
Tissue expansion techniques in reconstructive surgery: a 10-year bibliometric analysis
Highlight box
Key findings
• A bibliometric analysis was performed on studies investigating tissue expansion over the past 10 years. Keywords related to breast reconstruction appeared most frequently. “Activated controlled expansion” was one of the burst keywords that lasted until 2021.
What is known and what is new?
• Tissue expansion is one of the most widely used reconstructive techniques and many studies have been performed in this field. To our knowledge, this study is the first bibliometric analysis of literature related to tissue expansion.
What is the implication, and what should change now?
• This study provides an overview of the influential authors, countries, institutions, and journals on tissue expansion, and reveals the main research directions and hot spots. Relevant researchers can investigate patient-activated controlled expansion as a future research direction.
Introduction
Tissue expansion (TE) was first described by Neumann for ear reconstruction in 1957 (1). This technique was subsequently extended to breast reconstruction by Radovan in the late 1970s (2) and was reported by Becker in 1987 (3). It has been widely applied in plastic and reconstructive surgery. TE can be subdivided into internal TE and external TE. Conventionally, internal TE is performed in two stages. In the first stage, a tissue expander is placed in the subcutaneous region close to the area requiring reconstruction. The volume of the expander increases as saline solution is regularly—usually once or twice a week—injected into it, leading to skin growth. In the second stage, the expander is removed and additional skin is used for reconstruction (4). External TE promotes wound closure by exerting continuous tension to the wound margins. It reduces the risk of infection and avoids delaying definitive reconstruction but only partly achieves the expansion that can be attained with internal TE (5).
Compared with other techniques such as skin graft or flap transplantation, internal TE provides well-vascularized tissue that is similar in both color and texture to the surrounding skin tissue. The reduction of donor-site morbidity can also be achieved (6). However, it also has some significant disadvantages, including the lengthy duration of TE, the need for multiple-staged operations, and temporary discomfort (7). Moreover, for patients with large defects, the amount of skin provided by internal TE is often insufficient because of the limited regenerative capacity of skin (8). Due to its effectiveness and simplicity, TE has garnered keen interest among researchers in terms of its indications, complications, and improvements over the past decades (9). A larger number of related manuscripts are published every year. At present, there are no comprehensive reports about the publication trends, influential journals and authors, or hots pots and frontiers in this field.
Bibliometrics is an interdisciplinary subject that applies mathematical and statistical methods to analyze scientific literature (10) and has attracted the attention of academic researchers in recent years. Many researchers have employed this method to study rheumatic system diseases (11), cardiovascular system diseases (12), nervous system diseases (10), and cancer (13). Compared to reviews or meta-analyses, bibliometrics offers researchers information about the contributions of countries, institutions, authors, and journals (14). Research hot spots and frontiers can also be revealed.
In this study, we retrieved and collected the reviews and articles related to the surgical application of internal TE from the Web of Science Core Collection (WOSCC) database. Then, a quantitative and visual analysis was conducted using CiteSpace and VOSviewer. This study aimed to provide an overview of this field and help relevant doctors and researchers develop new directions for future TE research.
Methods
Data source and search strategy
The WOSCC is a leading global citation database that includes the Science Citation Index Expanded (SCIE), Social Sciences Citation Index (SSCI), and Emerging Sources Citation Index (ESCI), among others. We performed a literature search using WOSCC, and the data were downloaded within 1 day (March 1, 2022). The search strategy was as follows: Topic (TS) = (“tissue expansion” OR “tissue expander*” OR “skin expansion” OR “skin expander*” OR expander* OR expansion*) AND Web of Science Categories = (Surgery) AND Web of Science Index = (Science Citation Index Expanded OR Social Sciences Citation Index) AND Language = English AND Document types = (Article and Review). The publication year was confined to the period from 2012 to 2021. To ensure relevance, H.G and C.Y independently screened the titles and abstracts of all documents. Eligible documents were clinical studies and reviews related to internal TE. Any disagreements between the authors were resolved by consulting DW.
Data processing and bibliometric analysis
All retrieved documents were exported and saved as plain text with full record and references. Data including countries, institutions, journals, authors, references, total citations, and keywords were included in our study. Microsoft Excel 2021 was used to format these data into tables and to draw a line graph. CiteSpace (version 5.8 R3) was used to draw network maps as well as for country analysis, institution analysis, and burst detection. There are several nodes and lines in these maps. The size of the nodes represents the number of documents, while the thickness of the line represents the closeness of cooperation between countries or institutions. The outer purple circle denotes the centrality >0.1. Generally, a node with a centrality >0.1 is referred to as a key point. A keyword co-occurrence visual analysis was performed using VOSviewer (version 1.6.18). In the corresponding network map, the size of the nodes is determined by the keyword occurrence frequency.
