
A risk model to predict the mental health of older people in Chinese communities based on machine learning
Highlight box
Key findings
• This study designed a risk model based on machine learning that is useful for identifying older people with poor mental health.
What is known and what is new?
• Older people can experience a variety of psychological problems, which seriously affect their health of and increase the burden of treatment. Early screening can greatly improve the outcomes for older patients with mental health problems.
• We have developed a new predictive model that can be used to predict mental health problems in the elderly in the community. This model is easy to operate, low cost and widely suitable for aging.
What are the implications of this study, and what should change now?
• A new machine learning-based model to predict mental health problems in older people was constructed. This model is simple, easy to operate and can be used for self-examination at a low cost.
Introduction
The global population is experiencing aging. In 2000, there were 600 million older people worldwide, but by 2015, the number had climbed to 900 million (World Population Ageing. United Nations, 2015. Available at: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf, accessed 21 February 2021). In China, the Fifth National Population Census in 2000 showed that the over-65 age group accounted for 6.96% of the total population, which marked the beginning of China’s status as an aging society. In the Seventh National Population Census in 2010, the proportion of people aged 65 and over had risen to represent 13.50% of the total population. The United Nations Population Development Agency has predicted that the population aged over 65 in China will reach 334 million in 2050, making China the country with the largest population of older people in the world and bringing severe population aging-related challenges in the future (1).
Aging health not only includes all aspects of physical health, but also includes basic cognition, memory, emotional wellbeing, social interactions, and other aspects of mental health (2). Current mental health standards and specific disorders are not clearly defined, covering a wide range of issues, from the familiar anxiety and depression, to sleep disorders, mental disorders, as well as cognitive impairment and loneliness. In 2018, the Aging Health Service and Standardization Branch of the Chinese Geriatric Medical Research Society defined the mental health standards of the elderly in China. Mental health refers to the internal psychological harmony and consistency of the individual, and the stable mental state that is well adapted to the external. It includes five dimensions: cognitive efficacy, emotional experience, self-knowledge, interpersonal communication and adaptive ability (2). Among them, the elderly can maintain the basic daily cognitive function as the first criterion, is an important link to ensure the quality of life. The mental health status of older people is affected by a variety of factors, including genetics, physical health, personality, socioeconomic status, environment, and life experiences (3). However, older adults face unique challenges to their mental health, such as changes in their appearance and declines in physical and cognitive function (4-7). For example, older people are prone to chronic diseases, chronic pain, weakness, and other health problems (8,9), and are more likely to encounter stressful events such as the death of loved ones and a decline in socio-economic status due to retirement (10,11). These risk factors may cause an individual to experience social isolation and psychological distress, which can lead to the occurrence of psychological and mental disorders. Cognitive and emotional disorders also cannot be ignored in older people, with dementia, depression, and anxiety being the most prominent mental health problems in this demographic group (12).
The decline of the physiological and psychological systems is an inevitable and natural aging process. Compared to the physiological system, the psychological system is less affected by external conditions. The psychological system is more interventional, and can be more easily changed. Old age is not a linear, gradual stage of decline but a malleable stage of development. Hierarchical prevention and related intervention training can restore, maintain, and even improve the cognitive ability of older individuals, improve their mood, and alleviate their anxiety and depression symptoms. Furthermore, the psychological system can effectively slow down the process of physiological decline in old age (13,14). If the psychological problems of older people could be effectively predicted hierarchically, not only would the rates of recognition and detection of mental health problems improve, but medical resources could be reasonably arranged. Early prevention and precise intervention can help older people face the physiological and psychological changes of the aging process more actively and cope better with potential age-related risks and problems, thus allowing them to experience a high quality of life in old age.
Currently, it is difficult for general doctors diagnose anxiety, depression, and dementia in older people at the appropriate point in time (15). At present, there are several effective and reliable psychometric analysis tools for screening older people with anxiety, depression, or dementia. Among them are the Patient Health Questionnaire (PHQ)-9 depression screening scale, the Generalized Anxiety Disorder 7-item (GAD-7) screening scale, the AD8 Dementia Screening the Hamilton Anxiety and Depression Scales, and the Hospital Anxiety and Depression Scale (HADS) (16-20). However, the problem with using these tools is that they are time consuming and highly demanding. For older people, a variety of complex problems can arise in the process of filling out questionnaires, which makes this method extremely inconvenient. Furthermore, it is virtually impossible for general practitioners or specialists to manage the use of such tools, especially during very busy hours in the outpatient departments of hospitals or clinics in developing countries. In addition, some patients are even reluctant to answer a questionnaire because of their heavy psychological burden. As a result, appropriate diagnosis and treatment are initiated at an advanced stage of anxiety, depression and other mental illnesses, which leads to a higher incidence of associated morbidity and mortality. Therefore, there is an urgent need to develop automated prediction systems for the mental health of older people. Developing such systems would be of great help, not only in allowing general practitioners and specialists in all fields to screen patients for potential diseases, but also in improving the overall mental health of a society.
