
Individualized anatomical lateral plate for oblique lumbar interbody fusion: concerns required to be addressed
We have read the recently published paper entitled “Biomechanical evaluation of a novel anatomical plate for oblique lumbar interbody fusion compared with various fixations: a finite element analysis” by Huang and colleagues (1), in which a novel fixation option was presented for the oblique lumbar interbody fusion (OLIF) technique, namely anatomical lateral plate (ALP). Huang and colleagues’ new idea is much appreciated and several concrete suggestions for future researches regarding clinical application of ALP are being discussed here.
First, in clinical practice, it is difficult to accurately determine the distance between the cortical screw holes (“h” in Figure 1) in the ALP preoperatively. The main reason is that the cage height is determined by the intraoperative model test. Different cage height will result in different intervertebral space height. Therefore, the cortical screw holes are suggested to be manufactured after implanting the cage. Alternatively, ALP of different sizes is needed to be designed according to the anatomical parameters and clinical experience.
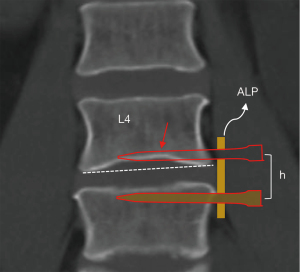
Second, the endplate morphology should be taken into consideration in designing the distance between the cortical screw holes (“h” in Figure 1) in the ALP. The shape of the endplate is defined as the concave endplate if the endplate demonstrates a smooth concave curvature (the inferior endplate of L4 in Figure 1) and the concave endplate accounts for 58.2% in lumbar spine (2). The height of ALP is 6 mm, so it is nearly impossible to change the direction of the cortical screws once the location of the ALP is determined. If the shape of the endplate is neglected, the cortical screw will cause iatrogenic endplate injury as is evident at L4 inferior endplate from Figure 1. And the endplate injury is one of the major factors causing cage subsidence (3).
Third, to improve the biomechanical property, the ALP is fixed by six screws in the vertebral body. Three screws are implanted in the same vertebral body from the left side. Whether or not those screws would damage the structure of the vertebral body or cause the vertebral fracture under stressed conditions would still need further investigation, especially for osteoporosis patients.
In conclusion, Dr. Huang et al. has presented a novel fixation option for the OLIF technique and it is much appreciated. We hope the aforementioned three suggestions here would be constructive to the article.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-5025/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang W, Tian Y, Ma X, et al. Biomechanical evaluation of a novel anatomical plate for oblique lumbar interbody fusion compared with various fixations: a finite element analysis. Ann Transl Med 2022;10:871. [Crossref] [PubMed]
- Wang Y, Battié MC, Videman T. A morphological study of lumbar vertebral endplates: radiographic, visual and digital measurements. Eur Spine J 2012;21:2316-23. [Crossref] [PubMed]
- Wu H, Shan Z, Zhao F, et al. Poor Bone Quality, Multilevel Surgery, and Narrow and Tall Cages Are Associated with Intraoperative Endplate Injuries and Late-onset Cage Subsidence in Lateral Lumbar Interbody Fusion: A Systematic Review. Clin Orthop Relat Res 2022;480:163-88. [Crossref] [PubMed]


