Anterior cruciate ligament ganglion causing flexion restriction: a case report and review of literature
Introduction
A ganglion is a cystic lesion containing a myxoid matrix bounded by a pseudomembrane (1). It tends to materialize within tendon sheaths, joint spaces or muscles, and can either exist as single or multilobulated entities (2). Most ganglia appear on the dorsum of the hand (3). Ganglia in the knee are not uncommon (4). However, ganglia of the anterior cruciate ligament (ACL) are relatively rare. Literature has revealed that the prevalence of ganglia related to the ACL reported on magnetic resonance imaging (MRI) range from 0.12–0.44% (5,6).
Many of these ganglions are incidental findings on either MRI or routine arthroscopy (7). In fact, the majority of them tend to be asymptomatic and of small clinical significance. Clinically, they do not result in a fixed cluster of symptoms. Instead, the sets of symptoms observed vary from case to case. Symptoms include pain, stiffness, clicks, mechanical locking and decreased range of movement (8-10). Krudwig et al. noted that although pain, followed by stiffness, was the most frequent presenting symptom, it was only noted in 11% of their cases (7). These symptoms can correlate with the size and positioning of the ganglion within the knee joint (11). Such non-specific symptoms varied from a few weeks to 5 years (12).
Krudwig et al. also noted that ACL ganglions tended to cause restriction to knee extension due to their anterior locations. However, this was not the case for the ACL ganglion we observed. In fact, knee flexion was restricted instead. Ethics exemption was granted for this case report by our institution (NHG DSRB Reference Number: 2013/01125).
Case presentation
A 37-year-old Chinese gentleman presented with a 2-year history of non-traumatic deep-seated pain in his left knee. His pain was exacerbated by knee flexion causing him to be unable to squat fully.
Clinical examination revealed left knee range of motion from 0 to 110 degrees, with flexion limited by mechanical block and pain. There was no effusion. Mild discomfort was elicited on the patella facets with deep palpation. There was no medial or lateral joint line tenderness. Cruciate and collateral ligaments were stable. There was no swelling in the popliteal fossa to suggest the presence of Baker’s cysts.
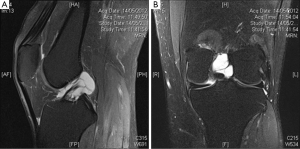
MRI of the left knee revealed a 1.5 cm × 3.3 cm × 1.7 cm septated cyst located in the intercondylar region arising from the ACL, which predominantly extended posteriorly (Figure 1).
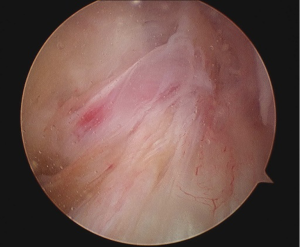
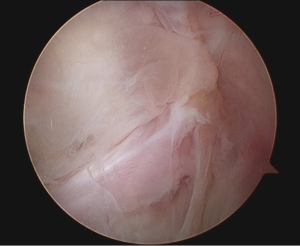
Arthroscopy revealed that the large ACL ganglion cyst was both intra-substance and extending in the posterior direction (Figures 2,3). A posteromedial portal was created to assist in visualising the ganglion from the back of the knee and to allow complete excision. The content consisted of a yellowish gelatinous material (Figure 4).
His post-operative recovery was uneventful and he was discharged the next morning. At 1-year follow-up, his left knee was symptom-free with range of motion from 0 to 130 degrees, similar to his right knee.
Discussion
The ACL ganglion cyst described in our patient appeared to be one of the largest reported in the English literature. Unlike other large ACL ganglion cysts, it caused restriction to flexion of the knee instead of extension.
The pathogenesis of ganglion cysts is contentious with theories such as herniation of synovium into surrounding tissues, mucinous degeneration of connective tissue following trauma, or synovial displacement during embryogenesis (2). Histological examination reveals that these fluid filled structures have no epithelial lining. This confirms that they are not true cysts and therefore reject the theories of synovial herniation, favouring a degenerative cause (9).
The etiology of the ganglion cysts remains unknown. Despite many reports showing that trauma need not exist for ganglia to develop, it is hypothesised that repetitive microtrauma from joint and soft tissue motion causes liberation of mucin and hyaluronic acid from ligament fibres and thus may behave as an initiator (8).
Caan was first to report an intra-articular knee cyst. This was after a cadaveric examination of an elderly male (13). Since the 1980s, there has been a rise in literature concerning ganglion cysts found in different parts of the knee. The typical locations for such lesions within the knee joint are the ACL, followed by the posterior cruciate ligament (PCL), then menisci, especially the medial meniscus (12). The cysts of the cruciate ligaments can extend outside along the fibres (anterior to the ACL and posterior to the PCL), between the 2 cruciate ligaments (intercruciate distension), or interspersing within the fibres. Nearly two thirds of all ganglion cysts originate from the ACL. They frequently arise from the tibial insertion. The shape of the ganglion cysts could be fusiform, spindle-shaped, rounded, ovoid, and well-demarcated outlines.
