
The regularity of nourishing-yin prescription for treating ascites due to hepatitis B cirrhosis based on data mining technology
Highlight box
Key findings
• Dispersion, elimination, and invigoration should all be applied in the treatment process of yin deficiency.
What is known and what is new?
• Approximately 1.5% to 4% of patients with cirrhosis further develop decompensated liver cirrhosis each year (with symptoms of ascites, hepatic encephalopathy, gastrointestinal varices, and hemorrhage, among others).
• This study used the Auxiliary Platform for Traditional Chinese Medicine Inheritance to analyze the literature related to nourishing-yin prescription for hepatitis B cirrhosis-related ascites over the past 20 years. A reference basis was subsequently provided for the clinical treatment of ascites due to hepatitis B cirrhosis.
What is the implication, and what should change now?
• All results of this study aim to provide theoretical basis for the clinical treatment of ascites due to hepatitis B cirrhosis.
Introduction
Hepatitis B cirrhosis, caused by the hepatitis B virus (HBV), is a chronic progressive liver disease. Hepatitis B cirrhosis results in diffuse liver disease due to the effect of prolonged or repeated action of one or multiple etiologies (1). It is estimated that 240 million people worldwide experience chronic HBV, and approximately 2% to 4% of patients develop compensated cirrhosis without effective treatment each year (2). Microscopically, cirrhosis shows absolute attenuation of the normal hepatocytes, massive fibrous hyperplasia, and nodule formation (3). Macroscopically, cirrhosis shows decreased volume atrophy in the liver (4). Cirrhosis is theoretically described as a “tympanite” disease in traditional Chinese medicine (TCM). In Suwen·Yinyang Yingxiang Dalun, cirrhosis was described as “yang transforming qi and yin transforming shape”. Therefore, cirrhosis is the embodiment of yin deficiency. The etiology and pathogenesis of cirrhosis can mostly be attributed to deficiency in the origin and excess in superficiality. Tonifying deficiency is the common treatment principle in treatment for cirrhosis in TCM (5).
Ascites is one of the most common complications of cirrhosis. Refractory ascites is present in 15–20% of all patients with ascites. Refractory ascites brings repeated hospitalizations, severe reduction in quality of life, and even death for patients (6). Therefore, it is particularly important to actively prevent the occurrence and development of cirrhotic ascites at an early stage.
TCM classifies patients with post-hepatitis B cirrhosis into “liver-kidney yin deficiency”, “dampness-heat internal smoldering”, “stasis-heat internal smoldering”, “liver depression and spleen deficiency”, and “spleen-kidney qi deficiency” (7). “Yin deficiency” is defined as a pathophysiological state with yin-related dysfunction (8). In the early stages of ascites due to hepatitis B cirrhosis, most of the symptoms of yin deficiency are not obvious, so yin deficiency is easily ignored in the process of treatment. However, in the late stage of hepatitis B cirrhosis-related ascites, yin deficiency is aggravated. Nourishing yin can easily invigorate the spleen for diuresis, while invigorating the spleen for diuresis can damage yin at this time (9). The treatment of late-stage hepatitis B cirrhosis-related ascites is difficult, as the disease is prone to variation and a threat to the life of patients. It has been proposed in TCM that Shaoyang-Taiyin syndrome is the basic pathogenesis of ascites from hepatitis B cirrhosis. Congestion and water stagnation are the symptoms of the occurrence of Shaoyang-Taiyin disease. Yin deficiency is an important pathological factor of ascites due to hepatitis B cirrhosis. In the treatment of ascites due to hepatitis B cirrhosis, the “reconciliation and Shaoyang” method and “warming Taiyin” are radical therapies, and promoting blood circulation and disinhibiting water are symptomatic treatments (10). In recent years, a large number of studies have proved that Chinese medicine has significant clinical effects and fewer side effects in the treatment of ascites due to hepatitis B cirrhosis, but the clinical ideas and medication habits of various scholars and physicians vary, and there are many experiences in the treatment of ascites due to hepatitis B cirrhosis, which are inconvenient to learn and pass on better (11,12). In order to optimize the treatment of ascites due to hepatitis B cirrhosis, we used the Auxiliary Platform for Traditional Chinese Medicine Inheritance (Institute of Traditional Chinese Medicine, Chinese Academy of Traditional Chinese Medicine, China) to analyze the composition of nourishing-yin prescription in the literature of hepatitis B cirrhosis-related ascites in the past 20 years. In this way, a reference basis for the clinical treatment of ascites due to hepatitis B cirrhosis was created.