At present, artificial intelligence (AI) is often used to support the early detection of diseases, understand the progress of diseases, optimize drug selection and therapeutic doses, and discover new treatments (21). Machine learning (ML) is at the core of the AI era. It requires a large amount of input data to generate reliable results and a large amount of computing resources to process data in a timely manner. However, it has the advantages of being able to discover potential patterns in datasets and develop improved pre-diagnostic screening risk models to determine an individual’s susceptibility or risk of developing mental illness (22). Various sociodemographic factors and disease conditions, which are important factors influencing the development of mental health issues in older people, can be used as predictors in automated system development. We present the following article in accordance with the TRIPOD reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-23-200/rc).
Methods
Data collection
Data of 15,173 older people from each district and county of Shanxi province, China, who were surveyed for the 2019 ‘13th Five-Year Plan for Healthy Aging – Psychological Care for the Elderly Project’ of the National Health Commission of China, were collected. The ‘13th Five-Year Plan’ refers to the outline of the 13th Five-Year Plan for National Economic and Social Development of the People’s Republic of China, which covered the period from 2019 to 2020. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). During this period, the aging degree of the population continued to deepen, the number of older people, including those with disabilities, increased, and the rigid demand for health services for older people was constantly raised, which brought severe challenges to older people’s health services as well as changes in family structure. To actively deal with mental health problems in older people and to effectively maintain and promote the mental health of this age group, the Chronic Disease Center of China and the National Health Commission—under the guidance of the 13th Five-Year Plan for Healthy Aging—1,600 urban communities were selected according to their geographical distribution in 31 provinces (autonomous regions and municipalities directly under the central government) in 2019–2020. Inclusion criteria: permanent residents aged 65 and above in pilot communities (refers to registered and non-registered residents who have lived for more than half a year), poor, empty-nest, disabled, mentally retarded, family planning special families and elderly people living alone are mainly included. Exclusion criteria: this survey was conducted for all older people over 65 years of age in the pilot community. The survey was conducted as comprehensively as possible but on a voluntary basis. Investigation methods: a unified questionnaire was used to investigate the mental health status of the elderly people in the community. The investigation fully respects the individual wishes of the elderly and obtains informed consent. Under the leadership of the Department of Aging and Health of the National Health Commission, a national project working group was established under the leadership of the Chronic Disease Center of the China Center for Disease Control and Prevention, Project Executive Office. The provincial health administration department is responsible for organizing and implementing the standardization through the four links of project design, project implementation, personnel training and project supervision. The final sample in Shanxi province consisted of 15,079 participants, including 8,212 females and 6,867 males. The mean age of the participants was 71.95 years (standard deviation =6.01; range, 65–106 years), and the average level of education was 7.02 years (standard deviation =3.81; range, 0–21 years).
The Psychological Care for the Elderly Project conducted a cross-sectional mental health questionnaire, which assessed a number of sociodemographic factors, including sex, age, education level, family members and relationships, and diseases. Subsequently, the following three standardized questionnaires were conducted:
- The PHQ-9 depression screening scale, Mandarin Chinese version (Cronbach’s alpha =0.85). The PHQ-9 is a nine-item self-evaluation tool for depression based on the Diagnostic and Statistical Manual of Mental Disorders (fourth edition) which is half the length of other depression screening tools (23). Respondents of the PHQ-9 are asked to answer nine questions related to the frequency of their experiences of depressive symptoms over the last 2 weeks, using a 5-point scale from 0 (not at all) to 4 (almost every day). An example item is ‘Over the last 2 weeks, have you felt no or little interest doing anything?’ A higher score indicates a higher level of depression. In the present study, participants were classified into two categories: no depressive tendency (PHQ-9 score <5) and depressive tendency (PHQ-9 score ≥5).
- The GAD-7 screening scale, Mandarin Chinese version (GAD-7, Cronbach’s Alpha =0.91). The GAD-7 scale is a concise and effective method for evaluating generalized anxiety disorder in clinical practice (24). Participants are asked to answer seven questions related to how often they have experienced anxiety symptoms in the previous 2 weeks using a 5-point scale from 0 (none) to 4 (almost every day). An example item is: “Have you worried about all sorts of things in the last 2 weeks?” A higher score indicates a higher level of anxiety. In this study, participants were divided into two categories: non-anxious (GAD-7 score <5) and anxious (GAD-7 score ≥5).
