The definition of spine bone mineral density (BMD)-classified osteoporosis and the much inflated prevalence of spine osteoporosis in older Chinese women when using the conventional cutpoint T-score of −2.5
Osteoporosis is a systemic skeletal disease characterised by a reduction in bone mass and qualitative skeletal changes that cause an increase in bone fragility and a higher fracture risk. The clinical significance of osteoporosis lies in the fractures that occur, and the most important fracture is hip fracture. According to the 1994 World Health Organization (WHO) criteria, the T-score is defined as: (BMDpatient − BMDyoung normal mean)/SDyoung normal population, where BMD is bone mineral density and SD is the standard deviation. When the femoral neck (FN) is measured in adult women, a cutpoint value of patient BMD of 2.5 SD below the BMDyoung normal mean satisfies that the prevalence of osteoporosis for those aged ≥50 years is about 16.2%, the same as the lifetime risk of hip fragility fracture (FF) (1,2). If other sites are also considered, this cutpoint value identifies approximately 30% of postmenopausal women as having osteoporosis, which is approximately equivalent to the lifetime risk of FF at the spine, hip, or forearm. It is widely assumed that this osteoporotic subset of the population loses bone mass at a faster rate, and interventions should ideally begin before an FF occurs.
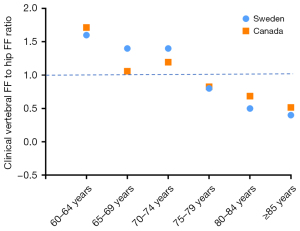
While some clinics measure only FN BMD, others measure anteroposterior lumbar spine BMD and total hip BMD as well, with the site presenting the lowest T-score considered for the diagnosis of osteoporosis. However, the 1994 WHO document did not provide a specific definition of spine osteoporosis (1). Though primary osteoporosis is a systematic disease that affects the whole skeleton, it has been demonstrated that FN BMD reduction best predicts hip FF, and spine BMD reduction best predicts vertebral FF (3,4). Therefore, when both FN BMD and spine BMD are measured, it may be reasonably assumed that the clinical endpoint for spine osteoporosis is clinical vertebral FF. It is widely believed that the ratio of clinical vertebral FF to hip FF ratio is roughly 1 (5-7). In the study of Lam et al. (6) using data from Manitoba, Canada (2000 to 2007), for the female age group of 55–84 years, there were 2,313 clinical vertebral FFs and 2,395 hip FFs. The younger subjects (<70 years) had a higher prevalence of vertebral FF and older subjects (>70 years) had a higher prevalence of hip FF. The ratio of clinical vertebral FF to hip FF is close to 1 around the age of 70 years (Figure 1) (6,7). However, the reported prevalence of clinical vertebral FF is likely affected by the ease of access to medical care, with populations with easier access reporting a higher prevalence. If we use a T-score of −2.5 as the cutpoint for defining spine osteoporosis in the National Health and Nutrition Examination Survey (NHANES) 2005–2008 data (8), the prevalence of spine osteoporosis for older USA Caucasian women ≥50 years is 15.8% (9), which is a reasonable value because it is similar to the osteoporosis prevalence of the FN BMD definition (considering the ratio of clinical vertebral FF to hip FF is close to 1). Therefore, for Caucasian women, using the same cutpoint osteoporosis T-score (i.e., ≤−2.5) to define both FN and spine osteoporosis is justifiable, although it may not be ideal. Figure 2 shows that, if lumbar spine T-score ≤−2.5 is taken as the cutpoint for defining osteoporosis, in addition to USA Caucasians and blacks (8,9), the data from Canada (10), Australia (11), Southern Italy (12), and Sweden (13) all demonstrate that FN BMD-classified osteoporosis (FN osteoporosis) prevalence and spine BMD-classified osteoporosis (spine osteoporosis) prevalence are similar. Löfman et al. (13) studied women aged 70 years and reported that FN osteoporosis prevalence and spine osteoporosis prevalence were 36% and 32%, respectively. Mautalen et al. (14) reported higher spine osteoporosis prevalence for the ‘younger’ group of their study participants and higher FN osteoporosis prevalence for the ‘older’ group of their study participants, consistent with the pattern that the clinical vertebral FF to hip FF ratio is higher than 1 prior to the age of 70 years and lower than 1 after the age of 70 years.