Results
Analysis of publication trends
In total, 1,085 documents on TE were included in our study. The number of publications showed a slight fluctuation. The year with the largest number of documents published was 2017 (n=126). Thereafter, the number of publications fell and reached a low of 95 in 2020 (Figure 1).
Analysis of countries and institution distribution
A total of 1,030 institutions from 45 countries were involved in TE research. As shown in Table 1, the United States was the most productive country with 618 articles, and China was the second most productive country with 120 articles, followed by Italy (n=66). The United States, Italy, England, and Canada were the 4 countries with a centrality greater than 0.1 (circled in purple in Figure 2).
Table 1
| Rank | Country | Article, n | Centrality |
|---|---|---|---|
| 1 | USA | 618 | 0.65 |
| 2 | China | 120 | 0.06 |
| 3 | Italy | 66 | 0.15 |
| 4 | South Korea | 45 | 0.00 |
| 5 | England | 43 | 0.29 |
| 6 | Canada | 23 | 0.12 |
| 7 | Turkey | 19 | 0.00 |
| 8 | Japan | 18 | 0.00 |
| 9 | Germany | 15 | 0.06 |
| 10 | The Netherlands | 8 | 0.00 |

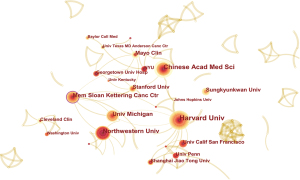
The top 10 institutions with the largest number of documents are listed in Table 2. The visualization map of the major institutions is shown in Figure 3. Harvard University (n=50) was the leading institution. The second and third institutions ranked by the number of documents were the Chinese Academy of Medical Sciences and Northwestern University, respectively. The top 3 institutions ranked by centrality were the Memorial Sloan-Kettering Cancer Center (0.10), Harvard University (0.07), and the University of Michigan (0.07).
Table 2
| Rank | Institution | Country | Articles, n | Centrality |
|---|---|---|---|---|
| 1 | Harvard University | USA | 50 | 0.07 |
| 2 | Chinese Academy of Medical Sciences | China | 36 | 0.03 |
| 3 | Northwestern University | USA | 32 | 0.03 |
| 4 | Memorial Sloan-Kettering Cancer Center | USA | 27 | 0.10 |
| 5 | The University of Michigan | USA | 24 | 0.07 |
| 6 | Stanford University | USA | 22 | 0.05 |
| 7 | Mayo Clinic | USA | 22 | 0.02 |
| 8 | Sungkyunkwan University | South Korea | 20 | 0.00 |
| 9 | The University of California, San Francisco | USA | 16 | 0.00 |
| 10 | The University of Pennsylvania | USA | 14 | 0.00 |
Analysis of journals
The 1,085 articles were published in 81 journals. Of these, the top 10 journals published 839 (77.3%) (Table 3). Plastic and Reconstructive Surgery (n=243, 22.4%), Annals of Plastic Surgery (n=210, 19.4%), and Journal of Plastic Reconstructive and Aesthetic Surgery (n=121, 11.2%) published the highest number of articles. These journals also ranked as the top 3 in terms of total citations. Notably, the Annals of Surgical Oncology had 1,051 total citations, which exceeded that of the Journal of Craniofacial Surgery and Aesthetic Plastic Surgery.
Table 3
| Rank | Journal | Articles, n | IF | Total citations, n |
|---|---|---|---|---|
| 1 | Plastic and Reconstructive Surgery | 243 | 5.169 | 8,408 |
| 2 | Annals of Plastic Surgery | 210 | 1.763 | 2,600 |
| 3 | Journal of Plastic Reconstructive and Aesthetic Surgery | 121 | 3.022 | 1,652 |
| 4 | Journal of Craniofacial Surgery | 64 | 1.172 | 313 |
| 5 | Aesthetic Plastic Surgery | 57 | 2.708 | 622 |
| 6 | Annals of Surgical Oncology | 42 | 4.339 | 1,051 |
| 7 | Journal of Plastic Surgery and Hand Surgery | 29 | 1.295 | 464 |
| 8 | Gland Surgery | 28 | 2.160 | 328 |
| 9 | Aesthetic Surgery Journal | 25 | 4.485 | 292 |
| 10 | EJSO | 20 | 4.037 | 430 |
TE, tissue expansion; IF, impact factor.
