
Atypical endoscopic finding of colocolic intussusception: case report and literature review
Introduction
Colonic intussusception by definition requires a lead point to act as a focus in altering normal intestinal peristaltic rhythm and activity. This would then initiate the telescoping of a proximal bowel segment (termed as intussusceptum) to within the receiving lumen of a distal bowel segment (termed as intussuscipiens) (1,2).
With relevance to our case study, adult-onset colonic intussusception is rare with a reported incidence of 5%, which in turn accounts for only 1–5% of all adult intestinal obstructions (3). In 90% of the cases encountered, an organic pathology is identified as the lead point and these includes both benign and malignant colonic tumors, postoperative etiologies and idiopathic causes (4,5). Out of these etiologies, colonic adenocarcinoma is reportedly discovered in 65–70% of the cases (6).
Our aim of this case is to describe an atypical endoscopic appearance of colonic intussusception, which is clinically pertinent and relevant to endoscopic practices. We present the following case in accordance with the CARE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-2022-61/rc).
Case presentation
Our patient was a 67-year-old woman who presented to the emergency department with a 1-week history of passing melenic stools alongside mucus, followed by a 4-day history of loose watery stools and hematochezia. She denied having weight loss, fever, nausea, vomiting, constipation, abdominal pain and abdominal distension. Her comorbidities included hypertension and dyslipidemia for which she was compliant to her prescribed medications and follow-ups.
Clinical examination revealed a small-built elderly lady with a blood pressure of 131/67 mmHg, pulse rate of 94 beats per minute, temperature of 36.8 ℃ and respiratory rate of 19 breaths per minute. Her oxygen saturation was 99% on room air and she was comfortable with no pain. Per abdominal examination revealed a soft and non-tender abdomen with no palpable masses. Other systems examination was unremarkable. Digital rectal examination was positive for melenic stools.
Relevant biochemical investigations revealed an elevated total white cell count of 16.34×103/µL (normal range 4.00–10.00/µL), hemoglobin of 9.4 g/dL (normal range 12.0–15.0 g/dL), erythrocyte sedimentation rate of 120 mm/Hr (normal range <20 mm/Hr), serum lactate of 0.82 mmol/L (normal range 0.50–2.20 mmol/L), serum albumin of 28 g/L (34–48 g/L), urea of 2.7 mmol/L (normal range 3.5–7.0 mmol/L) and creatinine of 75 µmol/L (normal range 50.4–98.1 µmol/L).
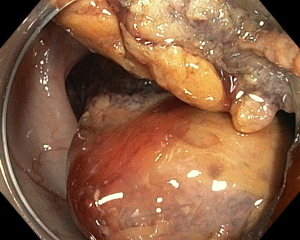
Colonoscopy done 2 days later by the referring endoscopist, revealed a large mass within the splenic flexure that prevented further progression of the adult colonoscope (outside diameter measuring 13.2 mm). Biopsies were taken and she was scheduled for a repeat colonoscopy the following day in a better equipped endoscopy center. The repeated colonoscopy confirmed the initial findings of a massive, black-to-yellowish mass lesion within the splenic flexure (Figure 1). Attempts to characterize with narrow-band imaging were not possible as there was no viable mucosa seen despite vigorous flushing. Initial suspicion of colonic bezoar was considered though endoscopic retrieval methods using a combination of endoscopic accessories were futile. At this point of time, we were concerned that the mass may have become impacted. We then switched to a slimmer diagnostic gastroscope (outside diameter measuring 9.2 mm) with the aim of maneuvering beyond the mass to identify its origin. This strategy was successful as we were able to advance further until a large stercoral ulcer was seen lying next to the mass within the ascending colon (Figures 2,3).
The colonoscopy was then abandoned as we were unable to proceed further. Decision was made to proceed with a CT scan to obtain diagnostic clarification. The CT abdomen revealed findings suspicious of perforated colocolic intussusception where the bowel-in-bowel sign and discontinuity of the medial aspect of the bowel wall was reported. The lead point (intussusceptum) was in the ascending colon invaginating into the distal transverse colon (intussuscipiens) and this was associated with proximal ileal dilatation associated with wall thickening (Figure 4). Collectively, this pointed to a subacute large bowel obstruction secondary to colocolic intussusception with radiographic features of sealed perforation.