- The AD8 Dementia Screening in Mandarin Chinese (Cronbach’s alpha =0.91). The AD8 scale is an eight-question visiting questionnaire developed by the University of Washington in 2005 and is used for the screening of very early dementia. The AD8 scale focuses on whether patients have experienced eight specific changes which could help family members to screen for dementia symptoms (25). Respondents are asked to answer eight questions using a 2-point scale, on which 0 is ‘no’ and 1 is ‘yes’. In this study, participants were divided into two categories: normal cognitive function (AD8 score <2) and possible cognitive impairment (AD8 score ≥2). In this study, the levels of anxiety, depression, and dementia in older people were assessed based on PHQ-9, GAD-7, and AD8 results, respectively.
Statistical analysis
Different ML algorithms can handle health-related classification problems very effectively (26). In this study, three different ensemble learning classifiers were used and their performances evaluated to select the best classifier for the selected feature set. Ensemble learning adopts the idea of integration to combine multiple weak learners to form a strong learner. Because a single weak learner may make prediction errors, and the combination of multiple learners can correct the errors, ensemble learning is often better than a single machine learning method. In this study, the three algorithms with the best ensemble learning performance, random forest (RF), Extreme Gradient Boosting (XGBoost) and Light Gradient Boosting Machine (LightGBM), were used to model the above data respectively, and then some features with high contribution to the model were selected to model the three models again. Finally, the two modeling methods were compared and analyzed to verify the selected influencing factors. Let’s start with these three models.
Overview of RF: RF model was proposed by Breiman in 2001 (27). Based on Bagging integrated learning method, RF can be used for classification, regression and other problems. It uses the self-lifting sampling method to extract multiple samples from the original sample, models each bootstrap sample, and then combines the predictions of multiple decision trees to obtain the final prediction result through voting. A study has proved that RF has high prediction accuracy, good tolerance to outliers and noise, and is not easy to overfit (27). In the training stage, RF uses bootstrapping sampling to collect several different sub-training data sets from the input training data set, so as to train several different decision trees in turn. In the prediction stage, the RF votes the prediction results of multiple internal decision trees to obtain the final value. Advantages are high accuracy, not easy to overfit, good anti-noise ability, can process high-dimensional data without feature selection, can process various types of data without normalization of data sets, fast training speed, can obtain the importance ranking of variables, easy to realize parallelization. The disadvantage is that the number of trees is large, the training needs a large space and a long time, and the model is not easy to explain because of the black box model. RF was compared in this study as baseline versus subsequent gradient lift predictor (28).
Boosting, a machine learning technique that can be used for regression and classification problems, generates a weak prediction model at each step and adds it to the overall model by weight. If the generation of the weak prediction model in each step is based on the Gradient direction of the loss function, they are called Gradient boosting, and the gradient Boosting algorithm based on CART Decision Tree is called gradient boosting decision tree (GBDT). Gradient lifting is widely regarded as the latest technology in table data prediction and many winning algorithms in the field of machine learning use gradient lifting (29). XGBoost’s full name is eXtreme Gradient Boosting, which was proposed by Dr. Tianqi Chen of the University of Washington in 2014 to further expand the gradient lift tree. Compared with traditional GBDT, XGBoost algorithm uses parallel, multi-core and distributed computation in training. It can converge on the training set much faster, resulting in significantly shorter training times, more than 10 times faster than common kits. XGBoost algorithm adopts greedy algorithm to slice the training data by using the optimal features of the tree structure recursively selected from the root node. Let L and R be the sample sets placed relative to each other around the split point. The segmentation with maximum information gain is the optimal segmentation of nodes. The calculation formula is as follows (30):
is the score of left subtree, is the score of right subtree, is the score that is undivided, λ is the complexity cost of adding new leaf nodes, when Gain <0, give up the partition.
Despite XGBoost is faster than other machine learning algorithms, the number of iterations of XGBoost is related to the feature dimension, and each iteration traverse the entire data set, which consumes a lot of memory. Secondly, XGBoost needs to traverse the segmentation points when calculating the information gain, which is costly and low in efficiency.
For these problems, LightGBM is a framework that realizes GBDT algorithm, which supports efficient parallel training, has the advantages of faster training speed, lower memory consumption, better accuracy, and supports distributed and rapid processing of massive data. LightGBM optimizes the traditional GBDT algorithm as follows: Based on Histogram, the decision tree algorithm; the use of Gradient-based One-Side Sampling (GOSS) can reduce a large number of data instances with only small gradients and save time and space overhead. Exclusive Feature Bundling (EFB) can be used to bundle many mutually exclusive features into a single feature for dimension reduction: leaf growth strategies of leaf-wise with depth restriction; directly support the categorical feature; supports efficient parallelism and cache hit ratio optimization (31).