Analysis of authorship
A total of 4,157 authors contributed to TE research. Table 4 presents the top 10 most productive authors and the top 10 most cited authors. Kim JYS had the most published articles in this field (n=31), followed by Fine NA (n=23), and Mum GH (n=23). He also ranked first in the analysis of cited authors. Although Nahabedian MY and Serletti JM published 16 and 14 articles, respectively they both had a high number of citations.
Table 4
| Rank | Author | Articles, n | Citations, n |
|---|---|---|---|
| Most productive | |||
| 1 | Kim JYS | 31 | 1,039 |
| 2 | Fine NA | 23 | 582 |
| 3 | Mum GH | 23 | 333 |
| 4 | Sbitany H | 20 | 604 |
| 5 | Pusic AL | 18 | 706 |
| 6 | Lee GK | 18 | 198 |
| 7 | Bang SI | 17 | 105 |
| 8 | Nahabedian MY | 16 | 729 |
| 9 | Xie F | 15 | 147 |
| 10 | Li QF | 15 | 142 |
| Most cited | |||
| 1 | Kim JYS | 31 | 1,039 |
| 2 | Nahabedian MY | 16 | 729 |
| 3 | Pusic AL | 18 | 706 |
| 4 | Serletti JM | 14 | 694 |
| 5 | Fischer JP | 13 | 673 |
| 6 | Nelson JA | 11 | 611 |
| 7 | Sbitany H | 20 | 604 |
| 8 | Fine NA | 23 | 582 |
| 9 | Wilkins EG | 13 | 551 |
| 10 | Choi M | 14 | 510 |
Analysis of cocitation and citation
There were 14,308 cited references included in this study. If 2 articles are cited simultaneously by a third one, then the relationship between the 2 articles is called co-citation. Table 5 shows the top 10 most cocited references (15-24). Among these references, Chun et al. (15) ranked first, with 143 cocitations, followed by Albornoz et al. (16) and Breuing et al. (17), with 133 and 116 cocitations, respectively.
Table 5
| No. | Title | Author | Journal | Cocitations, n | Year |
|---|---|---|---|---|---|
| 1 | Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications | Chun et al. | Plastic and Reconstructive Surgery | 143 | 2010 |
| 2 | A paradigm shift in US breast reconstruction: increasing implant rates | Albornoz et al. | Plastic and Reconstructive Surgery | 133 | 2013 |
| 3 | Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings | Breuing et al. | Annals of Plastic Surgery | 116 | 2005 |
| 4 | Acellular dermis-assisted breast reconstruction | Spear et al. | Aesthetic Plastic Surgery | 114 | 2008 |
| 5 | Acellular human dermis implantation in 153 immediate two-stage tissue expander breast reconstructions: determining the incidence and significant predictors of complications | Antony et al. | Plastic and Reconstructive Surgery | 102 | 2010 |
| 6 | Predicting complications following expander/implant breast reconstruction: An outcomes analysis based on preoperative clinical risk | McCarthy et al. | Plastic and Reconstructive Surgery | 99 | 2008 |
| 7 | Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm) | Salzberg et al. | Annals of Plastic Surgery | 98 | 2006 |
| 8 | A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: Part I: A prospective analysis of early complications | Cordeiro et al. | Plastic and Reconstructive Surgery | 94 | 2006 |
| 9 | A meta-analysis of human acellular dermis and submuscular tissue expander breast reconstruction | Kim et al. | Plastic and Reconstructive Surgery | 92 | 2012 |
| 10 | The effect of acellular dermal matrix use on complication rates in tissue expander/implant breast reconstruction | Lanier et al. | Annals of Plastic Surgery | 90 | 2010 |
TE, tissue expansion.
Analysis of keywords
The top 10 high-frequency keywords are listed in Table 6. Among them, “tissue expander” and “tissue expansion” were expected because they were the search terms. Apart from these 2 keywords, keywords with a frequency >150 were “complications” (n=348), “breast reconstruction” (n=323), “outcomes” (n=227), “mastectomy” (n=185), “acellular dermal matrix” (n=168), and “tissue expansion” (n=151).
