
Successful management of Stanford type A aortic dissection with severe scoliosis in the setting of Marfan syndrome: a case report
Introduction
Marfan syndrome (MFS) can have adverse effects on a number of body systems, with the cardiovascular and musculoskeletal systems most prominently affected. For those with MFS, acute aortic Stanford type A dissection (AADA) remains a common and potentially fatal occurrence (1). Standard median sternotomy is generally considered the most ideal surgical route for AADA repair. However, for patients suffering from severe thoracic deformity, scoliosis, and other complications, median sternotomy should be avoided as much as possible due to problems with exposure of the surgical field and postoperative lung function (2-4). However, in this patient, attribute to the severity of aortic root and arch dissection as well as aneurysmal dilatation of the aortic sinus, we attempted a median sternotomy with uncertainty and performed Bentall procedure and Sun’s procedure on an MFS patient with severe scoliosis and thoracic deformity. At present, there is no relevant literature report on the effect and degree of severe spinal deformity on the feasibility of median sternotomy and postoperative pulmonary function. Therefore, this report expands the indications for surgical treatment of AADA in this specific patient group. We present the following article in accordance with the CARE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4302/rc).
Case presentation
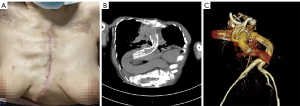
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. A 40-year-old female, under no obvious predisposing cause, suffered abrupt onset of severe pain on the left side of the chest. The ripping pain started 7 hours prior and had not been treated. From that point, the severity of pain persistently failed to be alleviated and pain radiated into the back and shoulder. The patient advised that scoliosis had developed steadily after her birth, that she had no history of hypertension or type 2 diabetes, and that her family had no history of aortic dissection or other genetic diseases. After emergency admission, physical examination revealed a body temperature of 36.5 ℃, heart rate of 65 beats per minute, blood pressure of 135/70 mmHg, respiration rate of 22 breaths per minute, distal blood oxygen saturation of 95%, a diastolic murmur in aortic valve area, increased arm and pectus carinatum deformity, severe scoliosis, acromicria, arachnodactyly, and planovalgus foot (Figure 1). The patient underwent echocardiogram, which revealed AADA, moderate aortic regurgitation, mild tricuspid regurgitation, hydropericardium in small amount, and normal left ventricle ejection fraction (EF) of 69%. In addition, computed tomography (CT) of the thoracoabdominal aorta showed the full extent of the dissection, extending through the ascending aorta and proximal to the innominate artery and the entire thoracoabdominal aorta. At the same time, severely tortuous descending aorta along with severe spinal deformity was also shown in the CT images (Figure 2). Based on revised Ghent criteria, the patient was diagnosed with MFS complicated with aortic dissection, and emergency surgery was planned for repair of acute aortic dissection and the diseased aortic valve.


We chose standard median sternotomy to overcome the anatomical challenge caused by severe tortuosity of the spine and aorta. Through the right atrium and right axillary artery, cardiopulmonary bypass was established. The ascending thoracic aorta was opened to reveal obvious thickened aortic valves, aortic regurgitation, and separation of the intima. A 2-cm intimal tear was located in the left coronary sinus and right coronary sinus near the aortic annulus. The dissection involved the ascending aorta, aortic arch, innominate artery, ostia, and the proximal innominate artery, without coronary ostial lesion or involvement of the left common carotid artery and left subclavian artery. After direct coronary perfusion by cold crystalloid cardioplegia, we performed the Bentall treatment using a 26-mm conduit composite and a 21-mm mechanical aortic valve (St. Jude Medical, Inc., St Paul, MN, USA). The diseased artery was then replaced with a 26-mm trifurcated graft. During descending aorta repair using a 26-mm CRONUS stent-graft and anastomosis between the distal end of the trifurcated graft and proximal descending aorta, we used deep hypothermia (24 ℃) circulatory arrest (DHCA) and selective cerebral perfusion via the left common carotid artery, which was followed by anastomosis of every side branch of the trifurcated graft during rewarming. Unsurprisingly, the left subclavian artery in the patient was located at a deep tissue level, and thus we adopted left axillary artery bypass. The branch of the left subclavian artery corresponding to the trifurcated graft was submerged at the level of the first intercostal space below the sternum and pulled to the level of the left axillary artery. Atrial appendage forceps clamped the position of anastomosis before left axillary artery angiotomy and removing part of the vessel wall. The branch anastomosis was then end-to-end at the distal end. Total cardiopulmonary bypass and aortic cross-clamping times were 320 and 175 minutes, respectively. Postoperative longtime mechanical ventilatory support was applied to promote the recovery of respiratory function. Before the patient’s recovery, we strictly monitored her respiratory function, pulmonary complications, and bleeding with neurologic events. Three weeks after admission, the patient was discharged home without any adverse events. The entire course of the disease is briefly depicted in the timeline figure (Figure 3).