Methods
Source and screening of prescriptions
Articles published from the year 2000 to 2020 related to ascites due to hepatitis B cirrhosis were searched in the Chinese National Knowledge Infrastructure (CNKI 2.0) and the Chinese Science and Technology Journal Database (CSTJ). The search terms for the first search were as follows: “ascites”, “peritoneal effusion”, and “tympanites”. The search terms for the second search were as follows: “yin”, “jing”, “blood”, “liquid”, and “jin”. The subject headings, keywords, and abstracts of each paper were combined to conduct a cross search. Tracing and querying were subsequently performed for the references of the target literature and review literature. This yielded 174 articles related to the treatment of ascites due to hepatitis B cirrhosis with the method of nourishing yin, which were then manually screened. This resulted in 198 complete prescriptions from the screened articles. The search terms for the second search were changed to “experience”, which yielded 25 articles about the treatment of ascites due to hepatitis B cirrhosis as summarized by prominent TCM doctors. After the articles were read one by one, 3 prescriptions about the treatment of ascites due to hepatitis B cirrhosis with the method of nourishing yin were selected. Finally, through combing 199 articles, a total of 201 target prescriptions were obtained. Inclusion and exclusion criteria were as follows. Inclusion criteria: (I) the disease diagnosis in the literature was clearly ascites from hepatitis B cirrhosis; the TCM certificate type included Yin deficiency. (II) The type of literature was clinical observation with effective treatment results, medical cases or experience summary of TCM experts. (III) There were clear prescriptions, flavors and dosages of herbal medicines in the literature. Exclusion criteria: (I) the prescription, flavor and dosage of Chinese medicine in the literature were incomplete; (II) duplicate literature and the same prescriptions in different literature.
Database establishment
First, a database was established with Microsoft Excel. Downloaded the medical case entry template provided by the TCM inheritance computing platform, entered the prescription data that met the inclusion criteria according to the template requirements, and standardized the terms involved in the prescriptions: deleted the method of concoction from the Chinese medicine drug names. For example, “processed rhizoma pinelliae” and “rhizoma pinellinae praeparata” were uniformly entered as “pinellia ternata” and modified according to the platform requirements with reference to the Pharmacopoeia of the People’s Republic of China (2015 edition) (13). The data was individually reviewed by two team members and timely proofread for incorrect information to ensure data authenticity and accuracy and reduce bias. After the entry was completed, the excel file was uploaded to the TCM inheritance computing platform to establish the database.
Data entry and analysis methods
The screened prescriptions were then entered with the help of the Auxiliary Platform for Traditional Chinese Medicine Inheritance. The specific steps for data entry were as follows: (I) the established database was uploaded in the “Data Upload” module of the software. (II) After “Statistical Analysis” in the “Data Analysis” module was run, “Four Properties (cold, hot, warm, and cool) (14)”, “Five Flavors (sour, sweet, bitter, pungent, and salty) (15)”, “Channel Tropism”, and “Efficiency” were analyzed, and the results of analysis were exported. (III) The “Herb Frequency”, “Association Rule”, and “Cluster Analysis” in the “Analysis of Prescription” modules were each entered. In “Association Rule”, Set the “Number of Support” (the numbers of occurrences of the same herbs at the same time among all herbs), and “Confidence Level”, and export results. In “Cluster Analysis”, cluster analysis [the core algorithm, including the improved mutual information method and complex system entropy cluster (2,5)] was conducted. Before cluster analysis, the number of clusters was selected. The “Extraction and Combination” command was then executed to perform network display [the basic algorithm was unsupervised entropy hierarchical clustering (16-18)]. Finally, the related results were exported one by one.
Results
Property, flavor, channel tropism, and efficacy statistics of the medicines in prescriptions
A total of 201 prescriptions were included. Property, flavor, channel tropism, and efficacy statistics of all medicines were recorded. According to the results, most of the medicines in prescriptions were cold, with a sweet flavor, placing them in the liver channel (Table 1). Most of the cold herbs belonged to tonifying herbs (36.3%) (Figure 1), suggesting TCM treatment of ascites due to hepatitis B cirrhosis was mainly based on tonifying deficiency.
Table 1
| Category | Classification frequency (times) |
|---|---|
| Four gases | |
| Cold | 1,004 |
| Warm | 712 |
| Neutral | 657 |
| Cool | 89 |
| Hot | 16 |
| Five flavors | |
| Sweet | 1,625 |
| Bitter | 1,049 |
| Pungent | 553 |
| Salty | 177 |
| Sour | 166 |
| Channel tropism | |
| Liver | 1,142 |
| Spleen | 1,120 |
| Kidney | 1,019 |
| Lung | 993 |
| Heart | 755 |
| Stomach | 655 |
| Bladder | 310 |
| Small intestine | 172 |
| Large intestine | 155 |
| Gall bladder | 152 |
| Triple energizer | 30 |
| Pericardium | 1 |
Frequency statistics of herb used in prescriptions
The frequency of the herbs used in 201 prescriptions were further determined. The frequency of herbs appearing ≥26 times is shown in Table 2. Poria cocos, rhizoma atractylodis macrocephalae, and radix astragali were applied frequently. Poria cocos could clear damp-heat, which had spleen-fortifying effects; rhizoma atractylodis macrocephalae focused on percolating water and resolving dampness; and radix astragali could invigorate qi for strengthening superficies. The results above indicated that TCM treatment of ascites due to hepatitis B cirrhosis consisted primarily of tonifying deficiency and invigorating the spleen for diuresis.
