normal saline after surgery. The patient was deprived of water for 2 hours, fasted for 4 hours, and placed on a liquid diet within 48 hours. The transplanted area was cold-compressed for 48 hours post-operation. Antibiotics were routinely used to prevent infection.
Postoperative evaluation and follow-up
After the operation, we made a comprehensive evaluation of the surgical effect based on the patient’s self-evaluation and the preoperative and postoperative photos. Follow-up lasts from six months to 2 years after surgery to assess whether patients have complications such as skin ulcers, infections, local induration, and fat liquefaction. Six months after surgery, the patient was assessed by using a graded scale, and the assessment record was based on the four levels of very satisfactory, satisfactory, average and dissatisfied with whether the suborbital depression was corrected, whether the mid-facial asymmetry was corrected, whether the nasolabial folds were reduced, and the fat survival status was taken as the evaluation criteria.
Statistical analysis
Postoperative follow-up data were analyzed by Excel 2020.Mean was calculated for continuous variables in normal distribution. For variables in skewed distribution, we calculated their medians. Percentages were calculated for ranked variables.
Results
The efficacy of the operation was evaluated according to self-evaluation assessments by the patients and the comparison of preoperative and postoperative photographs. A total of 107 patients were followed-up for 6–24 months after the surgery, with an average follow-up period of 12 months. The patients were asked to complete a satisfaction evaluation 6 months after the operation. Of the 107 patients, 72 (67.3%) were “very satisfied”, 31 (29.0%) were “satisfied”, 4 (3.7%) were “average”, and no patients were “dissatisfied”. No complications, such as skin ulcer, infection, local induration, or fat liquefaction, were observed. The depression in the infraorbital area disappeared, and a favorable mid-face augmentation effect was achieved.
Typical cases
Case 1
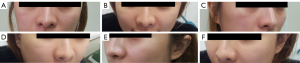
A 34-year-old man presented with depression of the infraorbital area and deformity of the lacrimal groove. The infraorbital area was filled with autologous fat via an oral incision. After 12 months of follow-up, the deformity of the infraorbital area and the lacrimal groove was corrected, and the mid-face augmentation effect was obvious. The skin texture was also improved. The patient was satisfied with the postoperative results (see Figure 4).
Case 2
A 28-year-old woman requested fat grafting to augment her mid-face area and fill the infraorbital area. The 3-month postoperative follow-up examination showed that the mid-face area was significantly augmented, the infraorbital area was plump, and the pigmentation in the suborbital region was improved. The patient was satisfied with the postoperative results (see Figure 5).
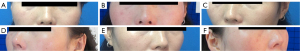
Case 3
A 47-year-old woman requested facial rejuvenation, which was performed with infraorbital fat grafting via oral incision. Preoperatively, this patient demonstrated infraorbital depression and mid-face sagging. Some 6 months after the surgery, the patient achieved a favorable augmentation effect and youthful appearance. The patient was satisfied with the postoperative results (see Figure 6).
Discussion
Fat transplantation, which can achieve the effects of adjusting the proportions of facial contours, restoring tissue volume, and improving skin texture (3-8), is currently a common surgical method in plastic surgery. With the wide application of fat grafting technology in plastic surgery or other specialties, complications, such as edema, infection, hematoma, calcification, granuloma formation, fat necrosis, and vascular embolism (9-12), present significant challenges for plastic surgeons. Thus, the surgical method and approach must be planned according to the patients’ anatomical characteristics to improve surgical results.
Common complications of infraorbital fat transplantation include insufficient volume or an over-correction of volume, local excessive bloating leading to obvious mid-face sagging after transplantation, infection, granuloma and inflammation, vascular embolism with a loss of vision, or cerebral infarction (13-15). In the mid-face, facial arteriovenous terminal branches traverse the muscular fascial system near the side of the nose. Due to the difficulty of precisely controlling the level of transplantation, the filling of subcutaneous soft tissue carries a risk of local soft tissue skin necrosis, fat embolism, and even blindness. Lazzeri et al. (16) reviewed and analyzed the literature on blindness caused by filler injection in 2012. A total of 32 cases were included, of which 15 cases were blinded after facial fat transplantation, none of whom later recovered their vision. Subsequently, other studies have also reported some cases of blindness caused by facial fat transplantation (17-19).