Discussion
MFS, an autosomal dominant inherited connective tissue disease, is brought on by FBN1 mutations and affects multiple organs and systems (5). The most serious appearance of MFS is thoracic aortic aneurysm (TAA), which can progress to AADA (6). Scoliosis, as a main type of spinal deformity, is one of the most common musculoskeletal manifestations of MFS (7). However, AADA associated with spinal deformity is unusual in MFS patients. Because of pain and restrictive ventilatory disturbance in patients as a result of spinal deformity, patients with MFS may be at an increased risk of additional cardiopulmonary damage while undergoing a thoracotomy or having repeated pneumothoraxes (8). Moreover, severe spinal deformity affects surgical intervention, aortic surgery in these patients is challenging. A good surgical approach can fully expose the surgical field and facilitate operation of the aorta. For this patient’s surgery, we chose standard median sternotomy and demonstrated that the surgical approach was still feasible (including being able to maintain the supine position during the operation). This degree of tortuosity of the aorta, in addition to the significant shift in the mediastinum due to scoliosis, is extremely rare and contributes to many operational challenges during surgery. Because the aorta is at a very deep level in the mediastinum and very close to the spine, it is easy to damage surrounding tissues involving the thoracic duct, recurrent laryngeal nerve, and pleura, in addition to the spine, during the operation. Properly expanding the median sternotomy combined with a rotating surgical platform can resolve the problem of difficult exposure of the surgical field so that the ascending aorta and arch vessels are obtained as in a typical cardiac operation. However, the branch of the left subclavian artery corresponding to the trifurcated graft is difficult to anastomose so we used axillary artery bypass. The branch was submerged at the level of the first intercostal space below the sternum and pulled to the level of the left axillary artery, while a small incision was made under the left clavicle for anastomosis of the axillary artery. Furthermore, in this patient, the aorta was twisted and formed multiple acute angles at the distal end of the descending aorta. Therefore, the distance from the descending aorta to the first tortuous acute angle at the distal end should be accurately evaluated before surgery to avoid hostile angulation between the stent-graft and tortuous artery. The stent-graft was positioned away from the distal end to avoid hostile angulation, preventing stenosis or blockage of distal blood vessels (Figure 4).
The adverse effects of spinal malformation on pulmonary function have a well-established correlation. Demonstrably, increased thoracic scoliosis as well as hypokyphosis and pulmonary impairment have been correlated in several investigations of adolescents with idiopathic scoliosis (9-11). There have been reports of both a restrictive and obstructive pulmonary pattern in individuals with spinal distortion. Diminished chest wall compliance, diminished rib excursion, potential diminished respiratory strength, and the resultant mechanical disadvantage of the diaphragm for inspiration and expiration are all probable causes of the restrictive pulmonary pattern. Some theories speculate that the obstructive pulmonary pattern may develop as a result of increased airway smooth muscle tone, variation asthma, lower airway malacia, or intrathoracic airway compression owing to chest wall deformity. As mentioned above, due to the deformity of the spine, postoperative pain in such patients is also more obvious and severe, which makes them reluctant to breathe fully and cough with expectoration. The aforementioned is accurate of the patient in this case. The patient experienced repetitive respiratory muscle weakness and quick shallow breathing after extubation, bringing about a low flow volume, followed by mild carbon dioxide retention and mild hypercapnia without hypoxemia. Therefore, the patient first required noninvasive ventilator-assisted for a longer period of time under the condition of analgesia to improve breathing weakness. Meanwhile, we encouraged the patient to take deep breaths and cough fully under the application of a vibration sputum excretion instrument and chest percussion techniques. In addition, she was given a fiberoptic bronchoscopy for sputum suction every other day, in addition to early ambulation and exercise at least half an hour a day, which can also strengthen the functions of multiple system. As these measures are also mentioned in the existing literature, early training programs may be advantageous in the short- and long-term postoperative stages, and respiratory physiotherapy may help avoid respiratory infections (12). The exercise included treadmill exercise, which facilitated the performance of breath actions (13) and may increase mucus clearance and achieve reductions in sputum mechanical impedance (14). Hence, early active sputum suction by fiberoptic bronchoscope, physical respiratory function exercise, and effective analgesia can reduce respiratory complications and help patients restore respiratory function as soon as possible.