Evaluation index
For the binary classification problem, the following situations exist when comparing the predicted results and the real categories of the test set samples. True positive (TP), the actual is positive and the prediction is positive; false positive (FP), actually negative but predicted negative; false negative (FN), actually positive but predicted negative; true negative (TN), the actual negative prediction is negative. For the classification model, the larger the number of TP and TN, the smaller the number of FP and FN, the more accurate the model prediction is proved. However, what the confusion matrix counts is the number of sample points, and the model cannot be weighed by the number alone. Therefore, four evaluation indexes of the model are extended from the confusion matrix: Accuracy, Recall, Precision and F1 score.
ROC curve is also called “receiver operating characteristic curve”. The horizontal coordinate of the curve is false positive rate (FPR) and the vertical coordinate is true positive rate (TPR). The curve mainly involves four points and a line: the first point is (0,1), in which case FPR =0, TPR =1, that is, FN =0, FP =0, then the classifier can divide all samples according to the correct category. The second point is (1,0). In this case, FPR =1 and TPR =0, the classifier classifies all samples according to wrong categories, and the classifier has the worst performance. The third point is (0,0), in which case FPR =0, TPR =0, then the classifier’s prediction results for all samples are negative. The fourth point is (1,1), in which case FPR =0 and TPR =0, the classifier’s prediction results for all samples are positive. Thus, the closer the ROC curve is to point (0,1), the better the classifier effect will be. The value of AUC is the area covered by the ROC curve. It can be seen that the larger the AUC, the better the classification effect of the classifier.
To find redundant features and minimize feature dimensions, and to build the simplest model, this study used the feature attribution framework for the Shapley value (32). This value is suitable for complex models, such as artificial neural networks and gradient lifting machines (33). The Shapley value originates in game theory and is obtained by dividing the predicted results of each sample into contributions for each constituent eigenvalue by estimating the differences between models with a subset of the eigenspace. In this study, features were sorted according to their Shapley value, and the relationship between the number of features used to construct the model and the model’s performance was studied. Partial dependence plot (PDP) (34,35) can be used to analyze the importance of individual features and marginalize other features that are not of interest.
In this study, features were sorted according to their Shapley value, and the relationship between the number of features used to construct the model and the model’s performance.
Results
Establishment of the prediction model
The researchers of this study were committed to building a simple and convenient model which could be applied to a grassroots health census or self-examination to make a rapid graded prediction of mental illness for older people in the community.
First, two classification problems were proposed: the general population versus the critical and at-risk population, and the at-risk population versus the general and critical population. Initially, there were 18 features of predictable outcomes in our data (Table 1). However, due to the problem posed by the skip structure of the questionnaire (for example, when answering ‘childless’ for A5, A6 would be skipped and A7 would be directly answered), the rationality and coherence of the respondents needed to be considered. Subsequently, 5 of the features were deleted and the classifier was finally constructed using 13 features.
Table 1
| Step involved | Description |
|---|---|
| Data collection/features | A1: ID number |
| A2: Years of education | |
| A3: Marital status | |
| A4: Do you have any religious beliefs? | |
| A5: Who do you currently live with? | |
| A6: Do you have any children? | |
| A7: Are you satisfied with your relationship with your children? | |
| A8: Are you satisfied with your relationship with your spouse? | |
| A9: How many friends do you have? Do you have close friends from whom you can get support and help? | |
| A10: Do you get along well with your friends? | |
| A11: How well do you get along with your neighbours? | |
| A12: Have you been diagnosed with any of the following diseases by the hospital? | |
| A13: What is your main daily work currently? | |
| A14: What are your main entertainment and leisure activities? | |
| A15: Is there a senior citizen area near your home? Do you attend activities often? | |
| A16: Do you think older people are a burden on society? | |
| A17: If you experience a major event in your life, can you recover quickly? | |
| A18: In general, are you satisfied with your life at present? | |
| Features after selection | A2; A3; A4; A5; A10; A11; A12; A13; A14; A15; A16; A17; A18 |
Detailed feature information is shown in Table 1. It was hoped that algorithmic learning would obtain representations of sociodemographic and disease conditions in groups of older adults suffering from anxiety, depression, and dementia. Thirteen questionnaire variables were used to train and test the ML algorithm according to the process described in the “Classification model” section, and two classification problems were solved. In total, six models were trained. When building models using classification algorithms, we solved the problem of unbalanced data classes by using random down-sampling. Since the ML approach is best suited to balanced datasets, it was necessary to consider the problem of unbalanced data classification, especially when the amount of data was limited.
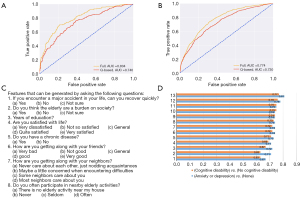
The ratio of training to testing set was 8:2. The classification results of the test set, which include the area under the receiver operating characteristic curve (AUC), accuracy, recall, and F measures (F1 scores) for cross-validation, are reported in Table 2. In the test set, the AUC range for the classifiers was 0.79 to 0.85. In the problem, however, the LightGBM algorithm showed higher accuracy than both the baseline and XGBoost, making it a stronger predictive model. This finding laid the foundation for us to further refine the usability of the method.
