
Learning curve for laparoendoscopic single-site radical hysterectomy using the “chopstick” technique: a retrospective cohort study
Introduction
Laparoendoscopic single-site surgery (LESS), which is an optimized form of laparoscopic surgery designed to further minimize surgical invasiveness, has developed rapidly in the field of gynecological surgery, and has even affected surgeries in the gynecological oncology field, including staging surgery for endometrial and ovarian cancer and LESS-radical hysterectomy (LESS-RH) (1-4). The “chopstick” effect, which occurs when all instruments in the umbilicus are arranged in parallel, creates a hindrance in delicate operations (5). To address this issue, researchers have proposed an ingenious approach based on physics that was inspired by the Asian use of chopsticks. To process delicate operations more efficiently, this approach uses the technique to change the instruments’ fulcrum numbers in LESS from single to double and operate the instruments following a chopstick-style movement (6). Named the “chopstick” technique, this technique has been used in the treatment of cervical cancer and endometrial carcinoma thus far, and its feasibility and safety have been confirmed in our previous study (6). On the other hand, the operability and practicability of “chopstick” technique were further recognized in our clinical practice, shown as making LESS convenient and improving surgical efficiency.
As a new technology in its initial application, assessment of its operability and practicability is very important, determining whether the technology can be popularized. Research on the learning curve is helpful in not only demonstrating the stable technical level interval, but also contributing to building a training program. In this retrospective study, we used the cumulative summation (CUSUM) method to generate a learning curve for LESS-RH in early cervical cancer patients and analyzed the demographic data and perioperative outcomes for different phases of the curve. The use of the new technique in LESS-RH, which is considered one of the most complex surgeries in gynecology, could increase its practicability to show its learning cycle. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4447/rc).
Methods
In this retrospective study, we included the clinical data of 44 patients who underwent LESS-RH for early-stage cervical cancer at a single medical center from November 2016 to September 2018. The eligible female patients were aged 18 years or older, and had been pathologically diagnosed with adenocarcinoma, squamous carcinoma, or adenosquamous carcinoma, categorized as Federation International of Gynecology and Obstetrics (FIGO 2014) stage Ia1 disease with stage Ib1 and IIa2 lymphovascular space invasion (LVSI). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was reviewed and approved by the Ethics Committee of First Affiliated Hospital, Army Medical University, PLA (No. KY2020025). Individual consent for this retrospective analysis was waived. All the methods were performed in accordance with the relevant guidelines and regulations. All the procedures were performed by a single chief surgeon (Yanzhou Wang) who has performed a high-volume of laparoscopic gynecologic oncology surgeries. The surgical team included 2 assistants, including a camera assistant and a uterine manipulator assistant, who had extensive experience in performing operations.
Data related to patient characteristics [e.g., age, parity, and body mass index (BMI)] and perioperative parameters, including operation time (OT), estimated blood loss, the number of retrieved lymph nodes, the length of hospital stay, and perioperative complications, were retrospectively extracted from the electronic medical records. The OT was defined as the time from the moment of the first skin incision to the moment of the last port site skin closure. Postoperative complications were defined as postoperative events above grade III according to the Clavien-Dindo classification (7) which took place within 8 weeks post operation.
After surgery, patients with 2 or more intermediate-risk factors (LVSI, tumors >4 cm, and deep cervical stromal invasion) were advised to undergo adjuvant radiation therapy, while patients with 1 or more high-risk factors (resection margin, parametrial, or lymph node involvement) were advised to undergo adjuvant concurrent chemoradiation therapy. After treatment, the patients were examined every 3 months for the first 2 years, then every 6 months for the next 3 years, and once per year thereafter.
Surgical details of the “chopstick” technique
The “chopstick” technique (6) consists of the following 3 parts:
- The establishment of a single-site surgical platform. A key point in establishing a surgical platform is formatting 2 or more separate channels through the umbilicus. This can be achieved via the means of multiple punctures in the rectus sheath or the use of a medium-soft, multichannel-tipped port.
- The arrangement of instruments. After placing 2 separate channels symmetrically to the left and right of the navel, 2 instruments are inserted into the abdominal cavity through these channels, and a 10-mm laparoscope is inserted at the upper part of the incision between these 2 channels.