Conclusions
The results of this case indicated that sternotomy might not necessarily be a contraindication to surgery to treat aortic dissection associated with scoliosis. The patient had a good prognosis after surgical treatment, and respiratory function was not greatly damaged under good intervention, although the surgery tests the surgeon’s abilities.
Acknowledgments
We would like to thank the medical imaging, pathology, and anesthesia departments of our hospital for their support.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4302/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4302/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Murdoch JL, Walker BA, Halpern BL, et al. Life expectancy and causes of death in the Marfan syndrome. N Engl J Med 1972;286:804-8. [Crossref] [PubMed]
- Okamoto Y, Harada Y, Uchita S. Fontan operation through a right lateral thoracotomy to treat Cantrell syndrome with severe ectopia cordis. Interact Cardiovasc Thorac Surg 2008;7:278-9. [Crossref] [PubMed]
- Kitamura T, Edwards J, Stuklis RG, et al. Minimally invasive mitral valve replacement in a patient with previous omphalocele repair and severe scoliosis. Gen Thorac Cardiovasc Surg 2011;59:117-9. [Crossref] [PubMed]
- Pau CP, Chong KS, Yakub MA, et al. Single-stage open repair of severe asymmetric pectus excavatum and mitral valve replacement in connective tissue disease. Asian Cardiovasc Thorac Ann 2022;30:480-2. [Crossref] [PubMed]
- Patel HJ, Deeb GM. Ascending and arch aorta: pathology, natural history, and treatment. Circulation 2008;118:188-95. [Crossref] [PubMed]
- Milewicz DM, Ramirez F. Therapies for Thoracic Aortic Aneurysms and Acute Aortic Dissections. Arterioscler Thromb Vasc Biol 2019;39:126-36. [Crossref] [PubMed]
- Pyeritz RE, Francke U. The Second International Symposium on the Marfan Syndrome. Am J Med Genet 1993;47:127-35. [Crossref] [PubMed]
- Taniguchi Y, Takeda N, Inuzuka R, et al. Impact of pathogenic FBN1 variant types on the development of severe scoliosis in patients with Marfan syndrome. J Med Genet 2021; Epub ahead of print. [Crossref] [PubMed]
- Upadhyay SS, Mullaji AB, Luk KD, et al. Relation of spinal and thoracic cage deformities and their flexibilities with altered pulmonary functions in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:2415-20. [Crossref] [PubMed]
- Yaszay B, Bastrom TP, Bartley CE, et al. The effects of the three-dimensional deformity of adolescent idiopathic scoliosis on pulmonary function. Eur Spine J 2017;26:1658-64. [Crossref] [PubMed]
- McPhail GL, Ehsan Z, Howells SA, et al. Obstructive lung disease in children with idiopathic scoliosis. J Pediatr 2015;166:1018-21. [Crossref] [PubMed]
- Kourek C, Karatzanos E, Nanas S, et al. Exercise training in heart transplantation. World J Transplant 2021;11:466-79. [Crossref] [PubMed]
- Santamato A, Ranieri M, Panza F, et al. Pulmonary rehabilitation for patients with bronchiectasis: case reports. Eur J Phys Rehabil Med 2012;48:293-8. [PubMed]
- Dwyer TJ, Alison JA, McKeough ZJ, et al. Effects of exercise on respiratory flow and sputum properties in patients with cystic fibrosis. Chest 2011;139:870-7. [Crossref] [PubMed]