Table 2
| Algorithm | Class | AUC | Recall | Precision | F1 score |
|---|---|---|---|---|---|
| LightGBM | General population or at-risk population | 0.8242 | 0.7518 | 0.7098 | 0.7302 |
| XGBoost | General population or at-risk population | 0.8060 | 0.6839 | 0.6972 | 0.6905 |
| RandomForest | General population or at-risk population | 0.7961 | 0.5976 | 0.7134 | 0.6504 |
| LightGBM | Risk group or general marginal group | 0.8466 | 0.8083 | 0.7760 | 0.7918 |
| RandomForest | Risk group or general marginal group | 0.8104 | 0.8455 | 0.7390 | 0.7886 |
| XGBoost | Risk group or general marginal group | 0.8267 | 0.7920 | 0.7702 | 0.7810 |
AUC, area under the receiver operating characteristic curve; XGBoost, eXtreme Gradient Boosting; LightGBM, Light Gradient Boosting Machine.
Factors affecting the effect of model classification
Different factors have different degrees of influence on the model. In the next part of the study, we make an effort to identify the key factors affecting the mental health of older people by Shapley analysis. As shown in Figure 1, Shapley analysis showed that the most predictive features affecting the classification of the general population model were A16 (the sense of social value) and A18 (life satisfaction).
Partial dependence graphs were further constructed for A16 and A18 (Figures 2,3, respectively), to capture the nonlinear association of each feature. The PDPs allowed the influence of the features on the prediction results of the model to be observed when different values changed. A16 was the most influential factor in the model, which reflected the phenomenon that the older people feel that they are a burden to society, the lower their mental health level. The phenomenon reflected in A18 was that the higher the life satisfaction of the elderly, the higher the level of mental health.


Study of the applicability of the model in different age groups
In addition to achieving high accuracy, our method was highly applicable a previous study has shown that age is related to the probability of mental diseases in older people (36). To further prove that our model could be used for older people of different ages, we constructed a model based on age group. We divided the population in the questionnaire data into three groups according to age: 61–70 years, 71–80 years, and above 80 years. In the general population versus the critical and risk population, and the risk population versus the general population and critical population, three new LightGBM classification predictors were trained according to the data of the three age groups. Finally, a new test set that included all three age groups was used. The classification results of the test set are reported in Tables 3,4.
Table 3
| Group | AUC | Recall | Precision | F1 score |
|---|---|---|---|---|
| 61–70 years | 0.7898 | 0.7455 | 0.7389 | 0.7422 |
| 71–80 years | 0.8176 | 0.6643 | 0.6942 | 0.6789 |
| >80 years | 0.7679 | 0.6465 | 0.7571 | 0.6974 |
AUC, the area under the receiver operating characteristic curve.
Table 4
| Group | AUC | Recall | Precision | F1 score |
|---|---|---|---|---|
| 61–70 years | 0.7642 | 0.6437 | 0.6756 | 0.6593 |
| 71–80 years | 0.7693 | 0.6481 | 0.7000 | 0.6731 |
| >80 years | 0.7496 | 0.6334 | 0.6786 | 0.652 |
AUC, the area under the receiver operating characteristic curve.
Through the four quantitative indicators, it was found that the models trained on different age groups had similar effects when tested against the same age-wide dataset, and there was no significant difference.
Building the simplest model
After communicating with the project staff who collected the data, it was found that many of the participants were not well informed when confronted with the questionnaire. There were two reasons for this: firstly, many older people were unwilling to fill in some of the questions for reasons relating to privacy; and secondly, the excessive setting of questionnaire topics increased the difficulty of filling out the questionnaire and thus reduced the enthusiasm of participants, leading to carelessness and major errors in information. Therefore, reducing the number of features and making our method simpler became the next goal of this research.
The order of feature importance was determined according to Shapley value, and to study the relationship between the number of features and model accuracy, the number of model features was reduced with the feature with the smallest Shapley value. As shown in Figure 4, in the two problems (general vs. critical and at-risk; at-risk vs. general and critical), the AUC value of the model increased from 0.6 to about 0.8 as the number of features increased. With eight features, the model achieved an AUC of 0.74. Following the principle of simplifying the model and questionnaire, eight simple questions that older people could answer were finally used to evaluate the performance of the model. As shown by the ROC curve, when the number of features dropped to eight, the model’s accuracy decreased compared with that of the full-question model. However, the similar AUC and greatly simplified questionnaire process still showed that the model had certain reference value for the diagnosis and screening of mental health of older people. The results are shown in (Figure 4).