Table 6
| No. | Keywords | Frequency |
|---|---|---|
| 1 | Complications | 348 |
| 2 | Breast reconstruction | 323 |
| 3 | Outcomes | 227 |
| 4 | Tissue expander | 225 |
| 5 | Mastectomy | 185 |
| 6 | Acellular dermal matrix | 168 |
| 7 | Tissue expansion | 151 |
| 8 | Reconstruction | 147 |
| 9 | Surgery | 138 |
| 10 | Cancer | 114 |
As shown in Figure 4, these keywords were classified into 5 different clusters, represented by 5 colors. The blue cluster comprised the keywords related to complications, implant, TE, and risk factors, while the yellow cluster was mainly related to acellular dermal matrix, Alloderm, coverage, etc. The keywords of the green cluster were related to reconstruction, defects, repair, head, neck, face, etc. The keywords of red cluster were largely associated with outcomes, cancer, skin-sparing mastectomy, nipple-sparing mastectomy, radiotherapy, and patient satisfaction. In addition, the purple cluster was the smallest cluster and covered keywords related to prepectoral breast reconstruction.
The top 25 keywords with the strongest citation bursts are shown in Figure 5. “Capsule formation” had the strongest burst (4.55), which emerged in 2012 and ended in 2014. “Surgical site infection”, “tissue expander/implant”, “bilateral prophylactic mastectomy”, and “activated controlled expansion” were the burst keywords that lasted until 2021.

Discussion
General information
In this study, we combined bibliometrics with visualization to analyze data from 1,085 articles published for the period of 2012–2021. The publication trend fluctuated slightly, which may be attributed to the different research directions across countries or institutions. The number of documents reflects the scientific research levels of a country or institution (25). The analysis of countries’ distribution indicated that the United States took the lead in TE research. Nearly all productive institutions came from this country. Furthermore, Italy, England, and Canada had a centrality greater than 0.1, which indicated that they made considerable contributions to TE research. Although China was ranked second (Table 1), its centrality was 0.06, suggesting the absence of collaboration with other countries.
The analysis of journals can help identify the zone of core journals. Plastic and Reconstructive Surgery, Annals of Plastic Surgery, and Journal of Plastic Reconstructive and Aesthetic Surgery were the top 3 journals in terms of the number of documents and citations. Thus, numerous relevant studies could be found in these journals. Annals of Surgical Oncology also deserves the attention of researchers because of its high number of citations. Based on the number of published articles and total citations, Kim JYS can be considered a particularly influential author in this field.
Through reference cocitation analysis, researchers can gain a better understanding of the basis of subject research (26). “Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications” was the most co-cited reference. The author found that postoperative seroma and infection were related to the introduction of ADM (15). “A paradigm shift in US breast reconstruction: increasing implant rates” ranked second. This study reported that the growth in implant use might popularize immediate breast reconstruction (16). The third most cocited article was “Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings”, which was published in 2005 by Breuing et al. (17). This study was the first to introduce the AlloDerm slings technique. These documents laid the foundation for TE research.
Research directions, hotspots, and frontiers
Analyzing keywords in documents can reveal research directions, hotspots, and frontiers in a particular research area. Although we divided the keywords into 5 clusters (Figure 4), the main research directions of TE can be summarized as nonbreast applications and breast reconstruction. According to the keyword co-occurrence analysis, the effect of ADM on the complication rates after breast reconstruction is the current hotspot. The keywords burst analysis indicated that patient-activated controlled expansion might be a future research direction for TE.
TE has been a well-established technique for soft tissue reconstruction. As presented in Figure 4, its nonbreast applications mainly include ear reconstruction, scalp reconstruction, facial defect reconstruction, and soft tissue defect reconstruction in other regions of the body. For ear reconstruction, TE provides an expanded skin flap to cover the framework and is usually accomplished in 3 stages (27,28). In the first stage, a tissue expander is placed subcutaneously in the retroauricular area. The second-stage surgery involves ear reconstruction using an autologous costal cartilage upon completion of TE (29). Tragus and concha construction is performed in the third stage (Figure 6).

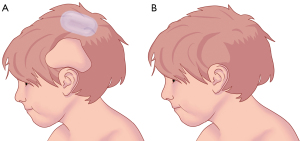
A hairless scalp can result in a severe psychological burden on patients, and TE is a good choice for hair restoration (30). The subgaleal and subcutaneous planes are the 2 recommended planes for tissue expander implantation (31). After full expansion, the expanded flap is used to repair the defects (Figure 7).
Facial defects secondary to trauma, burn, and tumor resection can lead to both physical and functional difficulties. TE offers an excellent color and texture match for the reconstruction of defects. One of the most frequently adapted flaps is the expanded forehead flap (32,33). The first-stage surgery involves the expander insertion, and the second-stage surgery involves the expander removal and forehead flap transfer. The distal portion of the flap is used to reconstruct facial defects, and the pedicle is cut off in the third stage (Figure 8). The trunk and limbs are also potential body parts for tissue expander insertion (34,35).

