Plasma alkaline phosphatase and survival in diabetic patients with acute myocardial infarction
Introduction
Alkaline phosphatase (ALP) is a hydrolase that removes phosphate groups from different types of molecules, acting as an ectoenzyme. From the cardiovascular standpoint, ALP is best known for hydrolyzing pyrophosphate, an inhibitor of vascular calcification (1). Several reports have linked plasma ALP levels to adverse cardiovascular events: all cause and cardiovascular mortality (1); risk of mortality and of hospitalization (2); coronary heart disease risk (3); mortality, myocardial infarction and stent thrombosis after coronary angioplasty (4); severity of coronary artery disease (5).
In the present investigation, we aimed at studying the relation between plasma ALP at admission and survival in diabetic patients with acute myocardial infarction. For that purpose, data from the admissions that took place during 15 months in an acute coronary care unit were retrospectively evaluated. The same cohort was previously studied in order to establish the relation between anti-diabetic drugs in use, peak plasma troponin levels after acute myocardial infarction (6), and also with survival.
Methods
The present study was retrospective, and part of the methods have been described in a previous report (6), and are hereby reproduced. From all patients admitted to an intensive coronary care unit from January 2011 to March 2012, patients with both acute myocardial infarction and Diabetes mellitus were identified. A patient was considered to have diabetes mellitus if anti-diabetic therapy was being taken, if the diagnosis had been previously established on the basis of the current recommendations or if glycated hemoglobin greater than 6.5% was present at admission. Acute myocardial infarction was diagnosed following the recommendations in use. Patients with in-hospital acute myocardial infarction were excluded. Patients who were initially admitted to another hospital, and who were later transferred into our institution, were only included if the peak value for plasma troponin I could be clearly identified.
From the electronic files, the following data were obtained: age; gender; peak plasma cardiac troponin I levels; plasma ALP; creatinine plasma levels at admission; presence of ST segment elevation in the electrocardiogram; previous history of myocardial infarction; previous coronary revascularization, either percutaneous or surgical; primary coronary angioplasty in the current episode. Troponin I was measured using the ARCHITECT STAT system, of Abbott Diagnostics (Abbott Park, Illinois, USA). The 99th percentile of troponin I in a normal population with this assay was established at 0.012 ng/mL.
Pearson correlation study was carried out, using peak plasma cardiac troponin I and ALP levels. Linear regression study, taking troponin as dependent variable, and age, gender, plasma creatinine, plasma ALP and ST segment elevation as independent variables, was also carried out. The median value for ALP (74 IU/L) was used as cut-off, and peak troponin levels and plasma creatinine were compared in the two groups of patients, by means of (the non-parametric) Mann-Whitney U test. The same test was used to compare the ages of female and male patients.
The survival of patients was established by the retrospective study of electronic health records, after a minimum period of 48 months had passed from each admission. In the case of dead patients, the date of death was recorded, when available, or alternatively the date of the last observation of each patient. In the case of patients not known to be dead, censoring was carried out in the date of the last observation. No attempt was made to study the causes of death or the medication in use after hospital discharge.
Kaplan-Meyer study was carried out, using the median value for ALP (74 IU/L) as cut-off value. The comparison between groups was made using the log-rank test.
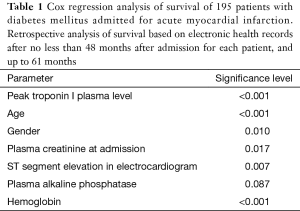
Cox-proportional hazards survival modelling was used. Covariates included gender, age, plasma creatinine, peak plasma troponin I, presence of ST segment elevation, and plasma ALP. Due to the possibility of multi-collinearity between troponin and ALP, an alternative analysis was carried out without troponin values.