Discussion
The standards of mental health for older people are: normal cognitive function, positive emotional stability, appropriate self-evaluation, harmonious interpersonal communication, and good adaptability (2). By predicting the mental health problems of older people by grade, screening them in advance, and carrying out graded prevention and precise intervention at an early stage, we can improve the quality of life of older people, reduce medical costs, and promote healthy aging. Researchers from the fields of medicine and engineering are working together to address this challenge using ML technology, which offers new hope for the development of automated disease diagnosis systems.
In this study, we strived to use ML techniques to predict some of the most prevalent age-related psychological issues, namely anxiety, depression, and dementia, from sociodemographic and medical factors. A large number of older patients (n=15,079) were interviewed and screened for anxiety, depression, and cognition. This dataset was used for predictive modeling. During the COVID-19 pandemic, ML was used by Flesia et al. to predict people’s stress perception (37). Another study conducted by Cho et al. attempted to use ML techniques to build predictive models for depression screening of 9,488 community residents, not just older people (38). It is not uncommon for ML models to be used to predict mental health-related problems, and the main data sources include imaging and biological markers. The disadvantages of ML models are their high cost and operational difficulty. At present, however, studies using demographic characteristics and specifically targeting older patients, especially for systematic grading prediction, are rare in the literature. Moreover, most studies using ML tend to only study the interrelationships between features and do not focus on building high-quality usable models.
Our model showed a certain degree of interpretability. As shown in Figure 4, the eight questions identified by the model covered psychological resilience, attitude to aging, life satisfaction, years of schooling, chronic diseases, social participation, and social support networks in relation to the mental health of older people. Psychological resilience in the elderly people refers specifically to the ability of the elderly to face common difficulties (such as physical decline, cognitive decline, and social and economic status decline) and special difficulties (such as the death of a spouse) with a positive attitude and strong willpower, which allows them to counter the adverse effects of risk factors, and achieve social adaptation and good physical and mental health. Mental resilience is closely related to mental health and plays an important role in successful aging (39). Attitude to aging has a complex psychological structure, which can be divided into multiple levels from different perspectives. Previous studies have shown that an individual’s aging attitude is closely related to their mental health and has a significant predictive effect on depression (40). As a positive indicator of mental health of older people, life satisfaction is negatively correlated with anxiety and depression (41). Long-term chronic diseases have a great impact on the mental health of older people. For example, older patients with hypertension usually experience headaches, dizziness, fatigue, and other symptoms, which can result in anxiety, depression, paranoia, and other negative emotions and psychological disorders (42). Older patients with diabetes are prone to develop depression, anxiety, and other negative emotions and psychological disorders due to the need for long-term strict dietary control, long-term drug use, and the associated economic burden. Arthritis, causes physical and psychological pain to older patients and profoundly affects their daily life and emotional experience; consequently, it is often accompanied by anxiety, depression, and other negative emotions and psychological disorders. Older patients with chronic obstructive pulmonary disease have symptoms including repeated cough and dyspnea, which limits their physical activity and can easily lead to anxiety, depression, other negative emotions, and even psychological disorders (43). In this study, we study the association between chronic disease and mental health in older people with PDPs, and we found that there was a non-linear dependency between various chronic diseases and depression and dementia scores. Years of schooling, social support networks, and social engagement also have a significant impact on the mental health of older adults (11,44-47).
In summary, the eight risk factors extracted from the model, like many other risk factors, have been confirmed in previous studies to have an impact on the mental health of older people. However, they have generally only been analyzed as influencing factors, with scattered information and a lack of practical application value. Through ML, this study has developed a predictive model which can be better applied to clinical practice and exert greater value. In addition, in the past, we have focused more on treating mental health problems in older adults than on the benefits that positive emotions can bring. This study found that the mental resilience and aging attitude of the elderly to mental health more proves this point, suggesting that we should strengthen the elderly mental health services to pay more attention to and support the positive emotions of the elderly.
Conclusions
This study used data from the ‘Psychological Care Project’ of The National Health Commission of China in 2019, which was large and representative. The data were not affected by the COVID-19 pandemic because they were collected the year before. The LightGBM-based full-feature classification prediction model we constructed had a good predictive performance, with an AUC as high as 0.846 (95% CI: 0.8251–0.8681). After simplification, the eight-question model based on older people also achieved satisfactory accuracy. Our model can be used in multiple age groups, and its accuracy is not affected by age. Using PDP and the Shapley value, we have also identified many risk factors affecting the mental health of older people, including psychological resilience, attitude to aging, life satisfaction, years of schooling, chronic diseases, and social support networks. Our findings remind social workers that it is particularly important to care for older people, to improve their psychological endurance, to provide them with more social support, and to improve their disease symptoms. Moreover, they also provide new ideas for our future research, which, through the use of ML, will study the complex relationship between mental resilience and mental illness with more ideal methods for quantifying mental resilience. Moreover, they also provide new perspectives for our future research in which we will study the complex relationship between mental resilience and mental illness with more ideal methods to quantify mental resilience by using ML.