According to the 2020 cancer statistics, breast cancer is the most commonly diagnosed cancer in females worldwide, accounting for about 11.7% of all new cancer cases (36). At present, surgical resection is one of the main treatment strategies. For women undergoing partial or total mastectomy, breast reconstruction is a good method to improve their aesthetic outcomes, satisfaction, and quality of life (37). There have been many innovations and different-sized tissue expanders developed in breast reconstruction over the past few decades. Radovan introduced the first modern tissue expander consisting of a balloon and a port in 1976 (38), and Austed introduced the self-inflating tissue expander in 1977 (39). Then, in 1982, Radovan presented his experience of using the temporary tissue expander for breast reconstruction (2). McGhan Medical (Allergan) produced a tissue expander in different sizes, which allowed for the preferential expansion of the lower pole of the breast to reconstruct a natural-looking breast (40,41). The application of ADM for the breast was first introduced in 2005 (17), and 2 years later, Widgerow developed a tissue expander with an external infusion pump controlled by patients (42). However, the pump increased the risk of infection.
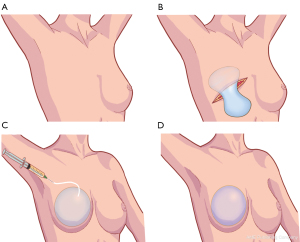
In 2011, the results of a feasibility study of the Aeroform system, known as patient-activated controlled expansion, were reported (43) (Figure 9). The tissue expander/implant-based breast reconstruction can be classified based on the location of the implant into either dual-plane subpectoral breast reconstruction or prepectoral breast reconstruction. In the first stage, a tissue expander is placed above or below the pectoralis major muscle, which is replaced with an implant in the second stage (Figure 10) (44). Subpectoral breast reconstruction is the current standard procedure for tissue expander/implant-based breast reconstruction. This procedure requires a sufficient amount of skin and muscle to cover the tissue expander. However, the elevation of the pectoralis may cause animation deformities, muscle spasms, chest tightness, and pain (45). As a less invasive procedure, prepectoral breast reconstruction has become popular in recent years. Its advantages include the elimination of animation deformities and muscle spasms. Studies have also shown that it is associated with less pain, is time-saving, and provides excellent aesthetic outcomes (46-48). Candidates for prepectoral breast reconstruction should have well-vascularized skin flaps and sufficient fat depots for fat grafting based on the concept of a bioengineered breast (49).
Due to the lack of lower pole coverage of the implant, subpectoral breast reconstruction involves a risk of implant migration and exposure. The introduction of ADM provides a solution to these problems. It also improves aesthetic results, especially in the inframammary fold position and the inferior breast contours (50). Despite the aforementioned advantages, the increase in complication rates is of concern. A meta-analysis performed by Kim et al. demonstrated that ADM-assisted tissue expander breast reconstruction had a higher incidence of postoperative complications. The total complication rate was higher in patients with ADM (15.4%) than in those without ADM (14%), and ADM doubled the risk of infection (23). Smith et al. found that the use of ADM was significantly associated with postoperative complications (51). Dikmans et al. likewise observed increased complication rates of wound infection, wound dehiscence exposure, and skin necrosis in patient reconstructions with ADM (52). A similar result was reported in a recent multicenter randomized controlled trial (RCT) (53). Although the complication rate in patients who received immediate implant-based breast reconstruction with ADM showed no statistical difference compared to that in patients without ADM, the total number of complications was higher in the ADM group. Overall, the use of ADM appears to increase complications in breast reconstruction. These advantages and disadvantages must be weighed judiciously for patients undergoing ADM-assisted reconstruction so that reconstructive surgeons can make an optimal choice. Further, more RCTs should be conducted to obtain high-level clinical evidence.
Traditional breast TE requires the use of a saline-based tissue expander. A serial percutaneous injection is administered weekly or biweekly by surgeons in the clinic, which is uncomfortable and time-consuming, and may hinder patients from undergoing breast reconstruction (54). The AeroForm System consists of an implantable tissue expander containing a compressed carbon dioxide reservoir and a handheld control device. Patients can manually release a predetermined volume of carbon dioxide gas using the controller under the direction of surgeons. This patient-activated controlled expansion eliminates the need for saline injections and can be performed in any location. In 2011, Connell reported the results of a clinical study on the AeroForm System (43); this was a proof-of-concept study and required further investigation. Three Australian clinical trials, including Patient Activated Controlled Expansion I (PACE I), Patient Activated Controlled Expansion II (PACE II) and Study of AeroForm Tissue Expander for Breast Reconstruction (ASPIRE), indicated that the AeroForm System is time saving, needle free, safe, and effective (43,54-56). Data from the Patient Controlled Tissue Expansion for Breast Reconstruction (XPAND) study revealed significantly shorter expansion and overall reconstructive times (57). These were also confirmed in the subsequent XPAND II study (58). However, the available literature remains inconclusive, and thus, additional clinical trials are required to provide an evidence base for clinical decision-making.
