Intensive care unit strain should not rush physicians into making inappropriate decisions, but merely reduce the time to the right decisions being made
Deaths in the intensive care unit (ICU) are preceded in 53% to 90% of cases by a decision to withhold or withdraw life-sustaining therapies (1-3). The most common reasons justifying this decision include the patient’s age, previous autonomy, comorbidities, expected future quality of life, diagnosis at admission, non-response to maximal therapy and multi-organ failure (1,3,4).
Decision-making in end-of-life situations is influenced by numerous others factors, such as resource availability and the surrounding environment (5), the use of intensive communication strategies (3,6), multidisciplinary care teams (7), institutional culture (8), cultural differences between countries (9), religious beliefs of the physicians (4), ICU family conferences (i.e., VALUES approach) (2), the presence or not of surrogate decision-makers (10) and ethics consultations (11).
Another factor that is garnering increasing attention is how the dynamic nature of the ICU may impact on patient outcome. Kerlin et al. (12) defined “ICU capacity strain” using three measures, each calculated at the time of discharge from the ICU, namely census, admissions, and acuity. Census includes a count of all patients spending at least 2 hours in the ICU each day, standardized to the mean of the ICU to account for differences in ICU size. Admissions correspond to the proportion of the daily census that comprises new admissions on that day, and takes account of possible differences in the intensity of resources expended on newly admitted versus previously admitted ICU patients. Finally, acuity is calculated as the average predicted probability of death of the other patients in the ICU, based on individual MPM0-III (Mortality Probability Model III) scores calculated on the day of admission. These three metrics all stem from a conceptual model of ICU capacity strain (13), and have been shown to be independently associated with ICU physicians’ and nurses’ rating of daily workload, thus supporting their construct validity (12,14).
In their recent paper, Hua et al. investigated the effects of ICU strain on time to death for patients with and without limitations in life-sustaining therapy (15). Increases in the three metrics of ICU capacity strain during the first 3 days of ICU admission were associated with a shorter time to placement of DNR (Do Not Resuscitate) orders, a shorter time to death among patients who had limitations in life-sustaining therapy and who died in the ICU, as well as a shorter time to ICU discharge among patients who survived the initial ICU stay but subsequently died during the same hospitalization.
The main limitation of this retrospective study conducted by Hua et al. (15) is the fact that there was no evaluation of how the end-of-life decisions were made, nor was there any evaluation of the influence of ICU capacity strain on family satisfaction, for example, or on the quality of dying and death (QODD) (16) as assessed by the families, physicians and nurses.
In addition to the difficulties highlighted by Hua and co-workers, several other quandaries exist surrounding end-of-life decision-making. Firstly, physicians are often unaware of the patients’ preferences regarding end-of-life care, because the clinical state of the patient prevents them from expressing their desires (e.g., coma, shock, mechanical ventilation, sedation). Secondly, the lack of a designated surrogate (17) or the failure to recognize a suitable reference person (18), a high prevalence of anxiety, depression and post-traumatic stress disorder (PTSD) in family members of critically ill patients (19) and high levels of burnout syndrome among ICU nurses and physicians (20-22) are further factors that may hinder the end-of-life decisional process.
The findings of Hua et al. suggest that physician behaviours in this regard can be influenced by what might be termed “organisational constraints”. In view of the retrospective nature of the study, it is impossible to tell whether the decisions were ultimately the “right” decision, as far as the patient was concerned (in terms of quality of the end-of-life), or as far as the family (satisfaction, PTSD) or caregiving teams (burnout) were concerned. Indeed, in Hua’s study, there is no evidence to indicate that the decisions were anything other than appropriate. In theory, it is probably always possible to make end-of-life decisions more quickly. However, it must be remembered that healthcare decisions, especially one as critical as an end-of-life decision, must always be made in the interest of the patient who is present, i.e. the patient that the physician is currently caring for, and not in the interest of a putative future patient who hasn’t yet been admitted. The management of one patient should not be influenced, and above all, should not be hastened, to safeguard the interests of other patients who require care and may be waiting to take the bed.
Current French legislation, notably the so-called “Leonetti law” dated 22 April 2005 (23) relating to patient rights at end-of-life, is particularly laudable in this regard, in that the collegial decision-making process that it imposes is designed to examine all the reasons that might incite physicians to withhold or withdraw life-saving therapies. It helps physicians to resist the temptation to withdraw therapy for the proverbial “wrong reasons”, such as the need “to free up” an ICU bed or for economic reasons. Our patients and their families expect physicians to make care-related decisions that are respectful of, and faithful to the patient, based on arguments that focus on the patient and their healthcare project. This expectation forms the foundation of the trust that patients and their families place in physicians, particularly in difficult situations such as end-of-life. Indeed, it is indefensible that such an important decision regarding the care of a patient should be taken on the basis of organisational or economic constraints.
