
A novel patient-specific 3D printed guide for accurate femoral derotation osteotomies: a case report
Highlight box
Key finding
• The application of a small 3D guide with uni-cortical K-wire placement for derotation osteotomies provides additional correction control during surgery and accurate outcome, while facilitating the surgical flow of this technically demanding procedure.
What is known and what is new?
• Femoral malrotation errors are prevalent after intramedullary nailing for femur fractures. Supposing fracture consolidation has occurred, only a derotation osteotomy can offer a solution, despite in situ nail interference.
• A novel case-based surgical technique using 3D technology planning and a 3D guide was presented to obtain an accurate correction and desired clinical outcome.
What is the implication, and what should change now?
• Primary or revision surgery for native axial malalignment or malrotation errors after nailing should be accurately performed. The threshold to use 3D technology for planning should therefore be low. Small 3D guides with uni-cortical pin fixation can ease derotation surgery technics with elegant nail exchange and accurate outcomes.
Introduction
The prevalence of evident rotational malalignment after intramedullary (IM) nailing for femoral fractures (pertrochanteric, subtrochanteric, diaphyseal) is broadly estimated on 2.3–35% (1,2). Due to the intraoperative closed reduction maneuver, it appears difficult to maintain control over the native rotation of the femur, both radiographically and clinically (1,3).
The most common malalignment after femoral IM nailing is internal rotation of the distal part resulting in increased femoral anteversion or femoral anteversion angle (FAVA) (normal value 15°±10°) (4,5). Relevant mechanical leg axis deviation might be expected in case of >20° side to side difference (6). However, increased femoral anteversion results in an elevated patellofemoral contract pressure, toeing-in during gait and anterior groin pain (1,3,7,8). This might severely impact the quality of life and the activity level of the ambulating patient (regardless of age) (1). Revision surgery can therefore be necessary after thorough imaged-based investigation by measuring the exact difference in FAVA angle on bilateral computed tomography (CT) scan (9). If noticed in the early postoperative phase (<4 weeks), a derotation over the non-consolidated fracture site can be performed with repositioning of the nail and locking screws. However, most axial malrotations become symptomatic in the later phase of rehabilitation because of altered gait (toeing-in/-out or abductor muscle malfunction) when fracture consolidation is almost reached (2,10). This urges the need for revision surgery in the form of a subtrochanteric or diaphyseal derotation osteotomy (1,3,4,9).
Femoral derotation osteotomies are technically challenging procedures for which careful preoperative CT-based planning of FAVA correction is key to successful outcome (1,9). Intraoperative translation of the planned correction seems difficult to obtain with the current surgical and measuring tools available, which leaves the effective correction subjected to the ‘eyeballing’ judgement of the surgeon (3).
With the increasing accessibility of preoperative 3D planning and printing in orthopaedics nowadays, patient specific instrumentation (PSI) can contribute to the improvement in performing femoral derotation osteotomies. The goal of this technology is to minimize perioperative tissue damage, to increase surgical accuracy and thereby improving function and quality of life, while minimizing the need for revision surgery. The authors present an alternative case-based derotation osteotomy technique using a patient-specific 3D printed guide in order to facilitate procedure technics and increase surgical accuracy (11). We present the following article in accordance with the CARE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1645/rc).
Case presentation
A 32-year-old woman was referred to our clinic with ongoing left groin pain. Three months earlier, she sustained a high energy fall resulting in a subtrochanteric femur fracture. This was treated with a long IM femoral nail (PFNA™, Synthes, Solothurn, Switzerland) elsewhere. Postoperatively, she developed a limping gait pattern and persistent pain during walking. Clinical examination revealed ‘toeing-in’ of the left limb during gait. In supine position, a notable axial malalignment towards increased femoral version was visible compared to the contralateral side with 46° FAVA on CT-scan (Figure 1).