- The operative procedure. As the 2 separate channels of the medium-soft port provide a double fulcrum for the forceps, the chief surgeon must stand on the cephalic side of the patient to keep his or her arm parallel to the forceps during the operation.
All the patients underwent Type C (Querleu and Morrow’s grading) RH and pelvic lymph node dissection. If the imaging showed that the abdominal para-aortic lymph nodes were enlarged, the abdominal para-aortic lymph nodes were removed. A uterine manipulator without a cup was used to manipulate the uterus to reduce the compression by the cervical tumor. Annular disconnection of the vagina was carried out through vaginal surgery to prevent cervical cancer tissue from entering the abdominal cavity.
Statistical analysis
The learning curve was evaluated using the CUSUM method (8). OT was set as the surrogate marker for surgical competency as in previous studies (9). The CUSUM method was used to calculate the total difference between the individual values and the mean of all values. The CUSUM OT (1) was the difference between the OT of the 1st case and the mean OT for all values: CUSUMOT(1) = OT(1) – OT(mean). The CUSUM OT(2) was the difference between the OT of the 2nd case and the mean OT for all values added to the CUSUMOT(1): CUSUMOT(2) = OT(2) – OT(mean) + CUSUMOT(1). This process continued successively until the last case: CUSUMOT(n) = OT(n) – OT(mean) + CUSUMOT(n–1). Linear regression was used to produce a recursive curve. The R2 value was calculated to determine the goodness of fit of the regression curve to the observation value, and a P value <0.05 indicated that the learning curve was reliable, and that the fitting was successful. The best fitting model of the CUSUM curve was .
SPSS 22.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. All the analyzed data are presented and reported as numbers (%) or medians (ranges). The continuous variables are presented as the mean value and standard deviation and were compared using Student’s t-test. The nominal variables were analyzed by the χ2 test and Fisher’s exact test. For all the statistical tests, a two-sided P value <0.05 was considered significant.
Results
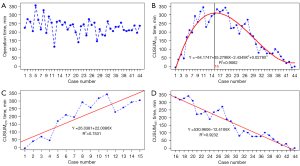
A total of 44 cervical cancer patients who underwent LESS-RH were included in this study. The demographic data and perioperative outcomes of the patients are shown in Table 1. All the operations were performed using the “chopstick” technique under LESS; there were no transitions to multiport laparoscopy or laparotomy. The median OT was 231.5 min (range, 115 to 355 min). Figure 1A shows the OTs for all cases in chronological order. Based on the cumulative sequence difference between each data point and the process average, we drew the best fitting model for the CUSUM curve (see Figure 1B). A CUSUM value of 15 was used to divide the learning curve into the following 2 different phases: Phase I (the initial learning stage), where the positive slope represents an average for the 1st 15 cases that were higher than the average value of the process (see Figure 1C); and Phase II (the consolidation stage), where the negative slope represents the next cases with 29 average values that were lower than the process average (see Figure 1D). From these data, an improvement in the surgeon’s ability was not observed until the surgical completion of the 1st 15 cases.