It is certainly necessary to protect against situations of this type, which could lead to decisions that may be taken hastily, due to outside pressures such as bed availability or high capacity strain. Two possible ways to anticipate these difficulties are to implement advance care planning (ACP), and to consolidate the position of the critical care physician as an external consultant, before the patient is admitted to the ICU.
In the same way as many people plan how to dispose of their estate by drawing up a last will and testament, planning for healthcare emergencies or indeed, chronic health problems can also be useful to resolve many of the questions that may arise when the person’s health deteriorates, be it acutely or over the longer term. The questions faced by the medical staff when a health event occurs concern several aspects. Firstly, anticipating a deterioration in the patient’s condition, and secondly, respecting the patient’s wishes and values in those circumstances. In the literature, several authors have reported the difficulties that these issues create, at several levels. Indeed, it is often difficult for physicians to evaluate prognosis accurately and with certainty, and this difficulty is compounded by their well-meaning optimism (24). Furthermore, physicians often lack detailed information about the patient’s clinical condition, previous history, previous quality of life, and healthcare pathway. Moreover, it can be challenging to inform patients and their immediate family about serious illness in an emergency situation, which is by its very nature, rare and unexpected. Lastly, many patients are unaware of the intensive therapies that can be implemented in emergency situations, particularly in critical care (25).
To answer these questions, for some years now, a number of Anglo-Saxon countries (e.g., United Kingdom, USA, Australia…) have initiated ACP, in addition to the previously existing advance directives (AD). ACP is an opportunity for people to reflect on their wishes, values and beliefs, and make them known to their family or close entourage as well as their usual physician, in order to make clear the treatment they would like to have, either at present or in the future, if their clinical situation deteriorated such that they were no longer able to make their own decisions. The patient can choose what types of treatment they would, or would not like to have for their disease, be it medical therapy (such as chemotherapy), surgical interventions (amputation) or initiation of life-saving therapies (mechanical ventilation, renal dialysis…). The appropriate time at which to consider ACP varies widely according to the patient’s state of health, and depends particularly on whether or not the patient has a chronic disease. The patient may change the wishes outlined in the ACP at any time according to the progression of the disease. However, ACP does require excellent communication between the patient and his/her entourage, and the treating physician(s).
In addition to usual care, another interesting option is to propose that during a pluridisciplinary meeting to discuss patient care, part of the discussion time could be dedicated to envisaging what should happen in case of “acute decompensation” (Figure 1). During this meeting, which the critical care physicians should be invited to attend, all the possible aspects (both advantages and disadvantages) of initiating (or not) one or several life-support therapies could be considered. The level of therapeutic intensity, the relevance of life-support therapies at specific points along the pathway of care, the legitimacy of repeating such therapies, etc, could all be defined. Along the patient’s healthcare pathway, these reflections could be enhanced by the patient’s own perceptions, experiences, feelings and desires. The patient would thus be in a position to prepare AD that would be of greater value than those prepared without the specific knowledge that the critical care physician can bring to the table. In this framework, the overall therapeutic project should integrate the question of admission to intensive care, allowing the patient, and/or their family, to participate in the choices that could be proposed in that scenario.
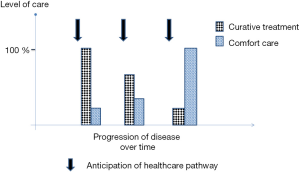
These considerations, as with ACP, could help critical care physicians in their decision-making processes, and thereby contribute to avoiding non-beneficent decisions regarding one patient (such as early discharge, withholding or withdrawal of therapy), on the—albeit laudable—basis of beneficence towards others (i.e., future admissions to ICU). When the patient’s wishes, and those of their entourage, are known in advance, end-of-life decisions can be made in the best possible circumstances, and probably more quickly in a substantial proportion of cases.
