
Anterior uterine incarceration complicated by placenta previa and placenta accreta spectrum disorder: a case report
Highlight box
Key findings
• For the first time, we present this rare case of anterior uterine incarceration complicated with placenta previa and placenta accreta spectrum disorder, which is misdiagnosed before operation and resulted in increase of the operative time and blood loss.
What is known and what is new?
• Retroflex uterine incarceration was reported sporadically in papers. However, despite these references, little attention has been paid while making clinical decision;
• We present a case of an anterior incarcerated uterus complicated with placenta previa and placenta accreta spectrum disorder.
What is the implication, and what should change now?
• When it comes to the patients with previous pelvic surgery, doctors need pay more attention to the position of the cervix, the situation of pelvic adhesion during prenatal examination, and be on the alert of uterine incarceration to reduce the likelihood of organ damage and major blood loss and make a complicated cesarean section to be plain sailing.
Introduction
Due to the relatively low incidence, cases of uterine incarceration have rarely been reported either at home or abroad (1-3). In the few published papers, the incarcerated uteruses are basically retroverse. In this article, we initially present a case of a patient with an anterior incarcerated uterus accompanied by placenta previa and placenta accreta spectrum disorder caused by serious pelvic adhesion which was confirmed in a second cesarean section (CS). The patient had a series of periodical ultrasound and magnetic resonance imaging (MRI) examinations in which placentopathy was described in detail. Unfortunately, her abnormal uterine position (incarceration) which was ignored and thus unreported during all the examination, finally complicated the surgery and increased the operative time and blood loss. Although the incidence is low, uterine incarceration should be noticed to avoid unnecessary trauma. By highlighting the location of cervix and uterus and noticing the dynamic changes in periodic examination, it is not difficult to identify. Hope our case can serve as a warning. Treatments to the incarcerations include spontaneous reduction, manual reduction, laparotomy, and colonoscopy (4). We present the following article in accordance with the CARE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-5158/rc).
Case presentation
A 28-year-old woman, gravida 4, para 1, at 35.6 weeks of gestation was hospitalized on October 9, 2021, suffering from placenta previa and placenta increta. The patient denied any uterine contractions, leakage of fluid, or bleeding, and remained clinically asymptomatic. The patient had a history of uterine surgical intervention and had undergone 1 cesarean delivery in 2017 and an open ectopic pregnancy surgery in 2019, both of which had been managed at a county hospital in her hometown. She stated that a diagnosis of pelvic adhesions had been confirmed in the second surgery, but the operative record was unavailable.
During the prenatal examination, each ultrasound examination suggested a total placenta previa. Based on her preoperative MRI, which indicated that the placenta was attached to the posterior lower wall of the uterus and some extended to the anterior wall covering the cervix, the placenta previa was considered complete. The image also indicated that the placenta invaded into the anterior lower layers with a range of about 50 mm × 60 mm.
On examination, the patient’s vital signs were stable. The abdomen was protuberant, and not tender with a well-healed surgical scar in the middle lower quadrant. The baseline of the fetal heart was normal. Estimated fetal weight is 3,000 g, vertex presentation. Laboratory results included: hemoglobin, 11.6 g/dL; albumin, 33.5 g/L. Other biochemical indexes were within the reference range. Due to the risk of bleeding, vaginal manipulation (including a speculum examination) was not performed because of concerns related to the placenta previa. Based on her history of the previous CS, she was diagnosed with placenta previa and placenta increta and repeat CS was recommended.
A multiple disciplinary team, including anesthesiologists, neonatologists, physicians and specialist in blood transfusion were consulted, and the preoperative preparations, including those related to the prevention of massive hemorrhage, blood volume management, and autologous transfusion, were completed without issue. The operation, which was a high-risk but common clinical surgery at our hospital, was performed on October 11, 2021.