Table 1
| Variables | Median [range] or No. (%) | P* |
|---|---|---|
| Age (y) | 48 [27–67] | 0.9 |
| Body mass index (kg/m2) | 23.6 [15.63–30.44] | 0.54 |
| Parity | 2 [0–7] | 0.20 |
| Clinical FIGO stage | 0.07 | |
| IA1/LVSI+ | 1 (2.27) | |
| IB1 | 21 (47.73) | |
| IB2 | 3 (6.82) | |
| IIA1 | 17 (38.64) | |
| IIA2 | 2 (4.55) | |
| Histology | 0.89 | |
| Squamous | 40 (90.91) | |
| Adenocarcinoma | 3 (6.82) | |
| Adenosquamous | 1 (2.27) | |
| Uterine size (week) | 0.84 | |
| <6 w | 43 (97.73) | |
| 6–8 w | 1 (2.27) | |
| Para-aortic lymph node | 0.59 | |
| Para-aortic lymph node sampling | 2 (4.55) | |
| Para-aortic lymphadenectomy | 8 (18.18) | |
| Pelvic lymph nodes | 18 [10–31] | 0.88 |
| Para-aortic lymph nodes | 6 [4–18] | 0.22 |
| Degree of pelvic adhesion | 0.21 | |
| None | 16 (36.36) | |
| Mild adhesion | 22 (50.00) | |
| Serious adhesion | 6 (13.64) | |
| Intraoperative complication | 1 (2.27) | |
| Postoperative complication | ||
| Clavien-Dindo grade III–IV | 3 (6.82) | |
| Operative time (min) | 231.5 [115–355] | |
| Estimated blood loss (mL) | 180 [10–800] | |
| Length of postoperative hospital stay | 9 [3–16] | |
| Time of catheter remove | 14 [3–100] | |
| Adjuvant treatment | ||
| Radiotherapy | 2 (4.55) | |
| Concurrent chemoradiotherapy | 15 (34.09) | |
| Chemotherapy | 8 (18.18) | |
| Recurrence | 4 (9.09) | |
| Death of disease | 0 |
*P means effect of different characteristics on operation time (Kendall’s tau-b), P<0.05 means significant influence. FIGO, International Federation of Gynecology and Obstetrics; LVSI, lymphatic vascular space invasion.
No significant differences were observed in terms of the age, BMI, parity, FIGO stage, or range of radical hysterectomy between the 2 phases. The OT of Phase II was significantly lower than that of Phase I (259 vs. 219 min; P=0.02). In Phase I, there was 1 case of intraoperative complications and 3 cases of postoperative complications above C–D grade III, 1 patient had left external iliac vein injury, 1 had postoperative ileus, 1 had lymphoid leakage, and 1 had a ureterovaginal fistula. The cases in Phase II had more complicated surgical features than those in Phase I, such as higher rates of locally advanced cervical carcinoma (Ib2 and IIa2) (13.79% vs. 6.67%), para-aortic lymph node resection completion (27.59% vs. 13.33%), pelvic adhesions (65.51% vs. 60%), and high-risk pathological features (20.69% vs. 6.67%). However, these differences were not statistically significant (see Table 2). Neither the number of pelvic lymph nodes (16 vs. 18, P=0.19) nor the estimated blood loss (100 vs. 200 mL, P=0.23) differed significantly between the two phases.
Table 2
| Variables | Median [range] or No. (%) | P* | |
|---|---|---|---|
| Phase I [1–15] | Phase II [16–44] | ||
| Age (y) | 50 [32–67] | 48 [27–64] | 0.62 |
| Body mass index (kg/m2) | 24.2 [19.5–29.0] | 23.0 [15.6–30.4] | 0.3 |
| Parity | 2 [1–3] | 2 [0–7] | 0.92 |
| Clinical FIGO stage | 0.35 | ||
| IA1/LVSI+ | 1 (6.67) | 0 | |
| IB1 | 6 (40.00) | 15 (51.72) | |
| IB2 | 0 | 3 (10.34) | |
| IIA1 | 7 (46.67) | 10 (34.48) | |
| IIA2 | 1 (6.67) | 1 (3.45) | |
| Para-aortic lymph node | 0.315 | ||
| Para-aortic lymph node sampling | 0 | 2 (6.90) | |
| Para-aortic lymphadenectomy | 2 (13.33) | 6 (20.69) | |
| Pelvic lymph nodes | 16 [10–31] | 18 [10–31] | 0.19 |
| Para-aortic lymph nodes | 5 [4–18] | 6 [4–18] | 0.29 |
| Degree of pelvic adhesion | 0.02* | ||
| None | 6 (40.00) | 10 (34.48) | |
| Mild adhesion | 6 (40.00) | 16 (55.17) | |
| Serious adhesion | 2 (20.00) | 3 (10.34) | |
| Intraoperative complication | 1 | 0 | |
| Postoperative complication | 0.03 | ||
| Clavien-Dindo grade III–IV | 3 (15.79) | 0 | |
| Operative time (min) | 259 [115–355] | 219 [141–275] | 0.02* |
| Estimated blood loss (mL) | 100 [50–800] | 200 [10–300] | 0.23 |
| Length of postoperative hospital stay | 7 [3–14] | 9 [5–16] | 0.14 |
| Time of catheter remove | 15 [3–50] | 14 [4–100] | 0.68 |
| Parametrial involvement | 0 | 1 (3.45) | |
| Lymph node positive | 1 (6.67) | 5 (17.24) | 0.64 |
| Deep stromal invasion | 6 (40.0) | 21 (72.41) | 0.04* |
| Lymphovascular space invasion | 3 (20.0) | 6 (20.69) | 0.96 |
| Recurrence | 1 (6.67) | 3 (7.69) | 1.0 |
| Death of disease | 0 | 0 | |
*P<0.05 means significant influence. FIGO, International Federation of Gynecology and Obstetrics; LVSI, lymphatic vascular space invasion.