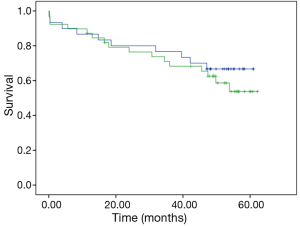
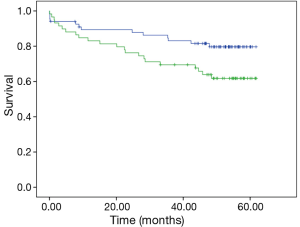
Sub-group analysis was carried out, analyzing separately female and male patients by means of Kaplan-Meyer study, as described above.
A significance level of 0.05 or lower was considered statistically significant. Data analysis was performed using the SPSS 22 software program, from IBM (Amonk, NY, USA).
The present protocol was approved by the ethics committee of our institution.
Results
Acute myocardial infarction data
Data from a total number of 195 admissions corresponding to different patients were under analysis, out of an initial number of 954 patients admitted in the period under study, from which 200 admissions corresponded to diabetic patients (in the case of more than one admission for the same patient, only the initial admission was considered). One hundred twenty-six patients were of the male sex and 69 were female. The mean age was 67.6±10.6 years. The mean age of female patients (72.8±7.8 years) was significantly greater than that of male patients (64.7±10.8 years; P<0.001). ST segment elevation myocardial infarction was present in 62 patients. Primary coronary angioplasty was carried out in 44 patients. The mean peak plasma cardiac troponin I values for the 195 admissions was 49.5±95.9 ng/mL.
A relatively weak but significant correlation was seen between the peak plasma cardiac troponin I and ALP levels (r: 0.21, significance level: 0.003). Linear regression, taking troponin as dependent variable, and age, gender, plasma creatinine, ALP, hemoglobin and ST segment elevation as independent variables, yielded an overall significance level <0.001, with a significance level of 0.004 for ALP and <0.001 for ST-segment elevation. Using the median value for ALP as cut-off (74 IU/L), peak troponin levels were not significantly different in the two groups of patients (Mann-Whitney U test)—42.0±80.2 ng/mL (mean ± standard deviation; lower ALP values) versus 57.0±109.1 ng/mL (higher ALP values). Plasma creatinine, on the other hand, was significantly higher in patients with higher values for ALP (P=0.019)—1.09±0.74 mg/dL (lower ALP values) versus 1.42±1.34 mg/dL (higher ALP values).
Survival data
After a period not inferior to 48 months and up to 61 months after each admission, the retrospective analysis of electronic records showed that 61 of the 195 patients had died (31.3%).
Kaplan-Meier analysis showed that patients with plasma ALP >74 IU/L had a significantly higher mortality, when compared to patients with plasma ALP ≤74 IU/L (with a significance level in log-rank test of 0.032; Figure 1).
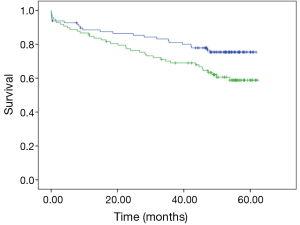
Cox regression analysis, with peak troponin I values in the model, showed that peak troponin I plasma level, age, gender, plasma creatinine at admission, ST segment elevation in electrocardiogram and hemoglobin reached significant levels, however plasma ALP did not (Table 1). Removing troponin from the model, plasma ALP reached a significance level of 0.013, whereas a lower significance level was seen with plasma creatinine (0.049) and ST segment elevation (0.283).
Full table
Sub-group analysis showed that in what concerns male patients, plasma ALP behaved as a prognostic biomarker, similarly to the whole population, whereas in what concerns female patients, no such prognostic value was seen. Kaplan-Meyer analysis yielded a significance level in log-rank test of 0.497 for female patients (Figure 2) and of 0.035 for male patients (Figure 3).
Discussion
In the present report, elevated ALP was associated to decreased survival after no less than 48 months after myocardial infarction, in a cohort of 195 diabetic patients. A weak association was seen between ALP levels and peak troponin I plasma levels. Patients with higher ALP values also had higher mean values for plasma creatinine.