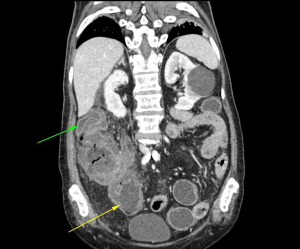
She was then referred on to our surgical colleagues where an extended right hemicolectomy with double barrel stoma was performed the next morning. Intraoperatively, a large lobulated colonic mass measuring 16 cm × 10 cm was discovered within the ascending colon. This was identified as the lead point for the source of colocolic intussusception. In addition, there was localized pus collection and scattered necrotic patches surrounding the intussusceptum in keeping with impending perforation.
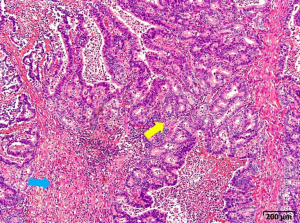
The final histopathological evaluation of the lead point confirmed this to be a pT2N0M0 ascending colonic adenocarcinoma. Amidst this lesion, there was background extensive ischemic changes in keeping with compromised blood flow attributed to the long-standing colocolic intussusception (Figure 5).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The dilemma that surrounds colonic intussusception is its variable presentation which can be non-specific (3). The timing of presentation plays a significant role in patient manifestation ranging from symptoms of acute to subacute and finally, chronic intermittent intestinal obstruction (7,8). This reflects the dynamic and variable time course of colonic intussusception prior to irreversible strangulation. The commonest reported symptoms include nausea, vomiting, gastrointestinal bleeding, altered bowel habits, constipation and abdominal distension which are also seen in many other gastrointestinal conditions (5,9). Unlike the pediatric population for which intestinal intussusception is far more common and benign, the classic triad of crampy abdominal pain, bloody diarrhea and a palpable abdominal mass is also extremely rare in adults (6). It is thus not surprising when there is a delay in diagnosis and other more common pathologies are sought first leading to detrimental outcomes for some patients (10). This highlights the importance of being extra vigilant when faced with a case of adult-onset intestinal obstruction and when there are doubts, this should be clarified by obtaining an urgent CT scan.
In relevance to our case, the initial diagnosis of colonic intussusception was not considered due to her atypical clinical presentation in addition to the unfamiliar endoscopic appearance. This was not surprising as endoscopic description of colonic intussusception is uncommon and may be dependent on the time course of presentation. Most published work describe cases diagnosed via radiographic imaging and provide images of gross specimen taken intraoperatively or just prior to histopathological processing (11). In the articles that do affix endoscopic images of colonic intussusception, the colonoscopy was performed to complement the diagnosis picked up on CT scan (11,12). In these instances, the endoscopic images of the intussusceptum were straightforward; healthy pink to ischemic purplish mucosa with an added clarity of viewing the site of ongoing intussusception (11-15). This was in contrast to our case where there was significant fecal concretion that has accrued over the mass with time in addition to worsening ischemia and necrosis, making it difficult to establish an endoscopic diagnosis. Furthermore, the intussusceptum was enormous, measuring up to 16 cm in length on the final pathological specimen. This would make it impossible to examine the full extent of the lesion endoscopically in order to better comprehend the main issue at hand.
This emphasizes the limited role of colonoscopy to purely localization, evaluation and possibly delineation of the intussuscepted mass depending on its size (1,16,17). Pertaining to the role of delineation in our case, we had to use a slimmer diagnostic gastroscope in order to advance beyond the mass before reaching its site of origin. Even then, we could not reliably make a definitive diagnosis due to the enormity of the lesion though it does set a precedent for subsequent investigation. This explained the need for CT scan which has the highest sensitivity in detecting colonic intussusception. In addition, other suspected colonic pathologies can be readily distinguished depending on their individual radiological features and hallmarks (7,18).
In terms of endoscopic intervention, the current recommendation is to only consider endoscopic reduction of intussusception once a benign lead point can be confirmed. Aside from this, operative en bloc resection abiding by oncological surgical principle remains the mainstay of treatment for adult-onset colonic intussusception (14,19). Endoscopic intervention namely, debulking with snare polypectomy is ill-advised as this would not only risk tumor spillage or seeding but may cause significant bleeding and/or colonic perforation that necessitates emergency surgical intervention with less than desirable outcomes (17,20).
In retrospect this was a challenging case mainly due to the vague symptoms on initial presentation. Our investigations were steered towards diagnosing more common colonic pathologies such as colon cancer, diverticular disease and internal hemorrhoids. Little did we expect to find an unusual large mass resembling a foreign matter, which led us to perform various endoscopic retrieval maneuvers. Looking back, the subsequent efforts to locate the mass’ origin after failure in endoscopic removal was perhaps an ideal strategy. After all, this realigned our thought process and redirected us back on track.