The ACL ganglion cyst described in our patient appeared to be one of the largest reported in the literature. It appeared to arise from the femoral attachment of the ACL and extended in the posterior direction, as well as interspersed between the ACL fibres.
One of the common presentations of a large symptomatic ACL ganglion cyst is the loss of full knee extension, as the cyst often extends anteriorly and impinges onto the roof of the intercondylar notch during knee extension. What is interesting in our case report is that the restriction was in flexion instead; this was because the cyst took an unusual course of extension predominantly in the posterior direction.
Arthroscopic excision is the gold standard treatment for patients with symptomatic intra-articular ganglion cysts, with Brown and Dandy showing that approximately 95% of patients reported positive outcomes (14). Although such a procedure necessitates hospitalisation and general anaesthesia, it has a low recurrence rate (15). A viable alternative would have been computed tomography (CT) or ultrasound-guided percutaneous aspiration. Advantages of this outpatient procedure would have included quicker recovery time and decreased invasiveness (8). However, the risk of recurrence is high (15-17) and it may be technically difficult in our case as the majority of the cyst was located posteriorly and part of it was interspersed in the ACL fibres.
In conclusion, we described a patient with a large ACL ganglion cyst extending posteriorly and thus resulted in restriction of knee flexion instead of the usual restriction of knee extension. Whilst intra-articular ACL ganglion cysts are rare, it must be included as a possible differential diagnosis as and when patients present with non-specific knee symptoms. This is especially important if a patient fails to respond to treatment prescribed for the initial diagnosis. Our patient recovered well following arthroscopic excision of the ganglion cyst and regained good knee flexion.
Acknowledgements
None
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Consent was also waivered due to the retrospective collection of data from past medical records, with anonymous and confidential reporting of data.
References
- Nikolopoulos I, Krinas G, Kipriadis D, et al. Large infrapatellar ganglionic cyst of the knee fat pad: a case report and review of the literature. J Med Case Rep 2011;5:351. [Crossref] [PubMed]
- Soren A. Pathogenesis and treatment of ganglion. Clin Orthop Relat Res 1966.173-9. [PubMed]
- Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg 1999;7:231-8. [Crossref] [PubMed]
- Sloane J, Gulati V, Penna S, et al. Large intra-articular anterior cruciate ligament ganglion cyst, presenting with inability to flex the knee. Case Rep Med 2010;2010:705919.
- Do-Dai DD, Youngberg RA, Lanchbury FD, et al. Intraligamentous ganglion cysts of the anterior cruciate ligament: MR findings with clinical and arthroscopic correlations. J Comput Assist Tomogr 1996;20:80-4. [Crossref] [PubMed]
- Huang GS, Lee CH, Chan WP, et al. Ganglion cysts of the cruciate ligaments. Acta Radiol 2002;43:419-24. [Crossref] [PubMed]
- Krudwig WK, Schulte KK, Heinemann C. Intra-articular ganglion cysts of the knee joint: a report of 85 cases and review of the literature. Knee Surg Sports Traumatol Arthrosc 2004;12:123-9. [Crossref] [PubMed]
- Bui-Mansfield LT, Youngberg RA. Intraarticular ganglia of the knee: prevalence, presentation, etiology, and management. AJR Am J Roentgenol 1997;168:123-7. [Crossref] [PubMed]
- Bergin D, Morrison WB, Carrino JA, et al. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol 2004;182:1283-7. [Crossref] [PubMed]
- Parish EN, Dixon P, Cross MJ. Ganglion cysts of the anterior cruciate ligament: a series of 15 cases. Arthroscopy 2005;21:445-7. [Crossref] [PubMed]
- Kaempffe F, D'Amato C. An unusual intra-articular ganglion of the knee with interosseous extension. A case report. J Bone Joint Surg Am 1989;71:773-5. [PubMed]
- Dinakar B, Khan T, Kumar AC, et al. Ganglion cyst of the anterior cruciate ligament: a case report. J Orthop Surg (Hong Kong) 2005;13:181-5. [PubMed]
- Caan P. Cyst formation (ganglion) in an anterior cruciate ligament of the knee. Dtsch Z Chir 1924;186:403-8. [Crossref]
- Brown MF, Dandy DJ. Intra-articular ganglia in the knee. Arthroscopy 1990;6:322-3. [Crossref] [PubMed]
- DeFriend DE, Schranz PJ, Silver DA. Ultrasound-guided aspiration of posterior cruciate ligament ganglion cysts. Skeletal Radiol 2001;30:411-4. [Crossref] [PubMed]
- Antonacci VP, Foster T, Fenlon H, et al. Technical report: CT-guided aspiration of anterior cruciate ligament ganglion cysts. Clin Radiol 1998;53:771-3. [Crossref] [PubMed]
- Campagnolo DI, Davis BA, Blacksin MF. Computed tomography--guided aspiration of a ganglion cyst of the anterior cruciate ligament: a case report. Arch Phys Med Rehabil 1996;77:732-3. [Crossref] [PubMed]