
Difficult airway management: is prevent by using routine videolaryngoscopy better than cure?
Summary of recommendations
Difficult airway, whether anticipated or not, is one of the most fearful events for anesthesiologists, as it can be associated with life-threatening complications. The most severe complications are neurological injuries or death (1), and their rate remain constant across the last 30 years, mostly associated with judgment errors or inadequate airway planning (1). Airway management has evolved a lot during these past ten years, and until recently last American recommendations were provided in 2013 (2).
New practice recommendations for managing the difficult airway were published in 2022 by the American Society of Anesthesiologists (3). The experts advised limiting the number of attempts at tracheal intubation or supraglottic airway placement in cases of predicted difficult airway management or unplanned and emergency difficult airway management to prevent potential harm and consequences (3). They also underlined the need to be aware of the passage of time, the number of attempts, and oxygen saturation (3). These points can mostly be achieved using videolaryngoscopes, when utilized in expert hands. The expertise and experience are important to allow the optimal use of videolaryngoscopes (4), and that is probably the reason why no recommendation was clearly made on the need to use videolaryngoscopes for first-attempt intubation, in both anticipated and unanticipated management of difficult airway. In the text of the American guidelines (3), The authors stressed that improved laryngeal views, a higher frequency of successful intubations, a higher frequency of successful first attempt intubations, and fewer intubation maneuvers were all seen with videolaryngoscopy compared to direct laryngoscopy in patients with predicted difficult airways. The results for the time to intubation were equivocal. This equivoque could also be due to the wide variability of experience of operators across studies.
Role of videolaryngoscopy
However, difficult and unsuccessful intubation rates by skilled providers drastically decreased after widespread adoption of videolaryngoscopy in operating rooms (5). Despite these evidence, similarly to the recent American guidelines (3), the last French guidelines (6) did not advise to use videolaryngoscopes in operating room as a first-attempt device, excepted during the coronavirus disease 2019 (COVID)-19 pandemic (7). Airway management is at risk for the intubation provider when a patient is infected (8), via the aerosolization of small particles containing the virus. In the French guidelines (7), it was advised to intubate the patient by the most experienced senior using a videolaryngoscope. Similar guidelines were produced in India (9), where it is stated that tracheal intubation with a videolaryngoscope is preferred for higher first-attempt success rate, and in guidelines from United Kingdom (10), where it is recommended for individuals trained in its use to utilize a videolaryngoscope with a separate screen to allow the operator to remain further away from the airway. When using a Macintosh laryngoscope for tracheal intubation, the intubation provider’s face is very close to the patient, increasing the danger of airway secretion contamination for the operator compared to when using a videolaryngoscope. The airway provider is farthest from the mouth of the patient, and therefore less exposed to airway secretions when using a videolaryngoscope. In this pandemic context, it seems no longer acceptable to perform intubation using “old” Macintosh Laryngoscope (11). It is important to remember that mastery of the videolaryngoscope is unlikely to be attained if its use is restricted to expected or unexpectedly difficult intubations. In this setting, United Kingdom hospitals were the first to report using videolaryngoscopy as a first-choice option for all anesthesia and intensive care unit procedures (12), with a nonangulated videolaryngoscope.
As clearly stated by the recent American guidelines (3), when compared to nonangulated videolaryngoscopes for expected difficult airways, randomized controlled trials found no significant differences in laryngoscopic view, intubation success, first attempt intubation success, or time to intubation with hyperangulated videolaryngoscopes. Nonangulated videolaryngoscopes, also called “Macintosh videolaryngoscopes”, present the advantages to allow both direct and indirect laryngoscopy (13). It is worth noting that operators are reluctant to give up direct laryngoscopy, that can be needed when videolaryngoscopes are not available or the operator is not experienced (14). For performing direct laryngoscopy, Macintosh standard laryngoscope remains the first choice for most anesthesiologists (15,16), and this important point could explain why the American guidelines could not clearly advice the use of videolaryngoscopes as preferred difficult airway device in case of unanticipated or anticipated difficult airway (3). However, direct laryngoscopy is not a synonym of Macintosh laryngoscopy. Nonangulated videolaryngoscopes (17,18) allow to perform both direct and indirect laryngoscopy, even if these devices are mostly used as indirect laryngoscopes, probably because of lack of scientific evidence regarding their use as direct laryngoscopes. To our knowledge, no data are reported throughout the literature regarding the glottis view by direct laryngoscopy with the nonangulated videolaryngoscope compared to the glottis view obtained with the Macintosh standard laryngoscope.