Thankfully, our patient went through the recommended investigative route and received the appropriate management with good outcome. She was subsequently discharged well a week later and remained well a month after the surgery.
Conclusions
We wish to highlight a variant endoscopic finding of colonic intussusception resembling a colonic bezoar. The combination of ischemia and necrosis resulting from strangulation in addition to fecal accretion makes it not only difficult to flush away but also mislead the endoscopist to consider other colonic pathologies that could be managed endoscopically. Endoscopic intervention in this patient could have led to detrimental outcomes. Our case also serves to emphasize the important role of CT scan in obtaining a clear diagnosis and in distinguishing other competing differential diagnoses prior to surgery.
Acknowledgments
We wish to express our appreciation by acknowledging our team of gastrointestinal nurses who assisted us and provided valuable insights and feedback during the second colonoscopy. They are Hendrita Malidin and Rudy J. Perizin from Queen Elizabeth Hospital, Kota Kinabalu, Sabah, Malaysia. Likewise, we would also like to acknowledge Dr. Muhammad Ilham Abd Hafidz for picking up the pathology and referring on to us for further management.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-2022-61/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-2022-61/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997;173:88-94. [Crossref] [PubMed]
- Takeuchi K, Tsuzuki Y, Ando T, et al. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol 2003;36:18-21. [Crossref] [PubMed]
- Azar T, Berger DL. Adult intussusception. Ann Surg 1997;226:134-8. [Crossref] [PubMed]
- Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg 1970;172:306-10. [Crossref] [PubMed]
- Weilbaecher D, Bolin JA, Hearn D, et al. Intussusception in adults. Review of 160 cases. Am J Surg 1971;121:531-5. [Crossref] [PubMed]
- Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg 1981;193:230-6. [Crossref] [PubMed]
- Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical relevance. Radiol Clin North Am 2003;41:1137-51. [Crossref] [PubMed]
- Martín-Lorenzo JG, Torralba-Martinez A, Lirón-Ruiz R, et al. Intestinal invagination in adults: preoperative diagnosis and management. Int J Colorectal Dis 2004;19:68-72. [Crossref] [PubMed]
- Tan KY, Tan SM, Tan AG, et al. Adult intussusception: experience in Singapore. ANZ J Surg 2003;73:1044-7. [Crossref] [PubMed]
- Haas EM, Etter EL, Ellis S, et al. Adult intussusception. Am J Surg 2003;186:75-6. [Crossref] [PubMed]
- Shenoy S. Adult intussusception: A case series and review. World J Gastrointest Endosc 2017;9:220-7. [Crossref] [PubMed]
- Ongom PA, Kijjambu SC. Adult intussusception: a continuously unveiling clinical complex illustrating both acute (emergency) and chronic disease management. OA Emergency Medicine 2013;1:3. [Crossref]
- Nakamatsu D, Nishida T, Yamamoto M, et al. Colon intussusceptions caused by a low-grade appendiceal mucinous neoplasm. Indian J Gastroenterol 2018;37:475-6. [Crossref] [PubMed]
- Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol 2009;15:407-11. [Crossref] [PubMed]
- Akçay MN, Polat M, Cadirci M, et al. Tumor-induced ileo-ileal invagination in adults. Am Surg 1994;60:980-1. [PubMed]
- Hirasaki S, Kanzaki H, Fujita K, et al. Ileal schwannoma developing into ileocolic intussusception. World J Gastroenterol 2008;14:638-40. [Crossref] [PubMed]
- Chang FY, Cheng JT, Lai KH. Colonoscopic diagnosis of ileocolic intussusception in an adult. A case report. S Afr Med J 1990;77:313-4. [PubMed]
- Floemer F, Bissig H, Oertli D, et al. Multislice CT in adult colocolic intussusception: case report and review of the literature. Emerg Radiol 2008;15:361-6. [Crossref] [PubMed]
- Dungerwalla M, Loh S, Smart P. Adult colonic intussusception: Surgery still the best option. J Surg Case Rep 2012;2012:3. [Crossref] [PubMed]
- Fazio RA, Wickremesinghe PC, Arsura EL, et al. Endoscopic removal of an intussuscepted appendix mimicking a polyp--an endoscopic hazard. Am J Gastroenterol 1982;77:556-8. [PubMed]