After laparotomy, the uterus was found to be about 45 degrees dextrorotatory, and extensive intraperitoneal adhesions (including in the lower uterine segment, bladder, and anterior abdominal wall) were confirmed. On inspection, we failed to expose the old uterine scar due to the extensive adhesion with the bladder. In addition, somewhat surprisingly, we observed that the uterine body was extremely anteverted and anteflexed about 90 degrees from the ground, and the position of double attachments had moved to the lower part of the anterior wall of the uterus. After the separation of the bladder and part of the adhesion, a transverse incision on the lower uterine segment was performed and the delivery of the fetus was finished routinely.
Based on the MRI, the surgeon had assumed that the placenta was attached to the posterior lower wall of the uterus and extended to the anterior wall, then covered the cervix. However, it actually invaded the posterior lower wall with a range of about 50 mm × 50 mm and not the anterior wall as the MRI had indicated. As a result of increta, the placenta could not be separated from the uterine spontaneously, and it had to be removed manually.
A massive hemorrhage occurred on the placental separation surface. The hemorrhage from the placental site remained severe even after the use of uterotonic drugs and the multiple suturing of the bleeding surface. The operator decided to use a uterine balloon tamponade to provide pressure hemostasis. However, this manipulation was impossible to execute, as the tail end of the balloon failed to pass through the cervix. The patient was placed in the lithotomy position, and another surgeon in the operating room finally located the cervix with great effort through the patient’s vagina. With the assistance of a transvaginal probe, the surgeon in charge identified the right low segment of the uterus.
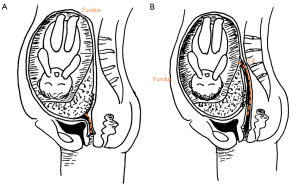
After performing the lysis of the pelvic adhesions around the uterus and cervix, the uterus was re-positioned. As a result, the placenta was found to be mostly attached to the anterior lower wall with some covering the internal os of the cervix and extending to the posterior wall. The placenta increta region was actually in the anterior myometrium. The balloon was placed and 250 mL of saline was immediately injected into it. The actual anatomy relationship during the operation was manually depicted in Figure 1.
During the entire surgery, which lasted 3 hours and 21 minutes, the patient developed severe hemorrhaging and lost approximately 5,000 mL of blood. She received blood transfusions and massive liquid infusions. Fortunately, she delivered a health male infant weighing 3,440 grams with Apgar scores of 9 at 1 minute and 10 at 5 minutes. Postoperatively, the patient had an uneventful recovery and was discharged 7 days after the operation. She was pale but in good condition at discharge, and moderate anemia was reported (hemoglobin, 9.4 mg/dL) due to the blood loss. We had lost touch with the patient since she was discharged from the hospital. The treatment timeline was shown in Figure 2.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Patients with placenta previa who have undergone a previous CS are at high risk for placenta accreta spectrum disorder, which is a major factor contributing to maternal death (5,6). The term “uterine incarceration” was coined by Hunter in 1771 (7) and is defined as the intrapelvic locking of the uterine fundus during pregnancy. The incidence of uterine incarceration is approximately 1 in 3,000–10,000 pregnancies (1-3). The following 2 types of uterine incarceration have been documented: (I) incarceration of an anteflexed gravid uterus with or without sacculation; and (II)a retroflexed uterus (8).
As the anterior/posterior myometrium of the incarcerated uterus overstretches to accommodate the growing fetus, sacculation develops. To date, only 3 cases of the anterior uterine incarceration have been reported in 2 papers (9). In these 3 cases, the posterior uterine wall overstretched and anterior sacculation developed. Each cervix was displaced high and posterior in the vagina. However, to date, there have been no previous reports of anterior uterine incarceration complicated by placenta previa and placenta accreta spectrum disorder.
The etiology of uterine incarceration is not well defined. However, there appears to be a strong connection between uterine incarceration and adhesions, pelvic tumors, uterine malformations, and an abnormal sacral concavity. In the present case, the extensive adhesion between the low segment of the uterus and the cervix due to the patient’s previous surgeries resulted in anterior uterine fixation.
