Techniques of training in the management of tension pneumothorax: bridging the gap between confidence and competence
Introduction
Tension pneumothorax carries a high mortality, with a near certain fatal outcome if not treated promptly (1,2). The management of the condition is by needle thoracocentesis, and if performed competently the condition can be treated promptly in both traumatic and atraumatic cases (1). Thoracocentesis is widely taught and relatively easily learnt.
It is a core skill as identified in both medical and paramedic training (1). Advanced Trauma Life Support and British Thoracic Society guidelines define the landmark for insertion of a needle as the mid-clavicular line, in the 2nd intercostal space (1,2).
Incorrect placement has potentially serious consequences due to damage of surrounding mediastinal and chest wall structures or failure to decompress the life-threatening tension pneumothorax. Morbidity associated with needle decompression is related to cardiac tamponade, haemorrhage, loculated intrapleural haematoma, pneumothorax, atelectasis and pneumonia (3-6).
The aim of this study was to determine both the ability and confidence of practitioners who would be expected deal with a tension pneumothorax both in and out of hospital. If any shortfall was identified between theoretical and practical knowledge the goal was to develop techniques to overcome that shortfall.
Methods
A total of 51 consenting medical practitioners were recruited to participate in a prospective single-subject crossover audit. It received local regulatory approval (7).
Participants
All participants were primary, secondary or tertiary care qualified healthcare professionals who would be expected to be able to treat a tension pneumothorax.
Intervention
After determining competence of the healthcare professionals involved, the results were circulated to the departmental leads of the included specialties and staffing groups. A 15-minute regular trauma refresher session including practical and theoretical knowledge of management of tension pneumothorax (and chest drain management) was implemented for all staff.
Anatomical diagram
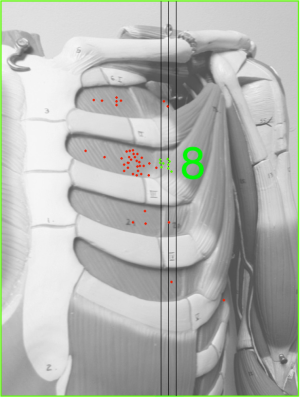
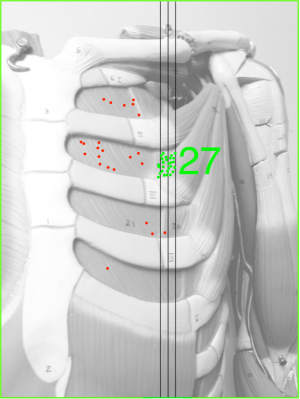
The correct anatomical position for needle decompression (2nd intercostal space, mid-clavicular line) (1) was identified on a separate 10 cm × 15 cm diagram for each candidate. Margins of error 5 mm medial and lateral to the 2nd intercostal space in mid-clavicular line were marked. Each participant’s answer was transposed onto one diagram for analysis.
Primary outcome
The primary outcomes were the accuracy of identification, before and after the intervention, of the correct anatomical position for a decompression needle thoracocentesis on an anatomical diagram (Figure 1) and also the ability, or lack thereof, to describe this position in words.

Secondary outcomes
Participants were asked to state their confidence in performing this skill by selecting 1 of 3 levels of confidence, as described in Table 1.

Full table
Additionally, a comparison was made for each candidate between anatomical and written ability and between both forms of ability and confidence at performing the procedure.
Analysis
Results were anonymous and descriptive statistics were calculated used Microsoft Excel (Microsoft Corporation, 2011).
Results
A total of 51 healthcare professionals were recruited from a single British city in primary, secondary and tertiary care.
Demographics
Participants were representative of the medical community and came from both a range of specialties and a range of seniorities. Three (5.9%) were consultant, 13 (25.5%) were senior trainees (at least 4 years postgraduate experience), 13 (25.5%) with at least 2 years postgraduate experience and 12 (23.5%) in either their first or second year of postgraduate experience. Five (9.8%) were paramedics and 5 (9.8%) emergency nurse practitioners.