The FF prevalence of older Chinese women is slightly less than half that of Caucasians (9,15). This is the case for hip FF, radiographic vertebral FF (Figure 3) (16), clinical vertebral FF (Figure 4) (17,18), and many other FF sites (9,15). Since the prevalences of vertebral FF and hip FF of older Chinese women are both slightly less than half of those of Caucasians, the clinical vertebral FF to hip FF ratio is also likely to be around 1 at the age of 70 for Chinese women (i.e., the same as for Caucasians), and this is demonstrated in Figure 4. Moreover, in a Korean study, Lim et al. (19) analysed female participants from the National Health Insurance Service senior cohort (mean age: approximately 68 years), and reported clinical vertebral FF and hip FF to be 10.7% and 9.6%, respectively (derived from Tab. 3 in reference 19). In a Japanese study of 1,342 postmenopausal women aged 50 years or more with a median follow-up of 15.2 years, Kamiya et al. (20) recorded 38 and 35 cases of clinical vertebral FF and hip FF respectively. We anticipate that the dual-energy X-ray absorptiometry (DXA) based prevalence of FN osteoporosis in Chinese women will be approximately half of that of Caucasians, and that the prevalence of FN osteoporosis and spine osteoporosis will be similar in Chinese women. However, the reported data show a quite different picture. Figure 5 shows one result from a meta-analysis of different Chinese female populations, four population-based studies from mainland China, two population-based studies from Taiwan and two population-based studies from Korea, and one each from Hong Kong and Japan (21-34). Except for the meta-analysis result, all other results were randomly selected from the literature. Overall, population-based studies from China, Korea, and Japan tend to report an FN osteoporosis prevalence of >8%, which is more than half of older Caucasian women’s rate. Moreover, for all studies in Figure 5, the prevalence of spine osteoporosis was substantially higher than that of FN osteoporosis, with spine osteoporosis prevalence exceeding what would be expected from the variation of the clinical vertebral FF to hip FF ratio across different age bands (5-7,9-14,19,20,35,36).



Based on statistical modeling, we recently proposed that the cutpoint T-score for defining FN osteoporosis should be revised from ≤−2.5 to ≤−2.75 for Hong Kong older women when a local BMD reference range is being applied (9). This lowers the prevalence of FN osteoporosis in women ≥60 years from 14.7% to 10%. More notably, if we use the Caucasian cutpoint T-score of ≤−2.5 to define spine osteoporosis, the prevalence of spine osteoporosis for Hong Kong women ≥60 years is as high as 34.8%, which is unreasonable (also see Figure 2 results for Caucasians). We also proposed that (9) the cutpoint T-score for defining spine osteoporosis should be revised from −2.5 to −3.74 in order to arrive at a prevalence of spine osteoporosis of 10% for Hong Kong women ≥60 years old using the local BMD reference of Lynn et al. (37). In an empirical study on women with radiographic vertebral FF, we recently demonstrated that, at the mean age of 73.5 years and considering vertebral FF status, an FN T-score of −2.56 for Italian Caucasians is equivalent to −2.61 for Hong Kong Chinese, while a lumbar spine T-score of −2.7 for Italian Caucasians is equivalent to −3.54 for Hong Kong Chinese [n=310 Chinese and Italian pairs (38)]. For the 512 Chinese cases [mean age: 74.0 years, from the MsOS (Hong Kong) study] analysed in that study, 20.5% of the cases had FN osteoporosis, while 41.0% had spine osteoporosis when the conventional cutpoint T-score of −2.5 was used (38).
In conclusion, while a cutpoint T-score ≤−2.5 for defining spine osteoporosis is justified for Caucasian women, for Chinese women the same cutpoint T-score much inflates the estimated prevalence of spine osteoporosis. Despite DXA being an imperfect method for measuring bone strength, in addition to the use of a local BMD reference database, an adjusted cutpoint T-score for defining osteoporosis among elderly Chinese women should be applied, particularly for spine BMD measurements (9,38). Moreover, although this article presents female data, our earlier analysis showed a similarly inflated prevalence of spine osteoporosis in older Chinese men if the cutpoint T-score ≤−2.5 is used (9). We expect that the principles presented here may also apply to osteoporosis estimation in other East Asian populations. For example, it has been suggested that older Korean women and Japanese women have FF risk profiles similar to those of older Chinese women (Figure 4) (5,39-41).
Acknowledgments
The author thanks Professor Glen Mervyn Blake, King’s College London, UK, for his constructive comments for this article.