Table 2
| Order | Herb name | Frequency |
|---|---|---|
| 1 | Poria cocos | 136 |
| 2 | Rhizoma atractylodis macrocephalae | 113 |
| 3 | Radix astragali | 100 |
| 4 | Oriental water plantain rhizome | 98 |
| 5 | Grifola | 92 |
| 6 | Carapax trionycis | 82 |
| 7 | Radix salviae miltiorrhizae | 79 |
| 8 | Radix angelicae sinensis | 76 |
| 9 | Radix rehmanniae recens | 76 |
| 10 | Pericarpium arecae | 73 |
| 11 | Radices paeoniae alba | 59 |
| 12 | Radix ophiopogonis | 59 |
| 13 | Adenophora stricta miq | 50 |
| 14 | Semen plantaginis | 50 |
| 15 | Radix codonopsis | 50 |
| 16 | Fructus lycii | 50 |
| 17 | Radix paeoniae rubra | 48 |
| 18 | Rhizoma dioscoreae | 47 |
| 19 | Radix glycyrrhizae | 40 |
| 20 | Radix bupleuri | 37 |
| 21 | Cassia twig | 37 |
| 22 | Herba lycopi | 35 |
| 23 | Radix pseudostellariae | 34 |
| 24 | Rhizoma imperatae | 34 |
| 25 | Fructus ligustri lucidi | 33 |
| 26 | Herba artemisiae scopariae | 31 |
| 27 | Colla corii asini | 30 |
| 28 | Fructus corni | 28 |
| 29 | Concha ostreae | 26 |
| 30 | Endothelium corneum gigeriae galli | 26 |
Prescription regularities analysis based on association rules
A total of 99 common herb combinations were obtained according to association rules. The associated herb groups that appeared ≥34 times are shown in Table 3. The combination of poria cocos-rhizoma atractylodis macrocephalae and poria cocos oriental water plantain rhizome occurred with a high frequency. The association of herb combinations (confidence level ≥0.76) in prescriptions was further examined. It was found that the confidence level of oriental water plantain rhizome-radix rehmanniae recens-poria cocos, radix astragali oriental water plantain rhizome-radix salviae miltiorrhizae-poria cocos, and cassia twig-poria cocos was close to 1 (Table 4). The confidence level of the above herb combinations indicated that the prescriptions mainly contained the herbs for tonifying deficiency and invigorating spleen for diuresis. These results suggested that poria cocos, radix astragali, and rhizoma atractylodis macrocephalae were the most common compatible herbs.
Table 3
| Order | Associated herb groups | Occurrence frequency |
|---|---|---|
| 1 | Poria cocos, rhizoma atractylodis macrocephalae | 88 |
| 2 | Poria cocos, oriental water plantain rhizome | 84 |
| 3 | Poria cocos, radix astragali | 72 |
| 4 | Poria cocos, grifola | 72 |
| 5 | Rhizoma atractylodis macrocephalae, radix astragali | 70 |
| 6 | Oriental water plantain rhizome, grifola | 62 |
| 7 | Rhizoma atractylodis macrocephalae, oriental water plantain Rhizome | 62 |
| 8 | Rhizoma atractylodis macrocephalae, grifola | 58 |
| 9 | Poria cocos, radix salviae miltiorrhizae | 57 |
| 10 | Poria cocos, rhizoma atractylodis macrocephalae, radix astragali | 56 |
| 11 | Poria cocos, carapax trionycis | 56 |
| 12 | Rhizoma atractylodis macrocephalae, radix salviae miltiorrhizae | 55 |
| 13 | Rhizoma atractylodis macrocephalae, carapax trionycis | 54 |
| 14 | Radix astragali, radix salviae miltiorrhizae | 54 |
| 15 | Poria cocos, radix rehmanniae recens | 53 |
| 16 | Poria cocos, radix angelicae sinensis | 53 |
| 17 | Rhizoma atractylodis macrocephalae, pericarpium arecae | 53 |
| 18 | Poria cocos, oriental water plantain rhizome, grifola | 53 |
| 19 | Poria cocos, rhizoma atractylodis macrocephalae, oriental water plantain rhizome | 52 |
| 20 | Radix astragali, carapax trionycis | 51 |
| 21 | Radix astragali, oriental water plantain rhizome | 51 |
| 22 | Radix astragali, grifola | 49 |
| 23 | Radix astragali, pericarpium arecae | 48 |