Which glottic view with nonangulated videolaryngoscopes?
We present a secondary analysis of an institutional assessment of airway management which evaluated four Single-Use nonangulated videolaryngoscopes with Macintosh similar blades [the McGrath Mac© (Medtronic Covidien, USA), the C-MAC-S© (Karl Storz, Germany), the C-MAC-S Pocket Monitor© (PM) (Karl Storz, Germany) and the APA™© (Advanced Airway Management Health Care, UK)], and the Macintosh standard laryngoscope (13). Approval was obtained from the ethics committee (Institutional Review Board, Comité Locale d’Ethique Recherche, agreement number: 2017_CLER-MPT_11-04) of Montpellier University Hospital. The institutional review board waived the requirement for written informed consent. We aimed to compare the proportion of Cormack-Lehane III and IV scores by direct laryngoscopy with the nonangulated videolaryngoscope and by direct laryngoscopy with the Macintosh standard laryngoscope. The main hypothesis was that the proportion of Cormack-Lehane III and IV scores obtained in direct laryngoscopy may differ between some nonangulated videolaryngoscopes and Macintosh laryngoscope. For each patient assessed, two direct laryngoscopies were performed: a first one with the Macintosh laryngoscope, and a second one with one of the four nonangulated videolaryngoscopes, separately assessed in a randomized order in the four anesthesia departments of the Montpellier University Hospital. For each direct laryngoscopy, the proportion of Cormack-Lehane III and IV scores was assessed using the Cormack-Lehane scoring system. The primary outcome was the proportion of Cormack-Lehane III and IV scores (19). We used this primary outcome as we considered the Cormack-Lehane scores during laryngoscopy was a reproductible and a simple surrogate of the quality of the glottis view. The primary outcome was compared between paired direct laryngoscopies (one with the nonangulated videolaryngoscope and one with the Macintosh laryngoscope) using a Mac Nemar test. From May 2017 to September 2017, 589 patients were included: 180 in the McGrath Mac© group, 132 in the C-MAC S© group, 139 in the C-MAC S© PM group and 138 in the APA™© group. In the McGrath Mac© and the C-MAC-S-PM© groups, the proportion of Cormack-Lehane III and IV scores was similar between nonangulated videolaryngoscopes used as direct laryngoscopes (respectively 20% and 27%) and Macintosh laryngoscopes (respectively 22% and 22%, Figure 1). However, in the C-MAC-S©, and the APA™© groups, the proportion of Cormack-Lehane III and IV scores was greater with the nonangulated videolaryngoscopes used as direct laryngoscopes (respectively 38% and 29%) than with the Macintosh laryngoscope (respectively 28% and 17%).
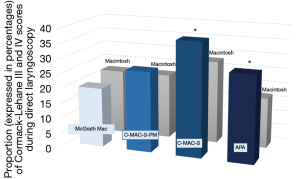
We showed in this institutional quality improvement project that two nonangulated videolaryngoscopes (the McGrath Mac© and the C-MAC-S-PM©) used as direct laryngoscopes provided similar percentages of Cormack-Lehane III and IV scores than the Macintosh laryngoscope.
To our knowledge, this is the first time that the proportion of Cormack-Lehane III and IV scores using direct laryngoscopy with Macintosh standard laryngoscope is compared with the proportion of Cormack-Lehane III and IV scores using direct laryngoscopy with the nonangulated videolaryngoscope.
This result is especially important in order to increase the use of videolaryngoscope worldwide, which seems mandatory in this pandemic period (11). Allowing a direct laryngoscopy using a nonangulated videolaryngoscope with similar performances than a Macintosh standard laryngoscope may increase the team acceptance and diffusion in different settings of videolaryngoscope use for first-attempt intubation.