Clinical manifestations are principally related to the resultant pelvic fullness. According to previous reports, patients with retroverted gravid incarcerated uteruses can suffer from lower abdominal pain, frequent painful urination, and constipation (3,8). It can also lead to more serious complications, including spontaneous abortion, urinary obstruction, gangrene of the colon, fetal growth restriction, preterm birth, and uterine rupture (9). However, our patient, whose uterus was anteverted and anteflexed, remained clinically asymptomatic during her pregnancy. The most prominent symptom would normally be observed during pelvic examination; however, the pelvic examination was purposely not performed to avoid inducing vagina bleeding. Assuming that her placenta was located in the normal position, we should have found that the cervix was extremely high, posterior, difficult to inspect, and perhaps unreachable during the speculum and bimanual examination.
To ensure the right diagnosis is made, an ultrasound study in the mid-pregnancy can be very helpful. Our patient received a series of regular prenatal ultrasonic examinations at our hospital. Having captured the abnormal ultrasound image, the examiners warned the patient of severe pelvic adhesion but communication with clinicians and relevant records were omitted. The retrospective scrutiny of an earlier ultrasound showed that the cervix was compressed against the anterior wall (Figure 3A,3B).

MRI is recommended as an effective tool to diagnose uterine incarceration (10). As for placenta accreta spectrum, the relative position of the cervical os and placenta should be confirmed by imageology preoperatively. In our case, the first MRI radiologist failed to recognize the displacement of the cervix and fundus. As a result, he misidentified the location of the placenta and placenta accreta site. The so-called “posterior inferior wall of the uterus” was actually the lower segment of the anterior wall. Before the operation, the surgeon observed the MRI scan carefully. Confused by the absence of the cervix, the surgeon consulted with another MRI radiologist by telephone, and was told that the location of the cervix appeared to be positioned backward. However, there was no further discussion.
The cervix, which is represented in Figure 4 was elongated and displaced high and posterior, and transfixed between the uterus and the spine reaching the level of the L4–L5 vertebra, making it difficult to expose. As the image shows, the uterus was incarcerated anteriorly, and the placenta was mostly attached to the anterior lower wall of the uterus with some covering the cervix and extending to the posterior wall, and the placenta increta region was actually in the anterior wall.

Some incarcerations resolve spontaneously (8), while others require manual manipulation, including manual reduction, laparotomy, and colonoscopy to reposition the uterus (4). If the incarceration reduction is not successful, a cesarean delivery may be a safer method for the termination of the pregnancy. However, performing the surgery without a correct diagnosis of anterior uterine incarceration may cause complications, such as an incision through the fundus or body of the uterus, bladder injuries, a long operation time, and postpartum hemorrhage. Thus, an early and correct diagnosis is critical.
The asymptomatic patient in our case highlights the importance of ultrasonography and MRI, which showed that the lower uterine segment was folded and attached to the front of the cervix, and the cervix was fixed upward and had been posteriorly stretched to become thinner and longer. Due to the limitations of the sound waves and the operator’s experience, it was easy to misdiagnose the patient. Compared to ultrasound, MRI provides more comprehensive anatomical insights into the pelvis, and has a higher tissue resolution and a wider field of vision. It can not only display the relative positions of the uterus, placenta, and cervix, but can also display the structure of the surrounding pelvic organs, such as the bladder, vagina, and rectum (11,12).
Conclusions
For the first time, we presented a rare case of anterior uterine incarceration complicated by placenta previa and placenta accreta spectrum disorder, which was related to the patient’s history of CS delivery and open ectopic pregnancy surgery. Imaging examinations are crucial for the correct diagnoses of patients who are asymptomatic and for those who have conditions for which vaginal manipulation is forbidden. When we interpret the imaging scans, we should pay close attention to the uterine body, lower uterine segment, cervix, vagina, bladder and other surrounding organs instead of focusing solely on the fetus and its adnexa. It is important that radiologists strictly follow the obstetric screening guidelines to conduct comprehensive and systematic examinations rather than confine their examinations just to a certain organ. Once an abnormal condition is observed, a detailed report should be made and the clinician should be contacted in a timely manner.