To our knowledge, this is the first bibliometric analysis of TE in clinical surgery. However, there were some limitations in our study that should be noted. First, this study is based on the WOSCC database. Some high-impact articles might have been excluded because they were not included in this database. Second, due to the limitation of the search terms, a few relevant articles were inevitably missed. Finally, we only limited the literature type to articles and reviews. Influential studies published in the form of letters, meeting abstracts, and proceeding papers might have been overlooked.
Conclusions
In this study, we used the bibliometric method to analyze 1,085 documents published on TE from 2012 to 2021. Despite its various indications, TE was mainly applied for breast reconstruction over the past 10 years. The effect of ADM on complication rates after breast reconstruction is the current hotspot of TE in surgery. Patient-activated controlled expansion might be a future direction for TE research.
Acknowledgments
Funding: This study was supported by the National Natural Science Foundation of China (No. 82072191 to CL), Shanghai Municipal Key Clinical Specialty (No. shslczdzk00901 to CL), the China Postdoctoral Science Foundation Grant (No. 2018M630449 to CL).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3643/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Neumann CG. The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear. Plast Reconstr Surg (1946) 1957;19:124-30. [Crossref] [PubMed]
- Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 1982;69:195-208. [Crossref] [PubMed]
- Becker H, Maraist F. Immediate breast reconstruction after mastectomy using a permanent tissue expander. South Med J 1987;80:154-60. [Crossref] [PubMed]
- De La Cruz Monroy MFI, Kalaskar DM, Rauf KG. Tissue expansion reconstruction of head and neck burn injuries in paediatric patients - A systematic review. JPRAS Open 2018;18:78-97. [Crossref] [PubMed]
- Choi YK, Mehta ST, Luo J, et al. Management of Large Pediatric Wound Defects Using a Continuous External Tissue Expander. Plast Reconstr Surg Glob Open 2021;9:e3723. [Crossref] [PubMed]
- Karagergou E, Papas A, Foroglou P, et al. Management of the complications of tissue expansion during a 5-year period (2005-2010). J Plast Surg Hand Surg 2012;46:167-71. [Crossref] [PubMed]
- Azzi JL, Thabet C, Azzi AJ, et al. Complications of tissue expansion in the head and neck. Head Neck 2020;42:747-62. [Crossref] [PubMed]
- Zhou SB, Zhang GY, Xie Y, et al. Autologous Stem Cell Transplantation Promotes Mechanical Stretch Induced Skin Regeneration: A Randomized Phase I/II Clinical Trial. EBioMedicine 2016;13:356-64. [Crossref] [PubMed]
- Langdell HC, Taskindoust M, Levites HA, et al. Systematic Review of Tissue Expansion: Utilization in Non-breast Applications. Plast Reconstr Surg Glob Open 2021;9:e3378. [Crossref] [PubMed]
- Ismail II, Saqr M. A Quantitative Synthesis of Eight Decades of Global Multiple Sclerosis Research Using Bibliometrics. Front Neurol 2022;13:845539. [Crossref] [PubMed]
- Zhang C, Feng X, Wang C, et al. Bibliometric analysis of scientific publications in rheumatology journals from China and other top-ranking countries between 2007 and 2017. PeerJ 2019;7:e6825. [Crossref] [PubMed]
- Ma D, Guan B, Song L, et al. A Bibliometric Analysis of Exosomes in Cardiovascular Diseases From 2001 to 2021. Front Cardiovasc Med 2021;8:734514. [Crossref] [PubMed]
- Hu S, Alimire A, Lai Y, et al. Trends and Frontiers of Research on Cancer Gene Therapy From 2016 to 2020: A Bibliometric Analysis. Front Med (Lausanne) 2021;8:740710. [Crossref] [PubMed]
- Zhang J, Song L, Xu L, et al. Knowledge Domain and Emerging Trends in Ferroptosis Research: A Bibliometric and Knowledge-Map Analysis. Front Oncol 2021;11:686726. [Crossref] [PubMed]