The nonangulated videolaryngoscope has the advantage to be able to perform a very rapid switch between direct laryngoscopy and videolaryngoscopy, if the direct laryngoscopy was unanticipatedly difficult. Moreover, nonangulated videolaryngoscopes used as direct laryngoscopes could allow the senior anesthesiologist to better guide the anesthesiologist in training and consequently shorten the learning time of direct laryngoscopy.
A pathway to universal videolaryngoscopy
These results complete recent findings of our team (20). Comparing the use of the nonangulated videolaryngoscope to the traditional Macintosh laryngoscope, we demonstrated that employing the nonangulated videolaryngoscope as a first-intention instrument for tracheal intubation increased the proportion of easy airways significantly (20), using a quality improvement project performed in 26,692 tracheal intubation procedures. An “easy airway”, the opposite of “difficult airway”, identified in the last American guidelines (3), was defined as a Cormack and Lehane grades of I or II (absence of difficult laryngoscopy), the absence of difficult mask ventilation and the absence of resort to a rescue technique for intubation (absence of difficult intubation). Additionally, the rise in the percentage of easy airway was linked to less utilization of rescue techniques such using a long intubating stylet or a hyperangulated blade. Operator-reported difficult intubation was also reduced using nonangulated videolaryngoscope as a first-intention device for tracheal intubation. Following these encouraging results, we can suggest that the preferred devices for both anticipated and unanticipated difficult airway management may be videolaryngoscopes. Videolaryngoscopes make it possible to decrease the incidence of unexpectedly unsuccessful intubations, especially in patients who present with an unexpectedly difficult airway (21). They also allow to improve glottis view and to perform intubation under visual control of the larynx, leading to fewer esophageal intubations (22). However, some operators are still reluctant to use videolaryngoscopes as a first-attempt device, and remains faithful to the “Old” Macintosh laryngoscopes. A randomized trial showed that expertise with direct laryngoscopy does not translate to expertise with videolaryngoscope (23). If we keep using the videolaryngoscopes only for difficult intubation, the time to obtain expertise will be higher, and the videolaryngoscope less easily adopted, leading to more unanticipated difficult intubation and associated morbidity and mortality (1). Using widely the videolaryngoscope in non-urgent conditions, for all intubations, including easy intubation, will allow all the operators to be comfortable with the technique. When the videolaryngoscope was used in routine for all first-attempt intubation procedures, it was reported that the videolaryngoscope was largely adopted by all the operators, even the most reluctant at the beginning (12). In the Montpellier experience (13,20), after using routinely videolaryngoscopes, the cost of intubation was very close to the cost of intubation before using routine videolaryngoscopes, taking into account the savings related to the reduced use of long stylet and hyperangulated blades (20), even if no formal medico-economic evaluation was performed. The time for adoption includes the time for formation, the time for acceptation and the time for resistance to change. For adopting universal videolaryngoscopy smoothly, the use of nonangulated videolaryngoscopes present the advantage to allow both direct and indirect laryngoscopy. Formation to direct laryngoscopy for the youngest generations can still be ensured, as conservation of expertise in direct laryngoscopy for the oldest ones. One can make calls and send texts using both a mobile phone and a smartphone. Mobile phones often stop there as well, but some have cameras. A smartphone offers a ton of added features, like a camera, the ability to download apps, and Internet connectivity. Nowadays, the smartphone became a basic need for everyone. Similarly, a Macintosh laryngoscope would do the job for intubation. As smartphones, one of the things that make videolaryngoscopes so vital to our daily lives of anesthesiologists is their efficiency. As said Benjamin Franklin, “without continual growth and progress, such words as improvement, achievement, and success have no meaning.”