| 24 | Poria cocos, pericarpium arecae | 48 |
| 25 | Poria cocos, rhizoma atractylodis macrocephalae, radix salviae miltiorrhizae | 46 |
| 26 | Poria cocos, rhizoma atractylodis macrocephalae, grifola | 46 |
| 27 | Poria cocos, radix astragali, oriental water plantain rhizome | 45 |
| 28 | Poria cocos, radix astragali, radix salviae miltiorrhizae | 43 |
| 29 | Radix rehmanniae recens, radix ophiopogonis | 43 |
| 30 | Poria cocos, rhizoma atractylodis macrocephalae, carapax trionycis | 43 |
| 31 | Rhizoma atractylodis macrocephalae, radix angelicae sinensis | 43 |
| 32 | Carapax trionycis, radix salviae miltiorrhizae | 42 |
| 33 | Oriental water plantain rhizome, radix salviae miltiorrhizae | 41 |
| 34 | Poria cocos, radix astragali, carapax trionycis | 41 |
| 35 | Poria cocos, radix codonopsis | 41 |
| 36 | Oriental water plantain rhizome, pericarpium arecae | 41 |
| 37 | Rhizoma atractylodis macrocephalae, radix astragali, radix salviae miltiorrhizae | 41 |
| 38 | Rhizoma atractylodis macrocephalae, oriental water plantain rhizome, grifola | 40 |
| 39 | Rhizoma atractylodis macrocephalae, radix astragali, carapax trionycis | 40 |
| 40 | Grifola, carapax trionycis | 40 |
| 41 | Poria cocos, rhizoma atractylodis macrocephalae, pericarpium arecae | 39 |
| 42 | Poria cocos, radices paeoniae alba | 39 |
| 43 | Poria cocos, radix astragali, grifola | 39 |
| 44 | Rhizoma atractylodis macrocephalae, radix astragali, oriental water plantain rhizome | 39 |
| 45 | Oriental water plantain rhizome, carapax trionycis | 38 |
| 46 | Poria cocos, semen plantaginis | 38 |
| 47 | Rhizoma atractylodis macrocephalae, radix astragali, grifola | 38 |
| 48 | Rhizoma atractylodis macrocephalae, radix astragali, pericarpium arecae | 37 |
| 49 | Poria cocos, oriental water plantain rhizome, radix salviae miltiorrhizae | 37 |
| 50 | Radix salviae miltiorrhizae, pericarpium arecae | 36 |
| 51 | Rhizoma atractylodis macrocephalae, radix paeoniae rubra | 36 |
| 52 | Poria cocos, rhizoma atractylodis macrocephalae, radix astragali, radix salviae miltiorrhizae | 36 |
| 53 | Grifola, pericarpium arecae | 36 |
| 54 | Radix astragali, radix angelicae sinensis | 35 |
| 55 | Poria cocos, rhizoma atractylodis macrocephalae, radix astragali, carapax trionycis | 35 |
| 56 | Poria cocos, cassia twig | 35 |
| 57 | Grifola, radix rehmanniae recens | 35 |
| 58 | Rhizoma atractylodis macrocephalae, radix codonopsis | 35 |
| 59 | Poria cocos, rhizoma dioscoreae | 35 |
| 60 | Radix astragali, carapax trionycis, radix salviae miltiorrhizae | 34 |
Table 4
| Order | Associations | Associations | Confidence level |
|---|---|---|---|
| 1 | Oriental water plantain rhizome, radix rehmanniae recens | Poria cocos | 0.97 |
| 2 | Radix astragali, oriental water plantain rhizome, radix salviae miltiorrhizae | Poria cocos | 0.97 |
| 3 | Cassia twig | Poria cocos | 0.95 |
| 4 | Oriental water plantain rhizome, radix salviae miltiorrhizae | Poria cocos | 0.9 |
| 5 | Grifola, radix rehmanniae recens | Poria cocos | 0.89 |
| 6 | Oriental water plantain rhizome, carapax trionycis | Poria cocos | 0.89 |
| 7 | Radix astragali, oriental water plantain rhizome | Poria cocos | 0.88 |
| 8 | Rhizoma atractylodis macrocephalae, radix astragali, carapax trionycis | Poria cocos | 0.88 |
| 9 | Rhizoma atractylodis macrocephalae, radix astragali, radix salviae miltiorrhizae | Poria cocos | 0.88 |
| 10 | Oriental water plantain rhizome | Poria cocos | 0.87 |
| 11 | Rhizoma atractylodis macrocephalae, radix astragali, oriental water plantain rhizome | Poria cocos | 0.87 |