So let’s anticipate and be prepared, so that the healthcare project of one patient, especially if it concerns end-of-life decisions, is not influenced by the equally respectable healthcare project of another patient. ICU capacity strain can be anticipated, as can the other factors that play a role in end-of-life decision making, while still maintaining the ultimate respect for the patient’s wishes and values. There is likely an important role for the physician both in the ICU, and outside the ICU as a consultant, especially to inform patient choices when preparing or formalising advance directives. Adequate preparation and anticipation could help to ensure that end-of-life decisions are made with the appropriate reflection, and respecting the patient’s wishes. In this way, we can ensure that organisational constraints such as ICU strain do not rush physicians into making inappropriate decisions, but merely reduce the time to the right decisions being made.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by Section Editor Zhi Mao, MD (Department of Critical Care Medicine, Chinese People’s Liberation Army General Hospital, Beijing, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferrand E, Robert R, Ingrand P, et al. Withholding and withdrawal of life support in intensive-care units in France: a prospective survey. French LATAREA Group. Lancet 2001;357:9-14. [Crossref] [PubMed]
- Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469-78. [Crossref] [PubMed]
- Quenot JP, Rigaud JP, Prin S, et al. Impact of an intensive communication strategy on end-of-life practices in the intensive care unit. Intensive Care Med 2012;38:145-52. [Crossref] [PubMed]
- Sprung CL, Maia P, Bulow HH, et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med 2007;33:1732-9. [Crossref] [PubMed]
- Stelfox HT, Hemmelgarn BR, Bagshaw SM, et al. Intensive care unit bed availability and outcomes for hospitalized patients with sudden clinical deterioration. Arch Intern Med 2012;172:467-74. [Crossref] [PubMed]
- Curtis JR, Treece PD, Nielsen EL, et al. Randomized Trial of Communication Facilitators to Reduce Family Distress and Intensity of End-of-Life Care. Am J Respir Crit Care Med 2016;193:154-62. [Crossref] [PubMed]
- Kim MM, Barnato AE, Angus DC, et al. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med 2010;170:369-76. [Crossref] [PubMed]
- Dzeng E, Colaianni A, Roland M, et al. Influence of institutional culture and policies on do-not-resuscitate decision making at the end of life. JAMA Intern Med 2015;175:812-9. [Crossref] [PubMed]
- Sprung CL, Cohen SL, Sjokvist P, et al. End-of-life practices in European intensive care units: the Ethicus Study. JAMA 2003;290:790-7. [Crossref] [PubMed]
- Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med 2006;166:493-7. [Crossref] [PubMed]
- Schneiderman LJ, Gilmer T, Teetzel HD. Impact of ethics consultations in the intensive care setting: a randomized, controlled trial. Crit Care Med 2000;28:3920-4. [Crossref] [PubMed]
- Kerlin MP, Harhay MO, Vranas KC, et al. Objective factors associated with physicians' and nurses' perceptions of intensive care unit capacity strain. Ann Am Thorac Soc 2014;11:167-72. [Crossref] [PubMed]
- Halpern SD. ICU capacity strain and the quality and allocation of critical care. Curr Opin Crit Care 2011;17:648-57. [Crossref] [PubMed]
- Vranas K, Ratcliffe SJ, Harhay MO, et al. A Prospective Study Of The Determinants Of Intensive Care Unit (ICU) Capacity Strain. Am J Respir Crit Care Med 2012;185:A1608.
- Hua M, Halpern SD, Gabler NB, et al. Effect of ICU strain on timing of limitations in life-sustaining therapy and on death. Intensive Care Med 2016;42:987-94. [Crossref] [PubMed]
- Curtis JR, Patrick DL, Engelberg RA, et al. A measure of the quality of dying and death. Initial validation using after-death interviews with family members. J Pain Symptom Manage 2002;24:17-31. [Crossref] [PubMed]
- White DB, Curtis JR, Wolf LE, et al. Life support for patients without a surrogate decision maker: who decides? Ann Intern Med 2007;147:34-40. [Crossref] [PubMed]
- Rigaud JP, Hardy JB, Meunier-Beillard N, et al. The concept of a surrogate is ill adapted to intensive care: Criteria for recognizing a reference person. J Crit Care 2016;32:89-92. [Crossref] [PubMed]
- Pochard F, Azoulay E, Chevret S, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 2001;29:1893-7. [Crossref] [PubMed]
- Embriaco N, Azoulay E, Barrau K, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med 2007;175:686-92. [Crossref] [PubMed]
- Poncet MC, Toullic P, Papazian L, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med 2007;175:698-704. [Crossref] [PubMed]
- Quenot JP, Rigaud JP, Prin S, et al. Suffering among carers working in critical care can be reduced by an intensive communication strategy on end-of-life practices. Intensive Care Med 2012;38:55-61. [Crossref] [PubMed]
- Law 2005-370 dated 22 April 2005 regarding patients’ rights and end-of-life. Journal Officiel de la Republique Francaise; 23 April 2005. Available online: (access date: 14 June 2016).http://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000000446240&categorieLien=id
- Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ 2003;327:195-8. [Crossref] [PubMed]
- Puchalski CM, Zhong Z, Jacobs MM, et al. Patients who want their family and physician to make resuscitation decisions for them: observations from SUPPORT and HELP. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc 2000;48:S84-90. [Crossref] [PubMed]