3D planning and guide design
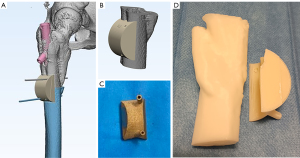
In order to measure the rotational error, a high-resolution bilateral CT-scan was obtained according to a specific protocol (slice thickness 0.5 mm, slice increment 0.2 mm, pixel size 0.29 mm, 120 kVp). The DICOM images were loaded into medical processing software Mimics Medical (Materialise NV, technologielaan 15, 3001 Leuven, Belgium) and the individual bones were segmented and converted into 3D STL (stereolithography) files. A mirrored version of the normal contralateral bone was superimposed over the malunited bone, which enabled evaluation of the deformity both intuitively and quantitatively (Figure 2A). Furthermore, the FAVA was measured as described by Waidelich et al. in the axial plane (12). Native femoral anteversion was 10° in the left femur and 46° in the operated right femur (Figure 2B). A corrective derotation osteotomy of 36° reduction in anteversion at the subtrochanteric level was simulated in 3-Matic (Materialise NV, Technologielaan 15, 3001 Leuven, Belgium), as bone fragments were reduced to their anatomical position (Figure 2C). Next, a patient-specific guide was designed, which matched the lateral femoral bone surface (Figure 3A). Correct guide placement was facilitated by specific post-traumatic marks in the subtrochanteric zone (Figure 3B). This guide determined the exact placement of two Kirschner wires (K-wires, 2 mm diameter); one above and one below the osteotomy. The direction of both K-wires was determined by the patient-specific implant in order that they were placed eccentrically in the thick anterior and posterior cortices without nail interference. After osteotomy, the derotation was accurate when both K-wires were finally in parallel position. The 3D guide was a disposable Aluminum (AlSi10Mg) device printed externally and sterilized onsite in an autoclave with saturated steam at 134 ℃ for 3.5 hours (Figure 3C). In order to facilitate correct guide placement, a phantom of the subtrochanteric femoral area and the guide was 3D printed in non-medical resin for perioperative use (Figure 3D).

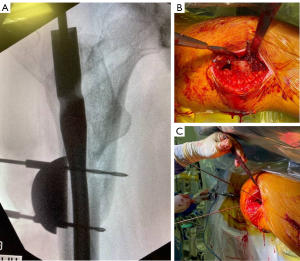
Surgical technique
The patient was positioned in dorsal decubitus on a traction table without traction. The same incisions were used with distal enlargement of the lag screw incision. Corresponding to a direct lateral approach to the proximal femur, the femoral subtrochanteric region was exposed by elevating the proximal vastus lateralis muscle. The lateral cortical bone was cleared from soft tissue for guide placement. The surgical 3D guide was fixed to the bone with two new 2.5 mm drill bits, perforating the thick cortex, without IM involvement (Figure 4). Position was checked with fluoroscopy. While keeping the guide in place, the distal locking screws, the lag screw and the PFNA nail were consequently removed at the level of the greater trochanter. Then, an IM rod (3×1,000 mm) was introduced into the femoral canal, while the guide was removed and the drill bits were replaced by 2.0 mm K-wires (Figure 4). The osteotomy was performed with a 1 mm sawblade oscillating saw and completed with a small chisel under fluoroscopic guidance. The IM rod prevented major antero-posterior or mediolateral displacement of the osteotomy. Next, the distal part was externally rotated for 36°, until the 2 K-wires were in parallel position (Figure 5A). This was confirmed by placement of a Hintermann retractor over the K-wires, also to maintain the planned correction during nail introduction (Figure 5B).

Next, a new long PFNA nail (Synthes, Solothurn, Switzerland) was introduced, using the same lag screw trajectory but new distal drillholes. In this way, the correction could be maintained with K-wires in situ while locking the nail.
From day one postoperatively, weight-bearing ‘as tolerated by the patient’ was permitted with two crunches. Six weeks after surgery the patient presented without pain and normal gait. Clinical examination showed bilateral similar rotations in supine position (Figure 6). A postoperative CT-scan at 3 months revealed a final anteversion (FAVA) of 10.1°, comparable to the contralateral side. Radiological consolidation was reached at 4 months with central location of the nail distally (Figure 7). At 6 months after the corrective osteotomy, the patient complained about irritation of the lag screw and proximal tip of the nail, so the revision nail was subsequently removed at this time.


All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of the manuscript and additional images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The here presented case-based surgical technique described a femoral derotation osteotomy to correct axial malrotation after primary IM nailing for a subtrochanteric fracture. The use of 3D planning and printing of a surgical guide for placement of 2 eccentrical K-wires provided the desired correction relative to the planning while facilitating surgical flow.
Continuous cortical fixation of the K-wires without interfering with nail exchange was considered to be a major advantage. Either central or eccentrical placement of the pins seems to be irrelevant to the amount of rotation needed before pins become parallel. Further, due to the compact design of the 3D guide, there was minimal need for periosteal stripping and soft tissue detachment as compared to other studies presenting 3D derotation guides (3,13). Besides fracture revision surgery, the concept of this 3D technique might be applicable for patients with excessive native ante-or retroversion of the femur too (14). Finally, who are low volume surgeons not familiar with rotational osteotomies might benefit most from this technique.