Several reports have linked plasma ALP levels to adverse cardiovascular events: all cause and cardiovascular mortality (1); risk of mortality and of hospitalization (2); coronary heart disease risk (3); mortality, myocardial infarction and stent thrombosis after coronary angioplasty (4). Concerning the mechanism by which elevated ALP would be associated to worse cardiovascular outcomes, the best known is the capacity of ALP for hydrolyzing pyrophosphate, an inhibitor of vascular calcification (1). In bacteria, ALP could act to generate free phosphate groups for uptake (7). It is tempting to speculate that plasma ALP could play a role in providing phosphate groups for cardiac metabolism, since it is known that adenosine triphosphate (ATP) is the major source of energy in heart cells (8).
Concerning the relatively weak but significant correlation that was seen between peak plasma troponin level and ALP, several different hypotheses may be put forward to explain these findings. A direct interaction at the analytical level (9) could occur. Labugger et al. showed that the sera of patients with myocardial infarction has not only intact troponin I, but also a set of modified products and phosphorylated troponin (10). ALP could be involved in dephosphorylation processes involving phosphorylated troponin, with a possible impact in troponin measurements.
Sahin et al. described an association between elevated ALP levels and higher Gensini coronary disease scores in 470 patients with stable angina pectoris (5). Baars et al. studied the severity of coronary artery stenosis in patients with acute myocardial infarction and found an association with ALP and also with liver transaminases (11). Transaminases levels, however, are known to change in the context of acute myocardial infarction. Shantouf et al. described a strong association between ALP and coronary artery calcification score in a cohort of 137 hemodialysis patients (12). High levels of the coronary artery calcification score were seen in patients with ALP levels higher than 85 IU/L, and especially in patients with ALP levels ≥120 IU/L (12). Vascular calcification patterns in hemodialysis patients, however, may differ from patterns seen in non-hemodialysis patients. Jung et al. studied a cohort of 38 hemodialysis patients, and found that elevated levels of cardiac troponins T and I were associated with the degree of severity of coronary artery calcification (13). Laufer et al. studied a cohort of 615 patients, and found that the extent of coronary atherosclerosis was associated with increasing circulating levels of high sensitive cardiac troponin T (14).
Higher ALP values were associated with higher mean values for plasma creatinine. Although differences in plasma creatinine values could correspond to differences in lean muscular mass or in nutritional status, it seems probable that higher creatinine would correspond to decreased renal function (15) in these patients. Thus, patients with higher ALP values could correspond to patients with decreased renal function, a condition known to be associated to increased mortality after acute myocardial infarction (16).
ALP was shown to act as prognostic indicator concerning overall survival in these patients. Whether it is an independent prognostic factor or not, and what might be the precise mechanisms underlying this survival difference, are aspects perhaps to be elucidated in further studies. Nevertheless, such a simple and routine laboratory measurement is able to identify patients more likely to be dead in 48–61 months, raising the question of knowing if therapeutic interventions could change this worse prognosis.
Gender differences seem to exist concerning the topic under analysis. Whereas in male patients a clear separation between the two curves depicted in Figure 3 appears just a few months after myocardial infarction, in female patients, and as shown in Figure 2, no such divergence is seen, at least for the first 40 months after myocardial infarction. Female patients do not seem do derive a survival benefit from low values of ALP, and, as shown in Cox regression analysis (Table 1), female gender acted as a factor of worse prognosis. Biological differences and/or environmental factors could be responsible for this phenomenon, and female patients were in fact older on average than male patients.
Study limitations—the present study has significant limitations: it is a retrospective study; the small dimension of the sample limits the strength of conclusions; no attempt was made to characterize the drugs in use after the admission or the causes of death; the study was primarily designed for a different purpose, to study the impact of antidiabetic drugs in use at admission (6) and on survival (unpublished observations).