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4559/coif). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992]. 1994. Available online: https://apps.who.int/iris/handle/10665/39142
- Jain RK, Vokes T. Dual-energy X-ray Absorptiometry. J Clin Densitom 2017;20:291-303. [Crossref] [PubMed]
- Fink HA, Harrison SL, Taylor BC, et al. Differences in site-specific fracture risk among older women with discordant results for osteoporosis at hip and spine: study of osteoporotic fractures. J Clin Densitom 2008;11:250-9. [Crossref] [PubMed]
- Alarkawi D, Bliuc D, Nguyen TV, et al. Contribution of Lumbar Spine BMD to Fracture Risk in Individuals With T-Score Discordance. J Bone Miner Res 2016;31:274-80. [Crossref] [PubMed]
- Bow CH, Cheung E, Cheung CL, et al. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int 2012;23:879-85. [Crossref] [PubMed]
- Lam A, Leslie WD, Lix LM, et al. Major osteoporotic to hip fracture ratios in canadian men and women with Swedish comparisons: a population-based analysis. J Bone Miner Res 2014;29:1067-73. [Crossref] [PubMed]
- Kanis JA, Johnell O, Oden A, et al. Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int 2000;11:669-74. [Crossref] [PubMed]
- Looker AC, Borrud LG, Hughes JP, et al. Lumbar spine and proximal femur bone mineral density, bone mineral content, and bone area: United States, 2005-2008. Vital Health Stat 11 2012;1-132.
- Wáng YXJ, Xiao BH. Estimations of bone mineral density defined osteoporosis prevalence and cutpoint T-score for defining osteoporosis among older Chinese population: a framework based on relative fragility fracture risks. Quant Imaging Med Surg 2022;12:4346-60. [Crossref] [PubMed]
- Tenenhouse A, Joseph L, Kreiger N, et al. Estimation of the prevalence of low bone density in Canadian women and men using a population-specific DXA reference standard: the Canadian Multicentre Osteoporosis Study (CaMos). Osteoporos Int 2000;11:897-904. [Crossref] [PubMed]
- Henry MJ, Pasco JA, Nicholson GC, et al. Prevalence of osteoporosis in Australian women: Geelong Osteoporosis Study. J Clin Densitom 2000;3:261-8. [Crossref] [PubMed]
- del Puente A, Heyse SP, Mandes MG, et al. Epidemiology of osteoporosis in women in southern Italy. Aging (Milano) 1998;10:53-8. [Crossref] [PubMed]
- Löfman O, Larsson L, Toss G. Bone mineral density in diagnosis of osteoporosis: reference population, definition of peak bone mass, and measured site determine prevalence. J Clin Densitom 2000;3:177-86. [Crossref] [PubMed]
- Mautalen C, Schianchi A, Sigal D, et al. Prevalence of Osteoporosis in Women in Buenos Aires Based on Bone Mineral Density at the Lumbar Spine and Femur. J Clin Densitom 2016;19:471-6. [Crossref] [PubMed]
- Wáng YXJ. Fragility fracture prevalence among elderly Chinese is no more than half of that of elderly Caucasians. Quant Imaging Med Surg 2022;12:874-81. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Leung JCS, et al. Much lower prevalence and severity of radiographic osteoporotic vertebral fracture in elderly Hong Kong Chinese women than in age-matched Rome Caucasian women: a cross-sectional study. Arch Osteoporos 2021;16:174. [Crossref] [PubMed]
- Wáng YXJ, Deng M, Griffith JF, et al. 'Healthier Chinese spine': an update of osteoporotic fractures in men (MrOS) and in women (MsOS) Hong Kong spine radiograph studies. Quant Imaging Med Surg 2022;12:2090-105. [Crossref] [PubMed]
- Hayhoe RPG, Chan R, Skinner J, et al. Fracture Incidence and the Relevance of Dietary and Lifestyle Factors Differ in the United Kingdom and Hong Kong: An International Comparison of Longitudinal Cohort Study Data. Calcif Tissue Int 2021;109:563-76. [Crossref] [PubMed]
- Lim JY, Yoo JI, Kim RB, et al. Comparison of the incidence rates of hip and vertebral fragility fractures according to cataract surgery in elderly population: a nationwide cohort study. Arch Osteoporos 2022;17:30. [Crossref] [PubMed]
- Kamiya K, Kajita E, Tachiki T, et al. Association between hand-grip strength and site-specific risks of major osteoporotic fracture: Results from the Japanese Population-based Osteoporosis Cohort Study. Maturitas 2019;130:13-20. [Crossref] [PubMed]
- Zhang ZQ, Ho SC, Chen ZQ, et al. Reference values of bone mineral density and prevalence of osteoporosis in Chinese adults. Osteoporos Int 2014;25:497-507. [Crossref] [PubMed]
- Wu XP, Liao EY, Huang G, et al. A comparison study of the reference curves of bone mineral density at different skeletal sites in native Chinese, Japanese, and American Caucasian women. Calcif Tissue Int 2003;73:122-32. [Crossref] [PubMed]
- Zhu H, Fang J, Luo X, et al. A survey of bone mineral density of healthy Han adults in China. Osteoporos Int 2010;21:765-72. [Crossref] [PubMed]
- Wang L, Yu W, Yin X, et al. Prevalence of Osteoporosis and Fracture in China: The China Osteoporosis Prevalence Study. JAMA Netw Open 2021;4:e2121106. [Crossref] [PubMed]
- Zeng Q, Li N, Wang Q, et al. The Prevalence of Osteoporosis in China, a Nationwide, Multicenter DXA Survey. J Bone Miner Res 2019;34:1789-97. [Crossref] [PubMed]
- Woo J, Li M, Lau E. Population bone mineral density measurements for Chinese women and men in Hong Kong. Osteoporos Int 2001;12:289-95. [Crossref] [PubMed]
- Lin YC, Pan WH. Bone mineral density in adults in Taiwan: results of the Nutrition and Health Survey in Taiwan 2005-2008 (NAHSIT 2005-2008). Asia Pac J Clin Nutr 2011;20:283-91.