Downsides of this approach are the indisputable cost [3D medical software and guide manufacturing (150 euro)], and additional time for preoperative 3D planning and guide design. Further, an exact match of the guide with the lateral cortical bone is mandatory to avoid mal-positioning of the drill bits and K-wires. Providentially, the lateral subtrochanteric bone can easily be exposed by flipping over the vastus lateralis muscle anteriorly which makes this region anatomically appropriate for correct bony guide positioning. However, in general, smaller 3D guides have the advantage of minimizing soft tissue damage while increasing the risk of malpositioning due to reduced bony contact surface. Further, a cutting slot or additional guidance pin in the 3D guide might have facilitated an exact perpendicular bone cut to the mechanical axis of the femur. Finally, when malrotation is discovered in the early phase (<4 weeks) after fracture nailing, there is no need for an osteotomy but a derotation can be performed over the fracture site.
In case revision surgery for malrotation errors is indicated after fracture union, a derotation osteotomy should be performed after thorough CT-based preoperative planning (9). The application of a 3D guide with uni-cortical K-wire placement as presented in this case provides accurate correction control during this technically demanding procedure.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1645/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1645/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1645/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of the manuscript and additional images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Branca Vergano L, Coviello G, Monesi M. Rotational malalignment in femoral nailing: prevention, diagnosis and surgical correction. Acta Biomed 2020;91:e2020003. [PubMed]
- Jaarsma RL, Pakvis DF, Verdonschot N, et al. Rotational malalignment after intramedullary nailing of femoral fractures. J Orthop Trauma 2004;18:403-9. [Crossref] [PubMed]
- Oraa J, Beitia M, Fiz N, et al. Custom 3D-Printed Cutting Guides for Femoral Osteotomy in Rotational Malalignment Due to Diaphyseal Fractures: Surgical Technique and Case Series. J Clin Med 2021;10:3366. [Crossref] [PubMed]
- Buly RL, Sosa BR, Poultsides LA, et al. Femoral Derotation Osteotomy in Adults for Version Abnormalities. J Am Acad Orthop Surg 2018;26:e416-25. [Crossref] [PubMed]
- Cibulka MT. Determination and significance of femoral neck anteversion. Phys Ther 2004;84:550-8. [Crossref] [PubMed]
- Flury A, Hoch A, Hodel S, et al. No relevant mechanical leg axis deviation in the frontal and sagittal planes is to be expected after subtrochanteric or supracondylar femoral rotational or derotational osteotomy. Knee Surg Sports Traumatol Arthrosc 2023;31:414-23. [Crossref] [PubMed]
- Flury A, Hoch A, Andronic O, et al. Increased femoral antetorsion correlates with higher degrees of lateral retropatellar cartilage degeneration, further accentuated in genu valgum. Knee Surg Sports Traumatol Arthrosc 2021;29:1760-8. [Crossref] [PubMed]
- Liska F, von Deimling C, Otto A, et al. Distal femoral torsional osteotomy increases the contact pressure of the medial patellofemoral joint in biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 2019;27:2328-33. [Crossref] [PubMed]
- Kent ME, Arora A, Owen PJ, et al. Assessment and correction of femoral malrotation following intramedullary nailing of the femur. Acta Orthop Belg 2010;76:580-4. [PubMed]
- Flury A, Aregger F, Rahm S, et al. Subtrochanteric osteotomy in the management of femoral maltorsion results in anteroposterior malcorrection of the greater trochanter: computed simulations of 3D surface models of 100 cadavers. Hip Int 2022; Epub ahead of print. [Crossref] [PubMed]
- Jud L, Vlachopoulos L, Grob K. Correction of complex three-dimensional deformities at the proximal femur using indirect reduction with angle blade plate and patient-specific instruments: a technical note. J Orthop Surg Res 2021;16:427. [Crossref] [PubMed]
- Waidelich HA, Strecker W, Schneider E. Computed tomographic torsion-angle and length measurement of the lower extremity. The methods, normal values and radiation load. Rofo 1992;157:245-51. [Crossref] [PubMed]
- Fiz N, Delgado D, Sánchez X, et al. Application of 3D technology and printing for femoral derotation osteotomy: case and technical report. Ann Transl Med 2017;5:400. [Crossref] [PubMed]
- Hartigan DE, Perets I, Walsh JP, et al. Femoral Derotation Osteotomy Technique for Excessive Femoral Anteversion. Arthrosc Tech 2017;6:e1405-10. [Crossref] [PubMed]