Conclusions
A relatively weak but significant correlation was seen between peak plasma troponin level and ALP. Elevated ALP acted as a prognostic indicator of decreased survival in diabetic patients with acute myocardial infarction, possibly in association to decreased renal function. This finding is limited to male patients, pointing to a possible different role of phosphatase activity in cardiovascular disease in male and female diabetic patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The present protocol was approved by the ethics committee of our institution.
References
- Tonelli M, Curhan G, Pfeffer M, et al. Relation between alkaline phosphatase, serum phosphate, and all-cause or cardiovascular mortality. Circulation 2009;120:1784-92. [Crossref] [PubMed]
- Abramowitz M, Muntner P, Coco M, et al. Serum alkaline phosphatase and phosphate and risk of mortality and hospitalization. Clin J Am Soc Nephrol 2010;5:1064-71. [Crossref] [PubMed]
- Wannamethee SG, Sattar N, Papcosta O, et al. Alkaline phosphatase, serum phosphate, and incident cardiovascular disease and total mortality in older men. Arterioscler Thromb Vasc Biol 2013;33:1070-6. [Crossref] [PubMed]
- Park JB, Kang DY, Yang HM, et al. Serum alkaline phosphatase is a predictor of mortality, myocardial infarction, or stent thrombosis after implantation of coronary drug-eluting stent. Eur Heart J 2013;34:920-31. [Crossref] [PubMed]
- Sahin I, Karabulut A, Gungor B, et al. Correlation between the serum alkaline phosphatase level and the severity of coronary artery disease. Coron Artery Dis 2014;25:349-52. [Crossref] [PubMed]
- Nunes JPL, Rodrigues JD, Melao F. Acute myocardial infarction associated to DPP-4 inhibitors. Heart Lung Vessel 2014;6:180-6. [PubMed]
- Horiuchi T, Horiuchi S, Mizuno D. A Possible Negative Feedback Phenomenon controlling Formation of Alkaline Phosphomonoesterase in Escherichia coli. Nature 1959;183:1529-30. [Crossref] [PubMed]
- Doenst T, Nguyen TD, Abel ED. Cardiac metabolism in heart failure: implications beyond ATP production. Circ Res 2013;113:709-24. [Crossref] [PubMed]
- Dasgupta A, Chow L, Wells A, et al. Effect of elevated concentration of alkaline phosphatase on cardiac troponin I assays. J Clin Lab Anal 2001;15:175-7. [Crossref] [PubMed]
- Labugger R, Organ L, Collier C, et al. Extensive troponin I and T modification detected in serum from patients with acute myocardial infarction. Circulation 2000;102:1221-6. [Crossref] [PubMed]
- Baars T, Neumann U, Jinawy M, et al. In Acute Myocardial Infarction Liver Parameters Are Associated With Stenosis Diameter. Medicine 2016;95:e2807. [Crossref] [PubMed]
- Shantouf R, Kovesdy CP, Kim Y, et al. Association of serum alkaline phosphatase with coronary artery calcification in maintenance hemodialysis patients. Clin J Am Soc Nephrol 2009;4:1106-14. [Crossref] [PubMed]
- Jung HH, Ma KR, Han H. Elevated concentrations of cardiac troponins are associated with severe coronary artery calcification in asymptomatic haemodialysis patients. Nephrol Dial Transplant 2004;19:3117-23. [Crossref] [PubMed]
- Laufer EM, Mingels AM, Winkens MH, et al. The extent of coronary atherosclerosis is associated with increasing circulating levels of high sensitive cardiac troponin T. Arterioscler Thromb Vasc Biol 2010;30:1269-75. [Crossref] [PubMed]
- Leibovitch I, Ben-Chaim J, Ramon J, et al. Increased serum alkaline phosphatase activity: a possible indicator of renal damage. J Clin Lab Anal 1991;5:406-9. [Crossref] [PubMed]
- Shlipak MG, Heidenreich PA, Noguchi H, et al. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med 2002;137:555-62. [Crossref] [PubMed]