- Chan WP, Liu JF, Chi WL. Evaluation of bone mineral density of the lumbar spine and proximal femur in population-based routine health examinations of healthy Asians. Acta Radiol 2004;45:59-64. [Crossref] [PubMed]
- Zhang X, Dai Z, Lau EHY, et al. Prevalence of bone mineral density loss and potential risk factors for osteopenia and osteoporosis in rheumatic patients in China: logistic regression and random forest analysis. Ann Transl Med 2020;8:226. [Crossref] [PubMed]
- Tao Y, Tang S, Huang X, et al. Prevalence and Risk Factors of Osteoporosis in Chinese Postmenopausal Women Awaiting Total Knee Arthroplasty. Clin Interv Aging 2021;16:379-87. [Crossref] [PubMed]
- Jiajue R, Qi X, Jiang Y, et al. Incident Fracture Risk in Type 2 Diabetic Postmenopausal Women in Mainland China: Peking Vertebral Fracture Study. Calcif Tissue Int 2019;105:466-75. [Crossref] [PubMed]
- Cui LH, Choi JS, Shin MH, et al. Prevalence of osteoporosis and reference data for lumbar spine and hip bone mineral density in a Korean population. J Bone Miner Metab 2008;26:609-17. [Crossref] [PubMed]
- Lee KS, Bae SH, Lee SH, et al. New reference data on bone mineral density and the prevalence of osteoporosis in Korean adults aged 50 years or older: the Korea National Health and Nutrition Examination Survey 2008-2010. J Korean Med Sci 2014;29:1514-22. [Crossref] [PubMed]
- Iki M, Kagamimori S, Kagawa Y, et al. Bone mineral density of the spine, hip and distal forearm in representative samples of the Japanese female population: Japanese Population-Based Osteoporosis (JPOS) Study. Osteoporos Int 2001;12:529-37. [Crossref] [PubMed]
- Pedrazzoni M, Girasole G, Bertoldo F, et al. Definition of a population-specific DXA reference standard in Italian women: the Densitometric Italian Normative Study (DINS). Osteoporos Int 2003;14:978-82. [Crossref] [PubMed]
- Legakis I, Papadopoulos V, Tataridas V, et al. Prevalence of osteoporosis-osteopenia at lumbar spine and femur in an urban female population. An epidemiological study in the Athens Metropolitan area, Greece. Endocrinology Studies 2012;2:e1.
- Lynn HS, Lau EM, Au B, et al. Bone mineral density reference norms for Hong Kong Chinese. Osteoporos Int 2005;16:1663-8. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Leung JCS, et al. Conversion of osteoporotic vertebral fracture severity score to osteoporosis T-score equivalent status: a framework and a comparative study of Hong Kong Chinese and Rome Caucasian older women. Arch Osteoporos 2022;18:1. [Crossref] [PubMed]
- Kwok AW, Gong JS, Wang YX, et al. Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int 2013;24:877-85. [Crossref] [PubMed]
- Patel MC, Chandra M, Lo JC. Mortality following hip fracture in Chinese, Japanese, and Filipina women. Am J Manag Care 2016;22:e358-9.
- Lo JC, Chandra M, Lee C, et al. Bone Mineral Density in Older U.S. Filipino, Chinese, Japanese, and White Women. J Am Geriatr Soc 2020;68:2656-61. [Crossref] [PubMed]