To search for safer and more meaningful surgical methods, the authors simulated the approach of infraorbital fat grafting via oral incision, and conducted the study based on the anatomical characteristics. In the study, fat grafting was performed via an oral incision on the reflex of the upper lip and buccal mucosa at the basal side of the alar nose. The surgical level followed the mucosal, submucosal, upper lip orbicularis muscle, and the upper maxilla bone surface. The study demonstrated that this layer is easy to peel-off, and the preoperative use of swelling fluid made the peeling of the soft tissue more conducive with needles for fat grafting on the surface of the periosteum. The anatomical study revealed that there are no major arteries on the surface of the periosteum at this level, and it naturally exists as an interstice, which makes it easy for soft tissue filling. Additionally, the superficial muscles in the transplanted area are mainly part of the levator labii superioris alaeque nasi muscle, zygomatic minor muscle, and zygomatic major muscle. Fat transplantation in the deep layer of the muscle can achieve an augmentation effect of the muscle fascia system. Thus, we adopted this surgical approach for the infraorbital fat grafting.
In this study, a total of 107 patients who underwent infraorbital fat grafting via oral incision were included. Comparisons of the preoperative and postoperative photographs showed that the depression in the infraorbital area of each patient was filled, and satisfactory surgical results were achieved. No serious complications were observed. During fat transplantation, infection is a common postoperative complication. For the facial lifting, the authors filled the surface of the maxillary periosteum, and used soft tissue as a base to lift the muscular fascia system upwards in the infraorbital area to improve the sagging and enhance the contour of the mid-face to achieve the purpose of facial rejuvenation.
To reduce the possibility of infection and to avoid fat infection at the filling site, which can occur under the oral incision approach, 3% hydrogen peroxide was used to rinse the mouth preoperatively. The operation area was disinfected with iodophor, and antibiotics were used to prevent infection post-operation. During the operation, a separate fat injection needle was used for transplantation. After the fat transplantation using the oral approach was completed, the needle was discarded, and new needles for transplantation were selected for the fat grafting in other parts. In this study, there were no cases of infection after fat transplantation. The analysis showed that the main reason for this was the preoperative and postoperative aseptic conditions and the postoperative prevention of infection. During the operation, only specific needles for transplantation were used for the injections to avoid the mixing of injection needles. These steps provide clinical guidance on how to reduce the infection rate after fat transplantation.
After the fat transplantation via oral incision was completed, if the patient wished to improve the skin texture of the mid-face or fill any small contour, small particles of fat or nano fat were used for supplementary filling. To enhance the survival of the fat in the transplanted area, the fat and the surrounding fascia composite tissue were selected for mixed transplantation. Fat transplantation of different components achieved a similar transplantation effect as dermal transplantation, which has a certain degree of rigidity. Notably, the patients can feel the rigidity of the grafted material in the area 1 month after the transplantation. Moreover, patients who were followed-up for 6 months reported feeling slight rigidity in the transplanted area compared to the non-transplanted area, but the mid-face lifting effect was satisfactory. Thus, this study indicated that composite fascial fat transplantation improves the survival rate of soft tissue transplantation and can be used as an arcuate fulcrum, similar to the accumulation of dermal tissue, to achieve the purpose of improving mid-face soft tissue. These findings are similar to those of Erol et al. (20), who, in 2000, used a mixture of dermal tissue, fat and fascia for the transplantation onto the patient's face. The patient was followed-up for 6 months to 10 years, and satisfactory results were achieved, which showed that the combined transplantation significantly improved the survival rate, and the effect was better than that of fat transplantation alone.