| 12 | Radix astragali, radix angelicae sinensis | Rhizoma atractylodis macrocephalae | 0.86 |
| 13 | Poria cocos, radix astragali, carapax trionycis | Rhizoma atractylodis macrocephalae | 0.85 |
| 14 | Rhizoma atractylodis macrocephalae, oriental water plantain rhizome, grifola | Poria cocos | 0.85 |
| 15 | Oriental water plantain rhizome, grifola | Poria cocos | 0.85 |
| 16 | Radix glycyrrhizae | Poria cocos | 0.85 |
| 17 | Rhizoma atractylodis macrocephalae, oriental water plantain rhizome | Poria cocos | 0.84 |
| 18 | Rhizoma atractylodis macrocephalae, radix salviae miltiorrhizae | Poria cocos | 0.84 |
| 19 | Poria cocos, radix astragali, radix salviae miltiorrhizae | Rhizoma atractylodis macrocephalae | 0.84 |
| 20 | Poria cocos, oriental water plantain rhizome, radix salviae miltiorrhizae | Radix astragali | 0.84 |
| 21 | radix codonopsis | Poria cocos | 0.82 |
| 22 | Rhizoma atractylodis macrocephalae, Radix astragali, grifola | Poria cocos | 0.82 |
| 23 | Poria cocos, radix salviae miltiorrhizae | Rhizoma atractylodis macrocephalae | 0.81 |
| 24 | Carapax trionycis, radix salviae miltiorrhizae | Radix astragali | 0.81 |
| 25 | Poria cocos, pericarpium arecae | Rhizoma atractylodis macrocephalae | 0.81 |
| 26 | Poria cocos, rhizoma atractylodis macrocephalae, carapax trionycis | Radix astragali | 0.81 |
| 27 | Cassia twig | Grifola | 0.81 |
| 28 | Cassia twig | Oriental water plantain rhizome | 0.81 |
| 29 | Radix astragali, radix salviae miltiorrhizae | Poria cocos | 0.8 |
| 30 | Oriental water plantain rhizome, pericarpium arecae | Poria cocos | 0.8 |
| 31 | Radix astragali, carapax trionycis | Poria cocos | 0.8 |
| 32 | Rhizoma atractylodis macrocephalae, radix astragali | Poria cocos | 0.8 |
| 33 | Oriental water plantain rhizome, pericarpium arecae | Rhizoma atractylodis macrocephalae | 0.8 |
| 34 | Rhizoma atractylodis macrocephalae, carapax trionycis | Poria cocos | 0.8 |
| 35 | Radix astragali, grifola | Poria cocos | 0.8 |
| 36 | Rhizoma atractylodis macrocephalae | Poria cocos | 0.79 |
| 37 | Poria cocos, radix astragali, grifola | Rhizoma atractylodis macrocephalae | 0.79 |
| 38 | Rhizoma atractylodis macrocephalae, grifola | Poria cocos | 0.79 |
| 39 | Grifola, carapax trionycis | Poria cocos | 0.78 |
| 40 | Grifola, radix astragali | Rhizoma atractylodis macrocephalae | 0.78 |
| 41 | Radix astragali, carapax trionycis | Rhizoma atractylodis macrocephalae | 0.78 |
| 42 | Poria cocos, rhizoma atractylodis macrocephalae, radix salviae miltiorrhizae | Radix astragali | 0.78 |
| 43 | Radix astragali, grifola | Rhizoma atractylodis macrocephalae | 0.78 |
| 44 | Grifola | Poria cocos | 0.78 |
| 45 | Oriental water plantain rhizome, radix salviae miltiorrhizae | Radix astragali | 0.78 |
| 46 | Rhizoma atractylodis macrocephalae, radix angelicae sinensis | Poria cocos | 0.77 |
| 47 | Radix astragali, pericarpium arecae | Rhizoma atractylodis macrocephalae | 0.77 |
| 48 | Poria cocos, carapax trionycis | Rhizoma atractylodis macrocephalae | 0.77 |
| 49 | Carapax trionycis, radix salviae miltiorrhizae | Poria cocos | 0.76 |
| 50 | Semen plantaginis | Poria cocos | 0.76 |
Prescription regularities analysis based on an unsupervised clustering algorithm (k means) and regression analysis
According to the unsupervised clustering algorithm (k means), the prescriptions underwent cluster analysis. After further regression analysis, 5 core herb combinations were found (Figure 2). All 5 core herb combinations contained 6 herbs (Table 5), with the efficacy related to nourishing yin, soothing liver, and invigorating spleen for diuresis.