To sum up, our model is simple and easy to operate, and can be used for self-examination at a low cost. The main limitation of this study is that most of the participants were active older people and the data only reflected problems at the community level. However, it is difficult for older people with serious diseases and disabilities to participate in surveys. Furthermore, many older adults experience shame in talking about poor family social relations and poor psychological conditions, so the survey may have underestimated the actual prevalence rate of mental illnesses, and systematic bias may exist. Therefore, further prospective studies based on A broader practical test, particularly in other regional populations, are needed to assess the clinical efficacy of the model we developed. The limitation of this study is that we used cross-sectional questionnaire data, and we need to further study and apply the prediction effect of the validated model.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the TRIPOD reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-23-200/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-200/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-200/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jiang Q, Feng Q. Editorial: Aging and health in China. Front Public Health 2022;10:998769. [Crossref] [PubMed]
- Aging Health Service and Standardization Branch CGMRS. Mental health assessment guidelines for the elderly. Chin J Gerontology 2018;16:40.
- Zhong BL, Chen SL, Tu X, et al. Loneliness and Cognitive Function in Older Adults: Findings From the Chinese Longitudinal Healthy Longevity Survey. J Gerontol B Psychol Sci Soc Sci 2017;72:120-8. [Crossref] [PubMed]
- Baltes PB. Theoretical propositions of life-span developmental psychology: On the dynamics between growth and decline. Developmental Psychology 1987;23:611-26. [Crossref]
- Martin KA, Leary MR, Rejeski WJ. Self-Presentational Concerns in Older Adults: Implications for Health and Well-Being. Basic and Applied Social Psychology 2000;22:169-79. [Crossref]
- Deng FM, Luo XD, Lang HL, et al. Role of amyloid beta-protein in postoperative cognitive dysfunction and effect of huperzine A on cognitive dysfunction in aged rats. Chinese Journal of Gerontology 2018;38:6034-6.
- Verhaeghen P, Salthouse TA. Meta-analyses of age-cognition relations in adulthood: estimates of linear and nonlinear age effects and structural models. Psychol Bull 1997;122:231-49. [Crossref] [PubMed]
- Aldwin CM, Igarashi H, Gilmer DF. Health, Illness, and Optimal Aging: Biological and Psychosocial Perspectives. International Journal of Health Care Quality Assurance 2013;172.
- Alexopoulos GS. Depression in the elderly. Lancet 2005;365:1961-70. [Crossref] [PubMed]
- Rosnick CB, Small BJ, McEvoy CL, et al. Negative life events and cognitive performance in a population of older adults. J Aging Health 2007;19:612-29. [Crossref] [PubMed]
- Litwin H. Social network type and morale in old age. Gerontologist 2001;41:516-24. [Crossref] [PubMed]
- Depp C, Vahia IV, Jeste D. Successful aging: focus on cognitive and emotional health. Annu Rev Clin Psychol 2010;6:527-50. [Crossref] [PubMed]
- Schaie WK. Midlife Influences Upon Intellectual Functioning in Old Age. International Journal of Behavioral Development 1984;7:463-78. [Crossref]
- Almeida OP. Prevention of depression in older age. Maturitas 2014;79:136-41. [Crossref] [PubMed]
- Mavis E, Pat M. Diagnosis of depression in elderly patients. Adv Psychiatr Treat 2000;6:49-56. [Crossref]
- Hendry K, Green C, McShane R, et al. AD-8 for detection of dementia across a variety of healthcare settings. Cochrane Database Syst Rev 2019;3:CD011121. [Crossref] [PubMed]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. [Crossref] [PubMed]
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. [Crossref] [PubMed]
- Herrmann N, Mittmann N, Silver IL. A validation study of the geriatric depression scale short form. Int J Geriatr Psychiatr 1996;11:457-60. [Crossref]
- Snaith RP. The Hospital Anxiety And Depression Scale. Health Qual Life Outcomes 2003;1:29. [Crossref] [PubMed]
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med 2019;25:44-56. [Crossref] [PubMed]
- Shatte ABR, Hutchinson DM, Teague SJ. Machine learning in mental health: a scoping review of methods and applications. Psychol Med 2019;49:1426-48. [Crossref] [PubMed]
- Xu Y, Wu H, Xu YF. Application of the Patient Health Questionnaire Depression Scale (PHQ-9) in the elderly in the community—reliability and validity analysis. Shanghai Psychiatry 2007;19:257-9.