- Chun YS, Verma K, Rosen H, et al. Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications. Plast Reconstr Surg 2010;125:429-36. [Crossref] [PubMed]
- Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131:15-23. [Crossref] [PubMed]
- Breuing KH, Warren SM. Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings. Ann Plast Surg 2005;55:232-9. [Crossref] [PubMed]
- Spear SL, Parikh PM, Reisin E, et al. Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg 2008;32:418-25. [Crossref] [PubMed]
- Antony AK, McCarthy CM, Cordeiro PG, et al. Acellular human dermis implantation in 153 immediate two-stage tissue expander breast reconstructions: determining the incidence and significant predictors of complications. Plast Reconstr Surg 2010;125:1606-14. [Crossref] [PubMed]
- McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 2008;121:1886-92. [Crossref] [PubMed]
- Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg 2006;57:1-5. [Crossref] [PubMed]
- Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg 2006;118:825-31. [Crossref] [PubMed]
- Kim JYS, Davila AA, Persing S, et al. A meta-analysis of human acellular dermis and submuscular tissue expander breast reconstruction. Plast Reconstr Surg 2012;129:28-41. [Crossref] [PubMed]
- Lanier ST, Wang ED, Chen JJ, et al. The effect of acellular dermal matrix use on complication rates in tissue expander/implant breast reconstruction. Ann Plast Surg 2010;64:674-8. [Crossref] [PubMed]
- Wang Y, Jiang L, Li B, et al. Management of Chronic Myeloid Leukemia and Pregnancy: A Bibliometric Analysis (2000-2020). Front Oncol 2022;12:826703. [Crossref] [PubMed]
- Ai Y, Xing Y, Yan L, et al. Atrial Fibrillation and Depression: A Bibliometric Analysis From 2001 to 2021. Front Cardiovasc Med 2022;9:775329. [Crossref] [PubMed]
- Zhang Q, Quan Y, Su Y, et al. Expanded retroauricular skin and fascial flap in congenital microtia reconstruction. Ann Plast Surg 2010;64:428-34. [Crossref] [PubMed]
- Wang Y, Zhang J, Liang W, et al. Ear Reconstruction with the Combination of Expanded Skin Flap and Medpor Framework: 20 Years of Experience in a Single Center. Plast Reconstr Surg 2021;148:850-60. [Crossref] [PubMed]
- Tripathee S, Xiong M, Zhang J. Microtia Ear Reconstruction Using Tissue Expander and Autologous Costal Cartilage: Our Experience and Comparing Two Age Groups. World J Plast Surg 2019;8:324-30. [PubMed]
- Shin D, Kim YH, Song HG, et al. Serially expanded flap use to treat large hairless scalp lesions. Arch Craniofac Surg 2019;20:408-11. [Crossref] [PubMed]
- Shin H, Shin J, Lee JY. Scarred scalp reconstruction with a rectangular expander. Arch Craniofac Surg 2020;21:184-7. [Crossref] [PubMed]
- Zhu S, Liu Y, Zang M, et al. Facial Defect Reconstruction Using the True Scarless Pre-Expanded Forehead Flap. J Craniofac Surg 2018;29:1154-60. [Crossref] [PubMed]
- Dong W, Yang Q. Reconstruction of Facial Defects with Three-Stage Frontal Expanded Bipedicled Flaps. J Craniofac Surg 2019;30:175-7. [Crossref] [PubMed]
- Wooten KE, Ozturk CN, Ozturk C, et al. Role of tissue expansion in abdominal wall reconstruction: A systematic evidence-based review. J Plast Reconstr Aesthet Surg 2017;70:741-51. [Crossref] [PubMed]
- Arain AR, Cole K, Sullivan C, et al. Tissue expanders with a focus on extremity reconstruction. Expert Rev Med Devices 2018;15:145-55. [Crossref] [PubMed]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Maisel Lotan A, Ben Yehuda D, Allweis TM, et al. Comparative Study of Meshed and Nonmeshed Acellular Dermal Matrix in Immediate Breast Reconstruction. Plast Reconstr Surg 2019;144:1045-53. [Crossref] [PubMed]
- Radovan C. Adjacent flap development using expandable silastic implants. Paper Presented at Annual Meeting of the American Society of Plastic and Reconstructive Surgeons 1976. Boston.