Of the non-paramedics (n=46), 17 (33.3%) participants worked in emergency medicine, 7 (13.7%) in Trauma and orthopaedics, 6 (11.8%) in paediatrics, 7 (13.7%) in surgery, 4 (7.8%) in medicine, 2 (3.9%) in GP and 3 (5.9%) in anaesthetics or intensive care medicine.
Primary outcomes
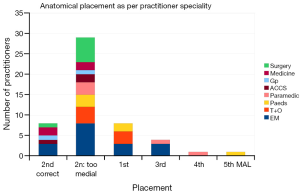
Eight marks (Figures 2,3) were positioned correctly (15.7%). A further 30 (58.8%) were placed within the 2nd intercostal space however medial to the mid-clavicular line. 13 (25.5%) were placed in the incorrect intercostal space, with 7 (13.7%) falling into the 1st, 4 (7.8%) into the 3rd, 1 (2.0%) into the 4th and 1 (2.0%) into the 5th intercostal spaces.
Anatomical and written ability
Thirty eight (74.5%) candidates were able to correctly name the anatomical position in words (Figure 4). However, 30 (78.9%) of those who correctly named the position in words were unable to correctly identify that place on the thorax diagram.
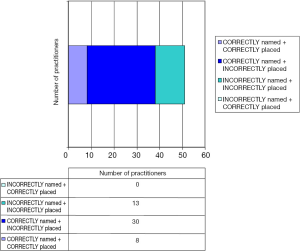
Nine (17.7%) named the position incorrectly and 4 (7.8%) people were unable to name the position at all. None of these 13 participants correctly placed a mark on the thorax diagram.
Secondary outcomes
Thirty one (60.8%) participants were confident that they would perform this procedure without seeking help. However, 27 (87.1%) of those with confidence had incorrectly identified the anatomical position of needle decompression.
Thirteen (25.5%) participants felt they understood the theory and anatomy but would be unable to perform the procedure without seeking help. Of these 2 (15.4%) were able to correctly identify the anatomy.
Seven (13.7%) participants did not understand the theory and would not perform the procedure without help. Of these, none were able to correctly identify the anatomy.
The effect of trauma course training
Thirty four (66.7%) participants had received trauma training in the form of a recognised course. Of those trauma-trained practitioners, 24 (70.6%) were able to correctly state in words where they would perform needle decompression and 4 (11.8%) were able to mark the position correctly. Eleven (32.4%) trauma-trained practitioners were unable to both anatomically and verbally identify the position correctly (Figure 5).

Twenty seven (79.4%) felt confident to perform the procedure without assistance. However, 23 (85.2%) of these incorrectly marked the anatomical site and 3 (11.1%) stated the wrong verbal position.
Five (14.7%) trauma-trained professionals felt they understood the theory but would not be confident to perform the procedure without assistance. Three (8.8%) stated they did not understand the theory and would not perform a decompression. Of these candidates, none were able to identify the correct anatomical position.
There were 17 (33.3%) participants who had not attended trauma training. Of these, 4 (25.5%) were able to correctly identify the anatomical position and 14 (82.4%) could correctly verbalise the location. Four (23.5%) had level 1 confidence, 9 (52.9%) had level 2 confidence and 4 (23.5%) had level 3 confidence.
Effects of frequent brief training
Following the use of a brief training intervention, 27 marks were positioned correctly (52.9%), compared to 8 (15.7%) prior to intervention. Fourteen (27.5%) were marked in the 2nd intercostal space but placed too medially. Ten (19.6%) were placed in the incorrect intercostal space.
Forty one (80.4%) candidates were able to correctly name the anatomical position in words, however, 13 (25.5%) of these were incorrectly placed on the anatomical diagram. This was an improvement from the pre-intervention arm.
Figure 6 compares the positions marked by the two groups.
Confidence and ability
In the post-intervention group, 41 (80.4%) participants were confident that they could perform this procedure without seeking help. Eighteen (43.9%) of those with confidence incorrectly identified the anatomical position of a decompression. Six (11.8%) participants felt they understood the theory and anatomy but would be unable to perform the procedure without seeking help. Of these 4 (66.7%) were able to correctly identify the anatomy. Four (7.8%) participants did not understand the theory and would not perform the procedure without help. Of these, 1 (25.0%) was able to correctly identify the anatomy. Figure 7 demonstrates pre and post-intervention confidence levels.