Radiologists and obstetricians should improve their imaging interpretation ability, and multi-disciplinary treatments should be organized as necessary. The enhancement of the identification ability of uterine incarceration will help reduce the likelihood of organ damage and major blood loss and ensure the smooth process of complicated CS (13). However, this case had 2 limitations. First, the patient’s position was changed to the lithotomy position, as we could not find the os of the cervical. It is suggested that CS be performed in the lithotomy position for patients who are diagnosed with invasive placental anomalies, as it facilitates the opportunities for intraoperative interventions (14). Second, we did not collect any follow-up information after the patient was discharged from the hospital, as we lost touch with the patient.
Acknowledgments
Funding: This study was supported by the Ningbo Science and Technology Bureau (grant No. 2019C50090, to W Zhuang), the Ningbo Key Medical Discipline (grant No. 2022-B16, to B Zhang and W Zhuang) and the Medical Scientific Research Foundation of Zhejiang Province (grant No. 2020PY024, to L Zhang).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-5158/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-5158/coif). BZ reports funding support from the Ningbo Key Medical Discipline (grant No. 2022-B16). LZ reports funding support from the Medical Scientific Research Foundation of Zhejiang Province (grant No. 2020PY024). WZ reports funding support from the Ningbo Science and Technology Bureau (grant No. 2019C50090) and the Ningbo Key Medical Discipline (grant No. 2022-B16). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fernandes DD, Sadow CA, Economy KE, et al. Sonographic and magnetic resonance imaging findings in uterine incarceration. J Ultrasound Med 2012;31:645-50. [Crossref] [PubMed]
- Shnaekel KL, Wendel MP, Rabie NZ, et al. Incarceration of the Gravid Uterus. Obstet Gynecol Surv 2016;71:613-9. [Crossref] [PubMed]
- Hess LW, Nolan TE, Martin RW, et al. Incarceration of the retroverted gravid uterus: report of four patients managed with uterine reduction. South Med J 1989;82:310-2. [Crossref] [PubMed]
- Seubert DE, Puder KS, Goldmeier P, et al. Colonoscopic release of the incarcerated gravid uterus. Obstet Gynecol 1999;94:792-4. [Crossref] [PubMed]
- Takeda S, Takeda J, Makino S. Cesarean Section for Placenta Previa and Placenta Previa Accreta Spectrum. Surg J (N Y) 2020;6:S110-21. [Crossref] [PubMed]
- Takeda S, Takeda J, Murayama Y. Placenta Previa Accreta Spectrum: Cesarean Hysterectomy. Surg J (N Y) 2021;7:S28-37. [Crossref] [PubMed]
- Longo LD. Classic pages in obstetrics and gynecology. On retroversion of the uterus. William Hunter. Medical Observations and Inquiries, vol. 4, pp. 400-409, 1771. Am J Obstet Gynecol 1978;131:95-6.
- Dierickx I, Mesens T, Van Holsbeke C, et al. Recurrent incarceration and/or sacculation of the gravid uterus: a review. J Matern Fetal Neonatal Med 2010;23:776-80. [Crossref] [PubMed]
- Hirsch E. Anterior uterine incarceration. Int J Gynaecol Obstet 1997;57:195-7. [Crossref] [PubMed]
- van Beekhuizen HJ, Bodewes HW, Tepe EM, et al. Role of magnetic resonance imaging in the diagnosis of incarceration of the gravid uterus. Obstet Gynecol 2003;102:1134-7.
- Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus. Surg J (N Y) 2020;6:S81-91. [Crossref] [PubMed]
- Bekiesinska-Figatowska M. Magnetic resonance imaging of the female pelvis after Cesarean section: a pictorial review. Insights Imaging 2020;11:75. [Crossref] [PubMed]
- Samejima K, Matsunaga S, Takai Y, et al. Efficacy of well-planned management in patients with incarcerated gravid uterus: A case series and literature review. Taiwan J Obstet Gynecol 2021;60:679-84. [Crossref] [PubMed]
- Pala Ş, Atilgan R, Başpınar M, et al. Comparison of results of Bakri balloon tamponade and caesarean hysterectomy in management of placenta accreta and increta: a retrospective study. J Obstet Gynaecol 2018;38:194-9. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)