After a median follow-up period of 45 months (range, 35–54 months), 4 cases of recurrence were reported. The anatomical site of recurrence was the bone in 2 patients, the lung in 1 patient, and the pelvic and para-aortic lymph nodes in 1 patient. There was 1 case of mortality. There was only 1 surgical case of bone metastasis in Phase I, and all the other surgical cases of bone metastasis occurred in Phase II.
Discussion
We evaluated the learning curve of LESS-RH for early stage cervical cancer using the CUSUM method. We evaluated the usefulness of a novel surgical technique named the “chopstick” technique in helping a surgeon to successfully complete the operation. We found that a surgeon with extensive experience in laparoscopic surgery achieved proficiency and stability after being trained in 15 operations, after which shorter OTs and fewer perioperative complications were observed. Perioperative complications mainly occurred in the early stage of the training (Phase I). No correlation was found in relation to the other surgical outcome indicators and follow-up treatment, such as bleeding, auxiliary treatment, the number of lymph node resections, the time of catheter extraction, or the survival outcomes.
The rising part of the learning curve was considered the initial learning stage, and the operations performed in this phase had longer OTs and more complications. The declining curve was considered the stage of ability consolidation, and this phase had shortened OTs and no complications. The curve declined slowly after rising to its peak, which indicated that it was difficult to obtain more surgical skill after 15 attempts. Furthermore, the curve reached its lowest point at 40 cases, which indicated that regardless of the amount of training, the surgeon’s operation ability had reached its limit. In addition to the surgeon’s mastery and proficiency improving obviously at the 15-case point, more difficult surgeries were performed in the later phase, including surgeries for locally advanced cervical cancer, para-aortic lymph node resection, and pelvic adhesions.
The CUSUM learning curve has been used to evaluate the learning difficulty of many types of surgical techniques, including laparoscopic surgery (10,11), robot-assisted laparoscopic surgery (12,13), and single-site laparoscopic surgery (14). With the development of the single-site technique in recent years, laparoscopy has been increasingly applied in the treatment of a variety of gynecological diseases, and studies on its learning curve have gradually increased. In the early stage of LESS development, it was reported that the achievement of proficiency and stability required 33 cases of LESS cystectomies (15) and 40 cases of LESS hysterectomies (16). A 2018 study revealed a change in this number, and showed that an experienced laparoscopic surgeon can become proficient in LESS subtotal hysterectomies after only 20 cases (17). A 2015 study evaluated the learning curve of LESS myomectomy and showed that the turning point for reaching proficiency was 45 cases (18). In 2019, a study showed that the turning point for reaching proficiency for VNOTES total hysterectomy was 20 cases (19). Compared to that of transumbilical LESS hysterectomy, the learning curve for robotic-assisted LESS hysterectomy rises more steeply, and only 13–14 cases are required to achieve proficiency (20). LESS is used mainly for the staging of early endometrial cancer in the field of gynecological malignant tumors. Barnes reviewed 110 cases of LESS endometrial cancer staging and found that the OT decreased significantly after 20 cases (21).