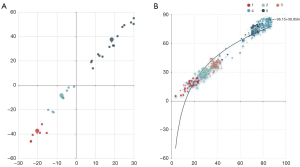
Table 5
| Combination | Core combinations | Frequencies |
|---|---|---|
| 1 | Rhizoma dioscoreae, poria cocos, oriental water plantain rhizome, fructus corni, cortex moutan, radix rehmanniae preparata | 23 |
| 2 | Rhizoma atractylodis macrocephalae, radix astragali, poria cocos, pericarpium arecae, carapax trionycis, radix salviae miltiorrhizae | 32 |
| 3 | Rhizoma atractylodis macrocephalae, poria cocos, radix astragali, pericarpium arecae, grifola, oriental water plantain rhizome | 23 |
| 4 | Rhizoma atractylodis macrocephalae, poria cocos, radix astragali, carapax trionycis, radix salviae miltiorrhizae, oriental water plantain rhizome | 75 |
| 5 | Radix ophiopogonis, radix rehmanniae recens, adenophora stricta miq, poria cocos, grifola, fructus lycii | 48 |
Discussion
HBV is a hepatotropic virus, and within TCM, it is a type of damp-heat epidemic virus. After invading the human body, HVB directly enters the liver and remains there for a long time, causing liver damage. Zheng et al. showed that HBV damaged and consumed body liquid, causing hepatic yin injury (19). The kidney is a water viscus, with the function of storing essence. However, the liver and kidney are present together in the lower energizer, exchanging essence and blood between each other. The liver and kidney share a common source, so when liver damage occurs, there is often concomitant kidney damage. Che et al. (20) thought that liver and kidney yin deficiency were the core pathogenesis in deficiency in origin and excess in superficiality and “coexistence of blood stasis and deficiency” for post hepatitis cirrhosis. In TCM, it is thought that ascites due to hepatitis B cirrhosis is a deficiency in origin and excess in superficiality; specifically, the deficiency of the liver, spleen, and kidney is the origin, while qi stagnation, blood stasis, and retained fluid is the superficiality (21,22). Ascites, one of the common complications of hepatitis B cirrhosis, is difficult to treat and characterized by frequent recurrence and high mortality (23). At present, the treatment of Western medicine for ascites consists mainly of diuretics, with poor efficacy and considerable side effects. Patients with ascites due to hepatitis B cirrhosis accompanied by deficiency in the liver, spleen, and kidney, are also prone to a deficiency in systemic yin fluid. A related study has revealed that, compared with Western medicine, the treatment of TCM for ascites due to hepatitis B cirrhosis has clear advantages (24).
Deficiency of the liver, spleen, and kidney is the predominant etiology in patients with ascites due to hepatitis B cirrhosis. Clinically, patients with severe ascites and abdominal distension are prone to experiencing complicating hydrothorax, especially right pleural effusion. Based on systemic qi and blood, the heart stores the spirit. Deficiency of qi and blood can result in loss of mind. Moreover, pathogenic factors like phlegm-heat syndrome, damp-heat, and others can blind the mind and heart, causing obnubilation and hepatic coma. Based on the theory of the liver governing free coursing, the liver can help the stomach digest food. In this study, we found that the frequencies of cold herbs were higher than those of warm herbs in clinical prescriptions. Sweet, bitter, and pungent were the main flavors of the herbs. Herbs with a sweet flavor can tonify deficiency and so are applied at high frequencies. Herbs with a bitter flavor can nourish yin and clear heat. Herbs with pungent flavor can promote qi and activate blood as well as eliminate stagnation and activate meridians. The combination of herbs of different natures and flavors can strengthen healthy qi and eliminate pathogenic factors. The efficacy of herbs examined in this study was mainly related to toxification deficiency, and the combination of herbs included diuretics for eliminating dampness, medicines for promoting blood circulation and removing blood stasis, and supplements for clearing heat and regulating qi. The efficacy of the above herbs was consistent with the treatment method of ascites due to hepatitis B cirrhosis.
Zan et al. (25) suggested that the disease position of ascites due to cirrhosis in the spleen, liver, kidney, and the spleen was the major position. Therefore, the treatment of ascites due to cirrhosis relies mainly on strengthening the spleen. Chen et al. (26) posited that in the lesion process of ascites due to cirrhosis, the key to the lesion is the spleen, with the main etiology being the insufficiency of the spleen. In this study, the 2 herbs with the highest frequencies were poria cocos and rhizoma atractylodis macrocephalae. Poria cocos and rhizoma atractylodis macrocephalae are the major components of Lishui formulas like Wuling powder, Lingguizhugan decoction, and other medicines. The herbs above are the common herbs in the treatment of ascites due to hepatitis B cirrhosis for invigorating spleen for diuresis. Li et al. (27) believe that the deficiency of vital energy, blood stasis, and fluid retention throughout each period of tympanites is the major etiology. Deficiency of vital energy is the initiating and aggravating factor of tympanites. Fan et al. (28) proposed that promoting blood circulation for removing blood stasis plays a key part in Lishui and should be continued throughout the whole process of treatment for ascites due to hepatitis B cirrhosis. Zhao et al. pointed out that the symptom of ascites due to hepatitis B cirrhosis was ascites while the disease sources were located in the blood. The stagnation of blood stasis is the basic contradiction of ascites due to hepatitis B cirrhosis (29). Ma et al. (30) reported that Jianpi Huoxue Lishui decoction could treat ascites due to hepatitis B cirrhosis and could improve the liver function of patients. In the present study, the associated herb groups of poria cocos-rhizoma atractylodis macrocephalae-grifola-oriental water plantain rhizome and poria cocos-rhizoma atractylodis macrocephalae-radix astragali could invigorate the spleen for diuresis and nourish and tonify blood, which was consistent with previous studies.