Acknowledgments
We thank Christine Faure Chazelles and her team for their help within the devices for anesthesia of Montpellier University Hospital.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Translational Medicine. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3883/coif). SJ reports receiving consulting fees from Drager, Medtronic, Mindray, Fresenius, Baxter, and Fisher & Paykel. ADJ reports receiving remuneration for presentations from Medtronic, Drager and Fisher & Paykel. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Approval was obtained from the ethics committee (Institutional Review Board, Comité Locale d’Ethique Recherche, agreement number: 2017_CLER-MPT_11-04) of Montpellier University Hospital. The institutional review board waived the requirement for written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Joffe AM, Aziz MF, Posner KL, et al. Management of Difficult Tracheal Intubation: A Closed Claims Analysis. Anesthesiology 2019;131:818-29. [Crossref] [PubMed]
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013;118:251-70. [Crossref] [PubMed]
- Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022;136:31-81. [Crossref] [PubMed]
- Cortellazzi P, Caldiroli D, Byrne A, et al. Defining and developing expertise in tracheal intubation using a GlideScope(®) for anaesthetists with expertise in Macintosh direct laryngoscopy: an in-vivo longitudinal study. Anaesthesia 2015;70:290-5. [Crossref] [PubMed]
- Cook F, Lobo D, Martin M, et al. Prospective validation of a new airway management algorithm and predictive features of intubation difficulty. Br J Anaesth 2019;122:245-54. [Crossref] [PubMed]
- Langeron O, Bourgain JL, Francon D, et al. Difficult intubation and extubation in adult anaesthesia. Anaesth Crit Care Pain Med 2018;37:639-51. [Crossref] [PubMed]
- Velly L, Gayat E, Quintard H, et al. Guidelines: Anaesthesia in the context of COVID-19 pandemic. Anaesth Crit Care Pain Med 2020;39:395-415. [Crossref] [PubMed]
- Cheung JC, Ho LT, Cheng JV, et al. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med 2020;8:e19. [Crossref] [PubMed]
- Patwa A, Shah A, Garg R, et al. All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID-19 pandemic. Indian J Anaesth 2020;64:S107-15. [Crossref] [PubMed]
- Cook TM, El-Boghdadly K, McGuire B, et al. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020;75:785-99. [Crossref] [PubMed]
- De Jong A, Pardo E, Rolle A, et al. Airway management for COVID-19: a move towards universal videolaryngoscope? Lancet Respir Med 2020;8:555. [Crossref] [PubMed]
- Cook TM, Boniface NJ, Seller C, et al. Universal videolaryngoscopy: a structured approach to conversion to videolaryngoscopy for all intubations in an anaesthetic and intensive care department. Br J Anaesth 2018;120:173-80. [Crossref] [PubMed]
- De Jong A, Pouzeratte Y, Laplace A, et al. Macintosh Videolaryngoscope for Intubation in the Operating Room: A Comparative Quality Improvement Project. Anesth Analg 2021;132:524-35. [Crossref] [PubMed]
- Jaber S, De Jong A, Pelosi P, et al. Videolaryngoscopy in critically ill patients. Crit Care 2019;23:221. [Crossref] [PubMed]
- Schroeder RA, Pollard R, Dhakal I, et al. Temporal Trends in Difficult and Failed Tracheal Intubation in a Regional Community Anesthetic Practice. Anesthesiology 2018;128:502-10. [Crossref] [PubMed]
- De Jong A, Molinari N, Pouzeratte Y, et al. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. Br J Anaesth 2015;114:297-306. [Crossref] [PubMed]
- De Jong A, Clavieras N, Conseil M, et al. Implementation of a combo videolaryngoscope for intubation in critically ill patients: a before-after comparative study. Intensive Care Med 2013;39:2144-52. [Crossref] [PubMed]
- De Jong A, Molinari N, Conseil M, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: a systematic review and meta-analysis. Intensive Care Med 2014;40:629-39. [Crossref] [PubMed]
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984;39:1105-11. [Crossref] [PubMed]
- De Jong A, Sfara T, Pouzeratte Y, et al. Videolaryngoscopy as a first-intention technique for tracheal intubation in unselected surgical patients: a before and after observational study. Br J Anaesth 2022;129:624-34. [Crossref] [PubMed]
- Hansel J, Rogers AM, Lewis SR, et al. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev 2022;4:CD011136. [PubMed]
- Myatra SN, Patwa A, Divatia JV. Videolaryngoscopy for all intubations: Is direct laryngoscopy obsolete? Indian J Anaesth 2022;66:169-73. [Crossref] [PubMed]
- Bakshi SG, Vanjari VS, Divatia JV. A prospective, randomised, clinical study to compare the use of McGrath(®), Truview(®) and Macintosh laryngoscopes for endotracheal intubation by novice and experienced Anaesthesiologists. Indian J Anaesth 2015;59:421-7. [Crossref] [PubMed]


