Primary extraskeletal pleural osteosarcoma: a rare pleural identity
Introduction
Extraskeletal osteosarcoma was first described by Wilson in 1941 (1); it accounts for 1–2% of all soft tissue sarcomas and 4% of all osteosarcomas (2). Primary extraskeletal osteosarcoma arising from the pleura is extremely rare with less than 10 cases published in the English literature (3). Osteosarcoma is a malignant tumor arising from the soft tissue and characterized by a uniform sarcomatoid pattern and osteoid production. A tumor is diagnosed as osteosarcoma if it has the aforementioned findings in one area and even if it shows other histological characteristics in the majority of the other areas (2).
Radiologically, extraskeletal osteosarcoma often appears as a mass with soft-tissue opacity and a diverse degree of mineralization on the chest radiograph. In approximately 50% of the patients with this tumor, calcification or osteoid formation is found. On the computed tomography (CT) scan, the tumor is found to be separate from the adjacent osseous structures and has a pseudocapsule. Moreover, CT is the best method for the detection of the matrix mineralization (4).
The differential diagnosis of extraskeletal osteosarcoma includes any identification of calcifications in the pleura benign and malignant diseases. The benign causes include previous trauma and hemothorax, infection, tuberculosis, calcifying fibrous pseudotumor, and calcified plaque by asbestos exposure; while the malignant causes include metastasis from osteogenic osteosarcoma, malignant pleural mesothelioma, fibrous mesothelioma with osseous metaplasia, parosteal osteosarcoma of the rib, and osseous Paget’s disease of the bone (5) and also calcifying malignant tumors such as malignant fibrous histiocytoma (MFH), liposarcoma, fibrosarcoma, chondrosarcoma, and malignant teratoma (6).
Case presentation
A 69-year-old woman, with a history of an orthotropic heart transplant in 1999, was admitted to the hospital after a cardiac catheterization and percutaneous coronary intervention (PCI) with two stents in the right coronary artery and posterior descending artery in April of 2015. On fluoroscopy, a large left chest mass was identified. The patient noted a 40 pound unintentional weight loss over the last year and worsening shortness of breath for some months. She complained of a generalized fatigue with a cough, without sputum production, hemoptysis or chest pain. The patient also denied fever or night sweats. She was treated in 2012 at a community hospital for pneumonia; a chest X-ray (CXR) at that time did not demonstrate a mass or effusion.
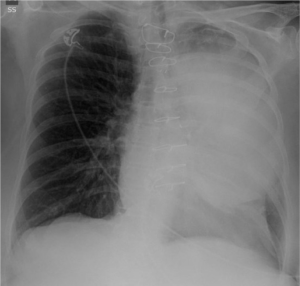
A CXR (Figure 1) in 2015 was performed followed by CT scan (Figure 2) showed a large mass in the left chest measuring greater than 17 cm with a watery density appearance and some septations were noted. The mass was well encapsulated, collapsing both left lobes. The mass appeared pleural in origin. The patient underwent a chest CT guided left pleural thoracentesis and a pigtail catheter was placed. The drainage was serous, pleural fluid chemistry corresponded with a transudate effusion; cytology did not demonstrate a malignancy. A repeat CXR following the thoracentesis demonstrated complete re-expansion of the left lung. She was discharged five days later.
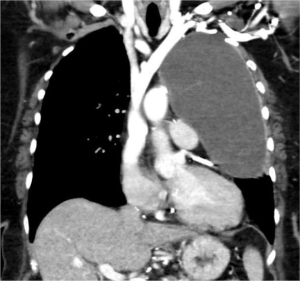
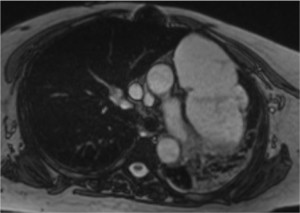
The patient continued to experience progressively worsening shortness of breath and dyspnea on exertion, limiting her to few steps of walking and become oxygen dependent. She presented again to the hospital three months later with a recurrence of the left pleural mass on CXR and CT scan. At this time, an MRI (Figure 3) of the chest showed a large complex cystic lesion within the left hemothorax; the cyst contained multiple septations and loculations of unclear etiology; but, the appearance and interval enlargement raised the possibility of a cystic malignancy. The cyst measured 12.7 cm, compromising the pericardium and altering the mediastinum. There was no mediastinal or axillary lymphadenopathy. The extensive work up failed to identify any primary source of the tumor or any metastasis. Surgical resection was the only available option of this rapidly progressed mass of unknown etiology leading to severe SOB and the progressively increasing amount of oxygen support needed.
