Isolated polycystic liver disease and aneurism: a case report
Introduction
It is known that autosomal dominant polycystic kidney disease (ADPKD) and polycystic liver disease (PCLD) follow an autosomal dominant pattern of inheritance, and cerebral vascular manifestations have been described as occasional part of the disease spectrum (1). Furthermore, cerebral aneurysms are suggested to be part of the spectrum of PCLD (2). Based on the mutation load there are different appearances of the disease in different vessels. In patients with multiple liver and/or kidney cysts and a history of headache, subarachnoidal hemorrhage as well as carotid dissection must be considered. We present a case with aneurism due to PCLD. Previous publications support the screening of these patients for cerebral and intracranial aneurisms (2,3).
Case presentation
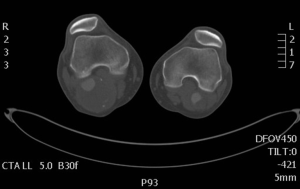
In January 2011 a 51-year-old man presented with a painful, pulsating right popliteal mass with no history of trauma. There was nothing else of significance in his family or past medical history apart from pharmaceutically controlled hypertension. The patient was unusually tall for Greek circumstances but no high arched palate, no pectus excavatum and no joint laxity. Clinical examination showed bilateral pulsating popliteal swellings and a left sided inguinal hernia. A computed tomogram with contrast confirmed bilateral partially thrombosed popliteal aneurysms (right 5.2×6 cm2 and left 2.6×2.5 cm2) (Figures 1,2) with PCLD, right common iliac and common femoral artery dilatation but no atherosclerotic disease or aortic aneurysmal changes. The patient underwent successful urgent femoro-popliteal bypass with vein graft and ligation of the aneurysm initially on the right followed by the same procedure on the left two months later. Histological evaluation of arterial sample did not reveal any signs of vasculitis or possible connective tissue disorder.
Discussion
PCLD is an assortment of rare human disorders and more particularly is an inherited Mendelian disorder (4,5). These disorders are results from structural changes of the biliary tree development and (6) also consist a group of genetic disorders that initiated by mutations in many related genes of PLD and characterized by the development of multiple cholangiocyte derived hepatic cysts that with time replace liver tissue (7,8). Current medical therapies for PLD include symptomatic management (9) and surgical interventions (10).
In our case report the patient unusually diagnosed also with bilateral popliteal artery aneurysm (PAA). The PAA is the commonest peripheral aneurysm which presenting bilaterally in 50% of cases. It is noticeable that 80% of the patients are asymptomatic when diagnosed with PAP, and as follows from the literature, at a rate of 14% per year, these patients become symptomatic (11,12). Best results demonstrated and the complications minimized when the treatment is given before symptoms onset (13). The treatment of choice includes surgical techniques and endovascular interventions, as in our case, where the patient submitted successfully in femoro-popliteal bypass with vein graft and ligation of the aneurysm (14,15).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Neumann HP, Malinoc A, Bacher J, et al. Characteristics of intracranial aneurysms in the else kröner-fresenius registry of autosomal dominant polycystic kidney disease. Cerebrovasc Dis Extra 2012;2:71-9. [Crossref] [PubMed]
- Geevarghese SK, Powers T, Marsh JW, et al. Screening for cerebral aneurysm in patients with polycystic liver disease. South Med J 1999;92:1167-70. [Crossref] [PubMed]
- Schievink WI, Spetzler RF. Screening for intracranial aneurysms in patients with isolated polycystic liver disease. J Neurosurg 1998;89:719-21. [Crossref] [PubMed]
- Roskams T, Desmet V. Embryology of extra- and intrahepatic bile ducts, the ductal plate. Anat Rec (Hoboken) 2008;291:628-35. [Crossref] [PubMed]
- Raynaud P, Carpentier R, Antoniou A, et al. Biliary differentiation and bile duct morphogenesis in development and disease. Int J Biochem Cell Biol 2011;43:245-56. [Crossref] [PubMed]
- Arrazola L, Moonka D, Gish RG, et al. Model for end-stage liver disease (MELD) exception for polycystic liver disease. Liver Transpl 2006;12:S110-1. [Crossref] [PubMed]
- Desmet VJ. Ludwig symposium on biliary disorders--part I. Pathogenesis of ductal plate abnormalities. Mayo Clin Proc 1998;73:80-9. [Crossref] [PubMed]
- Masyuk TV, Masyuk AI, La Russo NF. Therapeutic Targets In Polycystic Liver Disease. Curr Drug Targets 2015. [Epub ahead of print]. [PubMed]
- Everson GT, Taylor MR. Management of polycystic liver disease. Curr Gastroenterol Rep 2005;7:19-25. [Crossref] [PubMed]
- Drenth JP, Chrispijn M, Nagorney DM, et al. Medical and surgical treatment options for polycystic liver disease. Hepatology 2010;52:2223-30. [Crossref] [PubMed]
- Jung DH, Hwang S, Ahn CS, et al. Fenestration of liver cysts in polycystic liver disease to improve quality of life: a case report and literature review. Korean J Hepatobiliary Pancreat Surg 2015;19:40-6. [Crossref] [PubMed]
- Antonello M, Frigatti P, Battocchio P, et al. Endovascular treatment of asymptomatic popliteal aneurysms: 8-year concurrent comparison with open repair. J Cardiovasc Surg (Torino) 2007;48:267-74. [PubMed]
- Dubuis C, Déglise S, Saucy F, et al. Popliteal artery aneurysms: management in 2013. Rev Med Suisse 2013;9:1299-300, 1302-4. [PubMed]
- Ghotbi R, Deilmann K. Popliteal artery aneurysm: surgical and endovascular therapy. Chirurg 2013;84:243-54. [Crossref] [PubMed]
- Ravn H, Bergqvist D, Björck M, et al. Nationwide study of the outcome of popliteal artery aneurysms treated surgically. Br J Surg 2007;94:970-7. [Crossref] [PubMed]