- Austad ED, Rose GL. A self-inflating tissue expander. Plast Reconstr Surg 1982;70:588-94. [Crossref] [PubMed]
- Harless C, Jacobson SR. Current strategies with 2-staged prosthetic breast reconstruction. Gland Surg 2015;4:204-11. [PubMed]
- Morrison KA, Ascherman BM, Ascherman JA. Evolving Approaches to Tissue Expander Design and Application. Plast Reconstr Surg 2017;140:23S-9S. [Crossref] [PubMed]
- Widgerow AD, Murdoch M, Edwards G, et al. Patient-controlled expansion: applying a new technique to breast reconstruction. Aesthetic Plast Surg 2007;31:299-305. [Crossref] [PubMed]
- Connell AF. Patient-activated controlled expansion for breast reconstruction with controlled carbon dioxide inflation: a feasibility study. Plast Reconstr Surg 2011;128:848-52. [Crossref] [PubMed]
- Colwell AS, Taylor EM. Recent Advances in Implant-Based Breast Reconstruction. Plast Reconstr Surg 2020;145:421e-32e. [Crossref] [PubMed]
- Casella D, Kaciulyte J, Lo Torto F, et al. "To Pre or Not to Pre": Introduction of a Prepectoral Breast Reconstruction Assessment Score to Help Surgeons Solving the Decision-Making Dilemma. Retrospective Results of a Multicenter Experience. Plast Reconstr Surg 2021;147:1278-86. [Crossref] [PubMed]
- Haddock NT, Kadakia Y, Liu Y, et al. Prepectoral versus Subpectoral Tissue Expander Breast Reconstruction: A Historically Controlled, Propensity Score-Matched Comparison of Perioperative Outcomes. Plast Reconstr Surg 2021;148:1-9. [Crossref] [PubMed]
- Walia GS, Aston J, Bello R, et al. Prepectoral Versus Subpectoral Tissue Expander Placement: A Clinical and Quality of Life Outcomes Study. Plast Reconstr Surg Glob Open 2018;6:e1731. [Crossref] [PubMed]
- Tomita K, Yano K, Nishibayashi A, et al. Effects of Subcutaneous versus Submuscular Tissue Expander Placement on Breast Capsule Formation. Plast Reconstr Surg Glob Open 2015;3:e432. [Crossref] [PubMed]
- Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral Implant-Based Breast Reconstruction: Rationale, Indications, and Preliminary Results. Plast Reconstr Surg 2017;139:287-94. [Crossref] [PubMed]
- DeLong MR, Tandon VJ, Farajzadeh M, et al. Systematic Review of the Impact of Acellular Dermal Matrix on Aesthetics and Patient Satisfaction in Tissue Expander-to-Implant Breast Reconstructions. Plast Reconstr Surg 2019;144:967e-974e. [Crossref] [PubMed]
- Smith JM, Broyles JM, Guo Y, et al. Human acellular dermis increases surgical site infection and overall complication profile when compared with submuscular breast reconstruction: An updated meta-analysis incorporating new products☆. J Plast Reconstr Aesthet Surg 2018;71:1547-56. [Crossref] [PubMed]
- Dikmans RE, Negenborn VL, Bouman MB, et al. Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol 2017;18:251-8. [Crossref] [PubMed]
- Lohmander F, Lagergren J, Roy PG, et al. Implant Based Breast Reconstruction With Acellular Dermal Matrix: Safety Data From an Open-label, Multicenter, Randomized, Controlled Trial in the Setting of Breast Cancer Treatment. Ann Surg 2019;269:836-41. [Crossref] [PubMed]
- Ascherman JA, Zeidler KR, Jacoby A, et al. Carbon Dioxide versus Saline Tissue Expanders: Does It Matter?. Plast Reconstr Surg 2016;137:31-5. [Crossref] [PubMed]
- Connell TF. Results from the ASPIRE study for breast reconstruction utilizing the AeroForm™ patient controlled carbon dioxide-inflated tissue expanders. J Plast Reconstr Aesthet Surg 2015;68:1255-61. [Crossref] [PubMed]
- Connell TF. Patient-activated controlled expansion for breast reconstruction using controlled carbon dioxide inflation: confirmation of a feasibility study. Plast Reconstr Surg 2014;134:503e-11e. [Crossref] [PubMed]
- Ascherman JA, Zeidler K, Morrison KA, et al. Carbon Dioxide-Based versus Saline Tissue Expansion for Breast Reconstruction: Results of the XPAND Prospective, Randomized Clinical Trial. Plast Reconstr Surg 2016;138:1161-70. [Crossref] [PubMed]
- Ascherman JA, Zeidler K, Morrison KA, et al. Results of XPAND II: A Multicenter, Prospective, Continued-Access Clinical Trial Using the AeroForm Tissue Expander for Two-Stage Breast Reconstruction. Plast Reconstr Surg 2020;145:21e-9e. [Crossref] [PubMed]
(English Language Editors: A. Kassem and J. Gray)