(I) Rhizoma dioscoreae-poria cocos-oriental water plantain rhizome-fructus corni-cortex moutan-radix rehmanniae preparata (combination 1) is the core combination of the prescription of Liuwei Dihuang pills with the function of nourishing-kidney yin. The above core combination of herbs can be applied for the treatment of deficiency of kidney-yin characterized by soreness and weakness of waist and knees as well as hot flashes and night sweat. (II) Rhizoma atractylodis macrocephalae-radix astragali-poria cocos-pericarpium arecae-carapax trionycis-radix salviae miltiorrhizae (combination 2) is the combination that can invigorate spleen for diuresis, nourish yin, and soften hard mass as well as nourish blood and promote blood circulation. Pericarpium arecae can lower qi and eliminate turgor, which is more valuable for the treatment of ascites due to hepatitis B cirrhosis with the symptom of abdominal distension. (III) Rhizoma atractylodis macrocephalae-poria cocos-radix astragali-pericarpium arecae-grifola-oriental water plantain rhizome (combination 3) is a herb combination that can tonify qi and invigorate the spleen for diuresis. Poria cocos, grifola, and oriental water plantain rhizome can promote urination, which can treat patients with severe ascites due to hepatitis B cirrhosis. (IV) Rhizoma atractylodis macrocephalae-cocos-radix astragali-carapax trionycis-radix salviae miltiorrhizae-oriental water plantain rhizome (combination 4) has a high cluster frequency. Compared with core combination 2, combination 4 replaces pericarpium arecae with oriental water plantain rhizome. Oriental water plantain rhizome can promote urination, clear damp-heat, and eliminate kidney zang turbidity, which are described in New Compilation of Materia Medica. Oriental water plantain rhizome can be applied for the treatment of patients with ascites due to hepatitis B cirrhosis. (V) Radix ophiopogonis-radix rehmanniae recens-adenophora stricta miq-poria cocos-grifola-fructus lycii (combination 5). The core combination above belongs to the prescription of Yiguanjian decoction, which can nourish hepatic yin and invigorate spleen for diuresis. Combination 5 is consistent the treatment principles of ascites due to hepatitis B cirrhosis.
Conclusions
Deficiency of yin is an important pathological factor for ascites due to hepatitis B cirrhosis. Dispersion, elimination, and invigoration should be all applied in the treatment process of deficiency of yin. Healthy energy is supported mainly by the combination with upper, middle, and lower energizers (triple energizers). Based on qi-blood-water, multiple visceral functions can be fully used to adjust qi movement and smooth the blood and body liquid. Overall, the results of this study aim to provide a theoretical basis for the clinical treatment of ascites due to hepatitis B cirrhosis.
Acknowledgments
Funding: This study was supported by the National Natural Science Foundation of China (No. 81173183) and the clinical effect and mechanism of TCM formula therapy on cirrhosis ascites (No. 2021M217).
Footnote
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-883/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-883/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liao Y, An L. Therapeutie effect of cangniufangjihuangqi decoction assisted basic treatment of western medicine on hepatitis b virus cirrhosis ascites. Genomics and Applied Biology 2017;36:2343-8.
- Zhao H, Wang Q, Luo C, et al. Recompensation of Decompensated Hepatitis B Cirrhosis: Current Status and Challenges. Biomed Res Int 2020;2020:9609731. [Crossref] [PubMed]
- Zhou WC, Zhang QB, Qiao L. Pathogenesis of liver cirrhosis. World J Gastroenterol 2014;20:7312-24. [Crossref] [PubMed]
- Elnaggar AS, Griesemer AD, Bentley-Hibbert S, et al. Liver atrophy and regeneration in noncirrhotic portal vein thrombosis: Effect of surgical shunts. Liver Transpl 2018;24:881-7. [Crossref] [PubMed]
- Xu MY, Liu H, Wan WX, et al. Study on the medication rules of TCM masters in the treatment of cirrhosis. Henan Traditional Chinese Medicine 2021;41:706-10.
- Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013;57:1651-3. [Crossref] [PubMed]
- Wang X, Xie G, Wang X, et al. Urinary metabolite profiling offers potential for differentiation of liver-kidney yin deficiency and dampness-heat internal smoldering syndromes in posthepatitis B cirrhosis patients. Evid Based Complement Alternat Med 2015;2015:464969. [Crossref] [PubMed]
- Zhang Q, Liu P, Cheng HF, et al. Clinical investigation on characteristics of traditional Chinese medical syndrome of hepatocirrhosis. Zhong Xi Yi Jie He Xue Bao 2003;1:108-12. [Crossref] [PubMed]
- Ruan QF, Lin L, Kang MR, et al. Experiences of Kang Liang-shi in the Treatment of Hepatitis B Liver Cirrhosis Ascites. World Journal of Integrated Traditional and Western Medicine 2014;9:923-6.
