Post traumatic pulmonary pseudoaneurysm requiring pneumonectomy: a case report
Introduction
Penetrating trauma is the most common cause of traumatic pulmonary artery pseudoaneurysms (PAPAs) (1). The condition should be suspected when there is a history of substantial chest trauma along with consolidated well-circumscribed masses that are discovered on imaging. Traumatic PAPAs are rare lesions, and are treated with various techniques ranging from aneurysmectomy, arterial branch ligation, pulmonary resection, or angiographic embolization (2,3).
Case presentation
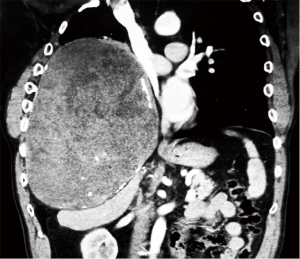
A 57-year-old male with a history of severe chest trauma from a motor vehicle collision in 1981 in which he had six fractured ribs with “flail” chest, hemopneumothorax requiring tube thoracotomy, and pulmonary contusions, presented to his primary care physician in 2013 for a concern of hemoptysis. He underwent a chest X-ray which was concerning for a mass and referred to a pulmonologist who ordered a computed tomography (CT) of the chest, which demonstrated a large soft tissue mass in the right chest however he was temporarily lost to follow-up. In November 2013, the patient had gone to the local county hospital for progressive hemoptysis, where he underwent an additional CT of the chest, abdomen, and pelvis which re-demonstrated a 27 cm × 20 cm right chest mass (Figure 1) that was causing significant local mass effect and compression with shift of the heart and mediastinum to the left. After he was admitted to the hospital, the patient underwent further diagnostics, which included a CT-guided biopsy that demonstrated “eosinophilic appearing necrotic tissue”, but was negative for malignancy. When patient’s condition improved and he was discharged with referred to the local university medical center for further evaluation by the cardiothoracic surgical team where a bronchoscopy with washings and aspiration along with endobronchial ultrasound guided biopsy was performed; demonstrating degenerating cellular debris and hemosiderin deposition, without features of malignancy. A CT positron emission tomography (PET) was also performed which only showed “fingers of FDG activity” and was otherwise “photopenic”.
Despite the lack of malignancy on the biopsy specimen, the underlying cause of the mass was unknown. After at length discussions with consulting services, consensus was that and the mass was still concerning for an aggressive process and surgery was undertaken. Once in the chest cavity there was noted to be extensive neovascularization of the nearby structures without clear tissue planes and it was decided here, that a right pneumonectomy with en bloc resection of the involved chest wall and diaphragm was to be performed. The diaphragm was reconstructed with a polytetrafluoroethylene mesh.
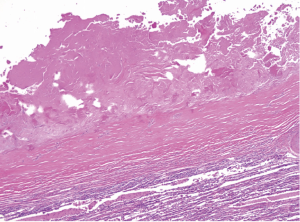
Pathologic examination of the resected material demonstrated a 25-cm aggregate of degenerating clotted blood surrounded by a thick fibrous wall (Figure 2). Cholesterol clefts and metaplastic bone formation were also prominent features seen in the fibrous wall. Normal vascular wall elements (e.g., intimal lining, elastic laminae, and smooth muscle) were lacking. Infectious organisms or malignancy were not seen. The pathologic findings were those of a massive intrathoracic pseudoaneurysm.
Discussion
The majority of PAPAs are complications of Swan-Ganz catheter placement (4,5). Other causes of PAPAs include infectious such as: (bacterial, mycobacterial, mycotic, or syphilitic), and vascular abnormalities found in such diseases such as (Marfan’s, cystic medial necrosis, Behcet’s, and other diseases causing vasculitis) (6). The infrequency of traumatic PAPAs is secondary to the high mortality associated with pulmonary artery injury, immediate repair of injuries, and the fact that it is a low pressure system (1,2,7,8).
It is not uncommon for PAPAs to escape discovery for several months to years, and until this report the longest latency reported was 30 years (3,7,8). Symptoms can vary from a completely asymptomatic patient to a patient presenting with dyspnea, cough, chest pain, and hypoxia with the most consistent presenting symptom being hemoptysis (3,7). The treatment of choice for PAPAs is the utilization of coil embolization (6). However, observation and spontaneous resolution have been mentioned in the literature (1). In the case of trauma many of the aneurysms are not amenable to coil embolization.
Regardless of symptoms or time interval, a patient with both a history of chest trauma and imaging demonstrating a large intrathoracic mass, a traumatic pulmonary artery pseudoaneurysm should be considered in the differential diagnosis. In retrospect, there was a very low consideration for pulmonary pseudoaneurysm given the size and delayed presentation of this lesion, while an angiogram was considered at one point, it was given little weight given the clinical picture. Accurate diagnosis of the lesion requires obtaining a thorough history resulting in a high index of suspicion for a traumatic pseudoaneurysm and is greatly aided by pathologic examination of the resected material, both for diagnostic confirmation and to exclude infection or malignancy.
Acknowledgements
None.
Footnote
Conflicts of Interest: Meeting Presentation—General Thoracic Surgery Club 2015, Naples, Florida, USA.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Donaldson B, Ngo-Nonga B. Traumatic pseudoaneurysm of the pulmonary artery: case report and review of the literature. Am Surg 2002;68:414-6. [PubMed]
- Khan AA, Bauer TL, Garcia MJ, et al. Angiographic embolization of a traumatic pulmonary pseudoaneurysm. Ann Thorac Surg 2005;79:2136-8. [Crossref] [PubMed]
- Savage C, Zwischenberger JB, Ventura KC, et al. Hemoptysis secondary to pulmonary pseudoaneurysm 30 years after a gunshot wound. Ann Thorac Surg 2001;71:1021-3. [Crossref] [PubMed]
- DeLima LG, Wynands JE, Bourke ME, et al. Catheter-induced pulmonary artery false aneurysm and rupture: case report and review. J Cardiothorac Vasc Anesth 1994;8:70-5. [Crossref] [PubMed]
- Cooper JP, Jackson J, Walker JM. False aneurysm of the pulmonary artery associated with cardiac catheterisation. Br Heart J 1993;69:188-90. [Crossref] [PubMed]
- Bartter T, Irwin RS, Nash G. Aneurysms of the pulmonary arteries. Chest 1988;94:1065-75. [Crossref] [PubMed]
- Symbas PN, Scott HW Jr. Traumatic aneurysm of the pulmonary artery. J Thorac Cardiovasc Surg 1963;45:645-9. [PubMed]
- Gavant ML, Winer-Muram HT. Traumatic pulmonary artery pseudoaneurysm. Can Assoc Radiol J 1986;37:108-9. [PubMed]