Discussion
This prospective study demonstrates an extremely low accuracy in identifying the correct anatomical landmark to perform an emergency needle thoracocentesis even amongst those with structured trauma training. The results show that it is possible to achieve a higher level of both confidence and competence with frequent refreshers of infrequently used skills.
The disparity between knowledge of position in theory and the anatomical relation is perhaps a reflection of limited exposure to ongoing practical use of the skill. Throughout medical training, emphasis is often placed on theoretical knowledge to assess candidates’ clinical competence, which can encourage trainees to place less focus on how to safely apply theoretical knowledge to a patient in a clinical situation.
Trauma training courses often involve more kinetic teaching and can provide the opportunity to practice and be assessed by a specialist in a simulated scenario. However, our study suggests that even those with trauma course training can lack both competence and confidence to perform this procedure. The level of self-confidence and ability to verbally describe the correct technique is higher amongst those who have trauma course training, but they can remain unable to perform the procedure competently.
A number of trauma-course trained participants also felt they did not understand the theory and would not be able to perform the procedure, as well as demonstrating an inability to do so, which is surprising given the emphasis placed on this skill during trauma courses.
However, the results following frequent short training sessions are promising. Improvement occurred across the board in all specialties, and in those with and without trauma training. A greater increase in ability is noted in those who are already trauma trained suggesting that regular intervention to refresh clinical skills is necessary and important, especially if the skill may be life-saving but performed infrequently.
Generally, level of confidence is high, although this does not correlate with simulated level of ability. Again this may be due to a high level of theoretical understanding with limited exposure to clinical application of that knowledge. Practitioners may feel able to perform thoracocentesis as they have adequately learned the theory and attended training courses, but due to the low incidence of tension pneumothorax have had little opportunity to practice and perform the skill to maintain precision.
While thoracocentesis is a quick and simple procedure with high potential to be life-saving, damage to the internal mammary, pulmonary and intercostal arteries have all been reported in the literature with life-threatening consequences (4,5). For this reason, although easy to learn and to teach, a certain degree of precision and knowledge of anatomy is necessary to ensure safe decompression of a tension pneumothorax (8,9). Although rarely required in clinical practice, the learning and re-learning of this skill should occur regularly through both theoretical and practical teaching to ensure the adequate ability of practitioners and reduce the danger associated with false confidence.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study received local regulatory approval and informed consent was obtained from all patients.
References
- ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg 2013;74:1363-6.
- Henry M, Arnold T, Harvey J, et al. BTS guidelines for the management of spontaneous pneumothorax. Thorax 2003;58 Suppl 2:ii39-52. [Crossref] [PubMed]
- Carney M, Ravin CE. Intercostal artery laceration during thoracocentesis: increased risk in elderly patients. Chest 1979;75:520-2. [Crossref] [PubMed]
- Butler KL, Best IM, Weaver WL, et al. Pulmonary artery injury and cardiac tamponade after needle decompression of a suspected tension pneumothorax. J Trauma 2003;54:610-1. [Crossref] [PubMed]
- Rawlins R, Brown KM, Carr CS, et al. Life threatening haemorrhage after anterior needle aspiration of pneumothoraces. A role for lateral needle aspiration in emergency decompression of spontaneous pneumothorax. Emerg Med J 2003;20:383-4. [Crossref] [PubMed]
- Leigh-Smith S, Harris T. Tension pneumothorax--time for a re-think? Emerg Med J 2005;22:8-16. [Crossref] [PubMed]
- Baer DM, Wolf MM, Risley TR. Some current dimensions of applied behavior analysis. J Appl Behav Anal 1968;1:91-7. [Crossref] [PubMed]
- Cullinane DC, Morris JA Jr, Bass JG, et al. Needle thoracostomy may not be indicated in the trauma patient. Injury 2001;32:749-52. [Crossref] [PubMed]
- Barton ED, Epperson M, Hoyt DB, et al. Prehospital needle aspiration and tube thoracostomy in trauma victims: a six-year experience with aeromedical crews. J Emerg Med 1995;13:155-63. [Crossref] [PubMed]