- Zhou XL, Ruan BW, Feng LJ, et al. Analysis of the treatment of ascites due to cirrhosis in the six channels syndrome differentiation. Lishizhen Medicine and Materia Medica Research 2021;32:150-1.
- Xiao M, Wang YF. To observe the clinical effect of Zi Shen Rou Gan method in the treatment of liver cirrhosis ascites of Gan Shen Yin Xu type. Chinese Community Doctors 2021;37:95-6.
- Shi L, Hao JM, Hang JM, et al. Effect of Jialingyin addition and subtraction on ascites due to liver cirrhosis of Qi and yin deficiency type and its influence on serum related inflammatory cytokines levels. Hainan Medical Journal 2021;32:1405-8.
- Commission CP. Pharmacopoeia of the People's Republic of China (2015 edition). BeiJing: China Medical Science Press, 2015.
- Deng J, Qin H, Liu L, et al. Review and reflection on study of four properties of traditional Chinese medicine. Zhongguo Zhong Yao Za Zhi 2009;34:3310-2.
- Zou P. Traditional Chinese Medicine, Food Therapy, and Hypertension Control: A Narrative Review of Chinese Literature. Am J Chin Med 2016;44:1579-94. [Crossref] [PubMed]
- Yang H, Zhao Y, Tang S. Study on the Relation of the Chinese Herbs in the Prescription of Stroke Based on the Method of Entropy. Chinese Journal of Basic Medicine in Traditional Chinese Medicine 2005;11:706.
- Tang S, Chen J. Designing new TCM prescriptions based on complex system entropy cluster. Modernization of Traditional Chinese Medicine and Materia Medica-World Science and Technology 2009;11:225-8.
- Yang H, Chen J, Tang S, et al. New drug R&D of traditional Chinese medicine: Role of data mining approaches. Journal of Biological Systems 2009;17:329-47.
- Zheng GY, Miao JQ, Chen Z. Ling Changquan’s experience in syndrome differentiation and treatment of chronic hepatitis B. Journal of Traditional Chinese Medicine 2014;55:975-6.
- Che ZY, He JC, Ma LZ, et al. The investigation on the relationship between syndrome of liver and kidney yin deficiency and virus hepatitis and posthepatitic cirrhosis. Liaoning Journal of Traditional Chinese Medicine 2011;38:632-3.
- Zhang ZL, Zhang Y. Clinical Analysis on Cirrhosis Ascites Treated with Self-mastery Xiaozhang Lishui Decoction and Incidence of Hyponatremia. Fujian Journal of Traditional Chinese Medicine 2009;40:15-6.
- Yao R. Clinical study of Xiaogu decoction and western medicine to treat ascites due to hepatitis B cirrhosis. Journal of Aerospace Medicine 2017;28:1007-9.
- Li HL, Lu XF, Li N. Efficacy of entecavir combined with alprostadil in treatment of hepatitis B-related cirrhotic ascites. Journal of Clinical Hepatology 2016;32:292-5.
- Li XL, Zhang M, Niu M. The clinical effect of Jianpi Huagu decoction combined with western medicine in the treatment of cirrhosis with ascites due to cirrhosis post hepatitis B. Shanxi Journal of Traditional Chinese Medicine 2015;36:1144-6.
- Zan L, Sun Z, Shen ZY. Shen Zhongyuan’s experience in treatment of ascites due to cirrhosis based on tonifying spleen. Hubei Journal of Traditional Chinese Medicine 2016;38:30-2.
- Chen Y, Zhang DL, Yang JL, et al. Clinical observation of using self-made Fupi Shugan decoction to treat ascites due to cirrhosis. Journal of Guiyang College of Traditional Chinese Medicine 2012;34:31-4.
- Li HL. Clinical observation on benefiting qi for activating blood circulation and diuresis in the treatment of ascites due to cirrhosis for 50 cases. Guangming Journal of Chinese Medicine 2016;31:1755-7.
- Fan YH, Bai T. Therapeutic effect of modified Gexia Zhuyu decoction for the treatment of ascites due to cirrhosis:An observation of 67 cases. Nei Mongol Journal of Traditional Chinese Medicine 2017;36:21.
- Zhao Y. Li Suling’s experience summary in treatment of tympanites of yin deficiency pattern. China's Naturopathy 2017;25:13-4.
- Ma XJ, Chen XP. Observation on the Therapeutic Effect of Jianpi Huoxue Lishui Decoction on Ascites due to Hepatitis B Cirrhosis. Guide of China Medicine 2020;18:173-4.