- Gong Y, Zhou H, Zhang Y, et al. Validation of the 7-item Generalized Anxiety Disorder scale (GAD-7) as a screening tool for anxiety among pregnant Chinese women. J Affect Disord 2021;282:98-103. [Crossref] [PubMed]
- Galvin JE, Roe CM, Powlishta KK, et al. The AD8: a brief informant interview to detect dementia. Neurology 2005;65:559-64. [Crossref] [PubMed]
- Melillo P, Jovic A, De Luca N, et al. Automatic classifier based on heart rate variability to identify fallers among hypertensive subjects. Healthc Technol Lett 2015;2:89-94. [Crossref] [PubMed]
- Breiman L. Random forests. Mach Learn 2001;45:5-32. [Crossref]
- Beura S, Majhi B, Dash R, et al. Classification of mammogram using two-dimensional discrete orthonormal S-transform for breast cancer detection. Healthc Technol Lett 2015;2:46-51. [Crossref] [PubMed]
- Fernández-Delgado M, Cernadas E, Barro S, et al. Do we need hundreds of classifiers to solve real world classification problems? J Mach Learn Res 2014;15:3133-81.
- Chen T, Guestrin C. Xgboost: A scalable tree boosting system. In: Proceedings of the 22nd Acm Sigkdd International Conference on Knowledge Discovery and Data Mining. ACM; 2016:785-94.
- Dwyer DB, Falkai P, Koutsouleris N. Machine Learning Approaches for Clinical Psychology and Psychiatry. Annu Rev Clin Psychol 2018;14:91-118. [Crossref] [PubMed]
- Noh B, Youm C, Goh E, et al. XGBoost based machine learning approach to predict the risk of fall in older adults using gait outcomes. Sci Rep 2021;11:12183. [Crossref] [PubMed]
- Liang W, Luo S, Zhao G, et al. Predicting Hard Rock Pillar Stability Using GBDT, XGBoost, and LightGBM Algorithms. Mathematics 2022;8:5.
- Guidotti R, Monreale A, Ruggieri S, et al. A Survey of Methods for Explaining Black Box Models. ACM Computing Surveys 2018;51:5-9. (CSUR).
- Goldstein A, Kapelner A, Bleich J, et al. Peeking Inside the Black Box: Visualizing Statistical Learning with Plots of Individual Conditional Expectation. Journal of Computational and Graphical Statistics 2015;24:1-5. [Crossref]
- Costa PT Jr, McCrae RR. Trait psychology comes of age. Nebr Symp Motiv 1991;39:169-204. [PubMed]
- Flesia L, Monaro M, Mazza C, et al. Predicting Perceived Stress Related to the Covid-19 Outbreak through Stable Psychological Traits and Machine Learning Models. J Clin Med 2020;9:3350. [Crossref] [PubMed]
- Cho SE, Geem ZW, Na KS. Predicting Depression in Community Dwellers Using a Machine Learning Algorithm. Diagnostics (Basel) 2021;11:1429. [Crossref] [PubMed]
- Ding YP, Shi CH. Application of resilience theory in successful aging research. Chinese Journal of Gerontology 2015;3.
- Tang D, Yan L, Wang DH. The influence of aging attitude on mental health. Chinese Journal of Clinical Psychology 2014;1:159-62.
- Yan DJ, Yu AY. Anxiety, depression and life satisfaction in older adults. Chinese Journal of Gerontology 2011;31:1847-8.
- Li MX, Ma ZW, Liu JZ. Analysis of psychological status and personality characteristics of essential hypertension patients. Chinese Journal of Health Psychology 2005;13:338-9.
- Yang S, Xu Y, Peng W, et al. Chinese herbal medicine for symptoms of depression and anxiety in chronic obstructive pulmonary disease: A systematic review and meta-analysis. Complement Ther Clin Pract 2021;45:101470. [Crossref] [PubMed]
- Belo P, Navarro-Pardo E, Pocinho R, et al. Relationship Between Mental Health and the Education Level in Elderly People: Mediation of Leisure Attitude. Front Psychol 2020;11:573. [Crossref] [PubMed]
- Douglas H, Georgiou A, Westbrook J. Social participation as an indicator of successful aging: an overview of concepts and their associations with health. Aust Health Rev 2017;41:455-62. [Crossref] [PubMed]
- Poulin J, Deng R, Ingersoll TS, et al. Perceived family and friend support and the psychological well-being of American and Chinese elderly persons. J Cross Cult Gerontol 2012;27:305-17. [Crossref] [PubMed]
- Xie L, Shen Y, Wu Y, et al. The impact of retirement on mental health. Int J Health Plann Manage 2021;36:1697-713. [Crossref] [PubMed]
(English Language Editor: J. Reylonds)