A video assisted thoracoscopic surgical exploration was performed and didn’t show any pleural lesions. The cystic mass filled majority of chest cavity, it looked inflamed with dense adhesions to the pericardium, mediastinum, left main bronchus and the main vascular structure. An endovascular endo-gastrointestinal anastomosis (GIA) stapler was used to perform a wedge resection of the adjacent left upper lobe parenchyma adherent to the mass. R0 resection was difficult to obtain without performing a pneumonectomy due to dense adhesion of the pseudocapsule with the left main artery, this small area was cauterized to destroy the epithelium of the cyst if any, pneumonectomy was also contraindicated due to here lung function. The cytology was again negative for malignancy. The final pathology confirmed the presence of high-grade osteosarcoma. Oncology was consulted and the patient was declined chemotherapy due to her comorbidities and depleted condition. The postoperative course was unremarkable, the chest tube was removed and the patient was discharged to a nursing home 7 days later. A six month follow-up CXR did not show any reoccurrence.
Discussion
All reported cases in the literature of extraskeletal osteosarcoma showed a tumor of high-grade malignancy with poor prognosis, with a 5-year survival rate of less than 40% (7). This malignancy typically metastasizes to the distant organs (7), and reoccurrence after resection happened in more than half of the patients. Radical resection of the tumor is the appropriate initial treatment because the tumor is not particularly chemosensitive or radiosensitive (4). The role of chemotherapy in the treatment of the tumor is still being debated, as there are no specific guidelines for chemotherapy for extraskeletal osteosarcomas. A tumor size greater than 5 cm is considered a risk factor for poor prognosis and some authors advocate for post-operative systemic chemotherapy, which was not performed in this patient due to the advanced age and the her physical condition.
In contrast to osteogenic sarcoma, which commonly occurs in younger patients, primary pleural osteosarcoma typically occurs in older patients (all patient except one were older than 60 years) (2). Due to the rarity of the disease there is no documented association between smoking, asbestos and other factors; our patient is chronically immunosuppressed secondary to a heart transplant.
In conclusion, primary pleural osteosarcoma is an extremely rare diagnosis of extraskeletal osteosarcoma. Although, the cytology was negative twice in this patient, the malignancy could not be ruled out and the possibility of a primary malignant tumor should be considered in patients who present with pleural calcifications. Complete surgical resection is the standard treatment option.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Wilson H. Extraskeletal ossifying tumors. Ann Surg 1941;113:95-112. [Crossref] [PubMed]
- Rosenberg AE, Heim S. Extraskeletal osteosarcoma. In: Fletcher CDM, Unni KK, Mertens F, editors. World Health Organizing Classification of Tumors. Pathology and Genetics of Tumours of Soft Tissure and Bone. Lyon: IARC Press, 2002:182-3.
- Shiota H, Yasukawa T, Hirai A, et al. Extraskeletal osteosarcoma of the pleura:report of a case. Ann Thorac Cardiovasc Surg 2013;19:297-301. [Crossref] [PubMed]
- Mc Auley G, Jagannathan J, O'Regan K, et al. Extraskeletal osteosarcoma: spectrum of imaging findings. AJR Am J Roentgenol 2012;198:W31-7. [Crossref] [PubMed]
- Lee CH, Park CR, Kim JW, et al. Extraskeletal osteosarcoma arising from the pleura. Korean J Thorac Cardiovasc Surg 2014;47:320-4. [Crossref] [PubMed]
- Chandak P, Hunt I, Rawlins R, et al. Bone or pleura? Primary pleural osteosarcoma. J Thorac Cardiovasc Surg 2007;133:587-8. [Crossref] [PubMed]
- Lee JS, Fetsch JF, Wasdhal DA, et al. A review of 40 patients with extraskeletal osteosarcoma. Cancer 1995;76:2253-9. [Crossref] [PubMed]