RH has always been considered a difficult operation in gynecological tumor treatment. In a study of robot-assisted RH, it was found that the OT, blood loss, and complication rate improved after 28 cases (9). A 2021 study (22) reported that the number of cases require to achieve surgical proficiency was 16 in transabdominal RH, 13 in laparoscopic surgery, and 21 in robot-assisted surgery. However, the sample size of this study was small (it included only 22 cases of abdominal surgery, 26 cases of laparoscopic surgery, and 41 cases of robot-assisted surgery); thus, its objectivity and accuracy are questionable.
The difficulty caused by the parallel arrangement of all the instruments in the umbilicus, which is called the “chopstick” effect, is considered an obstacle in delicate operations. The cases of LESS-RH that reached the inflection point of the learning curve are similar to those reported in laparoscopic surgery. The result was satisfactory for such a difficult surgery. According to our analysis, a number of factors affected the results. First, the surgeon in our study had a high level of experience in single-site surgery and laparoscopic RH. Second, the use of the “chopstick” technique may play an important role in LESS and simplify the difficulty of delicate operations. As mentioned above, the instruments that enter the cavity close to a single site of the abdominal wall may collide and interfere with each other. A variety of methods have been adopted to solve this problem, such as the “cross” technique, robot-assisted technique or the use of some pre-bent instruments; however, performing a delicate operation in LESS to treat gynecological cancers, especially the dissection of the vesicocervical ligament, remains difficult. The key to the delicate maneuver is that the tips of the instruments need to be placed very closely together.
In the “chopstick” technique, we used a single-site port or fascia platform to change the single fulcrum to a double fulcrum, establish the operation triangle and perform the delicate operation. Additionally, the traditional laparoscopic instruments used in the surgery will be familiar to most laparoscopic surgeons.
The cohort in this study only represents a small sample of learning curve data by a single surgeon, which limits our discussion as to whether the results are generalizable to the entire gynecologic oncology population. The required number of cases will vary depending on the previous experience and the individual skills of each surgeon. However, since the available data in the literature on LESS radical hysterectomy are limited, findings on the experience of a single surgeon also have value. Another limitation of this study is that it failed to compare a LESS-RH cohort using the “chopstick” technique and another cohort using the conventional laparoscopic technique.
In conclusion, we used the CUSUM method to analyze the learning curve of LESS-RH and we found that after 15 cases of training, the surgeon achieved proficiency and stability. There were significant differences in the OT and the incidences of complications between the 2 phases of the curve. The results of this study were derived from the learning curve of a single surgeon; however, they undoubtedly provide strong preliminary evidence of the use of LESS to treat gynecological carcinoma. We found that surgeries for complex gynecological malignant tumors can be completed by LESS, and that the “chopstick” technique may be the key to this complex operation. We will use this novel technique as a basis to carry out a variety of surgical treatments for gynecological malignant tumors in the future to further verify its value in single-site surgeries.
Acknowledgments
Funding: This study was supported by the National Key Technology R&D Program of China (Nos. 2019YFC1005200, 2019YFC1005202, and 2019YFC1005204), and a training program for clinical medical research in 2018 (No. 2018XLC3002).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4447/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4447/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4447/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was reviewed and approved by the Ethics Committee of First Affiliated Hospital, Army Medical University, PLA (No. KY2020025). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Boruta DM. Laparoendoscopic single-site surgery in gynecologic oncology: An update. Gynecol Oncol 2016;141:616-23. [Crossref] [PubMed]
- Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol 2009;114:157-61. [Crossref] [PubMed]
- Fagotti A, Boruta DM 2nd, Scambia G, et al. First 100 early endometrial cancer cases treated with laparoendoscopic single-site surgery: a multicentric retrospective study. Am J Obstet Gynecol 2012;206:353.e1-6. [Crossref] [PubMed]
- Garrett LA, Boruta DM 2nd. Laparoendoscopic single-site radical hysterectomy: the first report of LESS type III hysterectomy involves a woman with cervical cancer. Am J Obstet Gynecol 2012;207:518.e1-2. [Crossref] [PubMed]
- Yin H, Wang Z, Xu J, et al. A specific instrument to facilitate single-incision laparoscopic cholecystectomy: an initial experience. Surg Innov 2011;18:289-93. [Crossref] [PubMed]
- Wang Y, Yao Y, Dou Y, et al. Chopstick technique used in laparoendoscopic single site radical hysterectomy for early stage cervical cancer. Sci Rep 2021;11:6882. [Crossref] [PubMed]
- Katayama H, Kurokawa Y, Nakamura K, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today 2016;46:668-85. [Crossref] [PubMed]
- Wohl H. The cusum plot: its utility in the analysis of clinical data. N Engl J Med 1977;296:1044-5. [Crossref] [PubMed]
- Yim GW, Kim SW, Nam EJ, et al. Learning curve analysis of robot-assisted radical hysterectomy for cervical cancer: initial experience at a single institution. J Gynecol Oncol 2013;24:303-12. [Crossref] [PubMed]
- Zhu G, Zhang X, Tang Z, et al. The Learning Curve of Transareola Single-site Laparoendoscopic Thyroidectomy: CUSUM Analysis of a Single Surgeon's Experience. Surg Laparosc Endosc Percutan Tech 2016;26:364-7. [Crossref] [PubMed]
- Tahmasbi Rad M, Wallwiener M, Rom J, et al. Learning curve for laparoscopic staging of early and locally advanced cervical and endometrial cancer. Arch Gynecol Obstet 2013;288:635-42. [Crossref] [PubMed]
- Wang A, Polotti CF, Wang S, et al. Characterization of a learning curve for robotic cystectomy with intracorporeal urinary diversion at two institutions using the cumulative sum (CUSUM) method. Can J Urol 2019;26:10033-8. [PubMed]
- Cela V, Marrucci E, Angioni S, et al. Robot-assisted laparoscopic single-site hysterectomy: our experience and multicentric comparison with single-port laparoscopy. Minerva Ginecol 2018;70:621-8. [Crossref] [PubMed]
- Ding D, Jiang H, Nie J, et al. Concurrent Learning Curves of 3-Dimensional and Robotic-Assisted Laparoscopic Radical Hysterectomy for Early-Stage Cervical Cancer Using 2-Dimensional Laparoscopic Radical Hysterectomy as a Benchmark: A Single Surgeon's Experience. Med Sci Monit 2019;25:5903-19. [Crossref] [PubMed]
- Song T, Kim TJ, Lee YY, et al. Learning curves for single-site laparoscopic ovarian surgery. J Minim Invasive Gynecol 2012;19:344-9. [Crossref] [PubMed]
- Paek J, Kim SW, Lee SH, et al. Learning curve and surgical outcome for single-port access total laparoscopic hysterectomy in 100 consecutive cases. Gynecol Obstet Invest 2011;72:227-33. [Crossref] [PubMed]
- You SH, Huang CY, Su H, et al. The Power Law of Learning in Transumbilical Single-Port Laparoscopic Subtotal Hysterectomy. J Minim Invasive Gynecol 2018;25:994-1001. [Crossref] [PubMed]
- Lee HJ, Kim JY, Kim SK, et al. Learning Curve Analysis and Surgical Outcomes of Single-port Laparoscopic Myomectomy. J Minim Invasive Gynecol 2015;22:607-11. [Crossref] [PubMed]
- Wang CJ, Go J, Huang HY, et al. Learning curve analysis of transvaginal natural orifice transluminal endoscopic hysterectomy. BMC Surg 2019;19:88. [Crossref] [PubMed]
- Lopez S, Mulla ZD, Hernandez L, et al. A Comparison of Outcomes Between Robotic-Assisted, Single-Site Laparoscopy Versus Laparoendoscopic Single Site for Benign Hysterectomy. J Minim Invasive Gynecol 2016;23:84-8. [Crossref] [PubMed]
- Barnes H, Harrison R, Huffman L, et al. The Adoption of Single-port Laparoscopy for Full Staging of Endometrial Cancer: Surgical and Oncology Outcomes and Evaluation of the Learning Curve. J Minim Invasive Gynecol 2017;24:1029-36. [Crossref] [PubMed]
- Kim S, Min KJ, Lee S, et al. Learning curve could affect oncologic outcome of minimally invasive radical hysterectomy for cervical cancer. Asian J Surg 2021;44:174-80. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