Facial rejuvenation is a complex research topic, and many methods use adipose tissue. This research achieved relatively satisfactory results in these cases. To obtain a more satisfactory and safe effect for fat transplantation, the authors will use fat with different components to fill different regions in future studies, the texture of which will be suitable for each area being transplanted. Further, the authors will collect more cases to analyze the postoperative effect of fat transplantation on a large scale.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-3872/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-3872/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3872/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Zhongda Hospital (No. 2016ZDKYSB031). All the patients signed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Crowley JS, Kream E, Fabi S, et al. Facial Rejuvenation With Fat Grafting and Fillers. Aesthet Surg J 2021;41:S31-8. [Crossref] [PubMed]
- Brooker JE, Rubin JP, Marra KG. The Future of Facial Fat Grafting. J Craniofac Surg 2019;30:644-51. [Crossref] [PubMed]
- Marten T, Elyassnia D. Periorbital Fat Grafting: A New Paradigm for Rejuvenation of the Eyelids. Facial Plast Surg Clin North Am 2021;29:243-73. [Crossref] [PubMed]
- van Dongen JA, Langeveld M, van de Lande LS, et al. The Effects of Facial Lipografting on Skin Quality: A Systematic Review. Plast Reconstr Surg 2019;144:784e-97e. [Crossref] [PubMed]
- Rigotti G, Charles-de-Sá L, Gontijo-de-Amorim NF, et al. Expanded Stem Cells, Stromal-Vascular Fraction, and Platelet-Rich Plasma Enriched Fat: Comparing Results of Different Facial Rejuvenation Approaches in a Clinical Trial. Aesthet Surg J 2016;36:261-70. [Crossref] [PubMed]
- Schultz KP, Raghuram A, Davis MJ, et al. Fat Grafting for Facial Rejuvenation. Semin Plast Surg 2020;34:30-7. [Crossref] [PubMed]
- Trivisonno A, Rossi A, Monti M, et al. Facial skin rejuvenation by autologous dermal microfat transfer in photoaged patients: Clinical evaluation and skin surface digital profilometry analysis. J Plast Reconstr Aesthet Surg 2017;70:1118-28. [Crossref] [PubMed]
- Willemsen JCN, Van Dongen J, Spiekman M, et al. The Addition of Platelet-Rich Plasma to Facial Lipofilling: A Double-Blind, Placebo-Controlled, Randomized Trial. Plast Reconstr Surg 2018;141:331-43. [Crossref] [PubMed]
- Cuzalina A, Guerrero AV. Complications in Fat Grafting. Atlas Oral Maxillofac Surg Clin North Am 2018;26:77-80. [Crossref] [PubMed]
- Gornitsky J, Viezel-Mathieu A, Alnaif N, et al. A systematic review of the effectiveness and complications of fat grafting in the facial region. JPRAS Open 2019;19:87-97. [Crossref] [PubMed]
- Kim IA, Keller G, Groth MJ, et al. The Downside of Fat: Avoiding and Treating Complications. Facial Plast Surg 2016;32:556-9. [Crossref] [PubMed]
- Dhooghe NS, Maes S, Depypere B, et al. Fat Embolism After Autologous Facial Fat Grafting. Aesthet Surg J 2022;42:231-8. [Crossref] [PubMed]
- Boureaux E, Chaput B, Bannani S, et al. Eyelid fat grafting: Indications, operative technique and complications; a systematic review. J Craniomaxillofac Surg 2016;44:374-80. [Crossref] [PubMed]
- Maamari RN, Massry GG, Holds JB. Complications Associated with Fat Grafting to the Lower Eyelid. Facial Plast Surg Clin North Am 2019;27:435-41. [Crossref] [PubMed]
- Yang F, Ji Z, Peng L, et al. Efficacy, safety and complications of autologous fat grafting to the eyelids and periorbital area: A systematic review and meta-analysis. PLoS One 2021;16:e0248505. [Crossref] [PubMed]
- Lazzeri D, Agostini T, Figus M, et al. Blindness following cosmetic injections of the face. Plast Reconstr Surg 2012;129:995-1012. [Crossref] [PubMed]
- Loh KT, Chua JJ, Lee HM, et al. Prevention and management of vision loss relating to facial filler injections. Singapore Med J 2016;57:438-43. [Crossref] [PubMed]
- Prado G, Rodríguez-Feliz J. Ocular Pain and Impending Blindness During Facial Cosmetic Injections: Is Your Office Prepared? Aesthetic Plast Surg 2017;41:199-203. [Crossref] [PubMed]
- Sorensen EP, Council ML. Update in Soft-Tissue Filler-Associated Blindness. Dermatol Surg 2020;46:671-7. [Crossref] [PubMed]
- Erol OO. Facial autologous soft-tissue contouring by adjunction of tissue cocktail injection (micrograft and minigraft mixture of dermis, fascia, and fat). Plast Reconstr Surg 2000;106:1375-87; discussion 1388-9. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


