Single-incision video-assisted anatomical segmentectomy with handsewn bronchial closure for endobronchial lipoma
Introduction
Endobronchial lipoma is a rare benign tumor which represents less than 0.5% of all lung neoplasms (1). Typically affects the first divisions of tracheobronquial tree (2). Symptoms are nonspecific arising from cough to recurrent pneumonia (2,3), due to endobronchial obstruction. Macroscopic appearance and pathological findings can mimic other low-grade malignances such as carcinoid tumors (4), thus difficult the identification. When the diagnosis is well set, first line treatment is endobronchial resection. However complications in bronchoscopic treatment and unclear definitive diagnosis may lead to surgical treatment. We present a Single-incision video-assisted thoracoscopic surgery (SI-VATS) anatomical segmentectomy with handsewn bronchial closure for an unsuspected endobronchial lipoma.
Case presentation
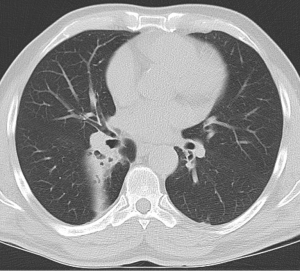
A 60-year-old man presented with right lower lobe (RLL) recurrent infections, limited to upper segment of RLL. Chest scan showed complete atelectasis and endobronchial obstruction of that segment (Figure 1). Bronchoscopic examination evidenced an endobronchial tumor with macroscopic features that strongly suggest carcinoid tumor (smooth, pearly appearance). Bronchial biopsy reported submucosal myxoid changes. With the high suspicion of carcinoid tumor without clinical nodal involvement, we decided to perform an anatomical segmentectomy with diagnostic and therapeutic aim.
Through a 4-cm SI-VATS approach, an anatomical RLL upper-segmentectomy with hilar and mediastinal lymphadenectomy were performed (Figure 2). Upper-segment parenchyma seemed congestive due to recurrent previous infections. Intraoperative frozen section showed myxoid tumor with bronchial margin contact. With the suspicion of carcinoid tumor, and in order to achieve microscopic complete resection (R0), wedge bronchoplasty with handsewn closure was carried out achieving free margins, assisted by intraoperative bronchoscopy (Figure 3). A new frozen section of the extension of the resection was informed as free of tumor. Total surgical time was 190 minutes including intraoperative frozen section.


During postoperative period there was no air leak, but due to handsewn bronchial suture chest tube was kept until 5th postoperative day. Pain control was adequate with maximum postoperative pain score in the visual analogue scale (VAS) of 2. No complications were observed during follow-up. Final pathological examination was concordant with unexpected myxoid endobronchial lipoma of 12 mm and all lymph nodes negative. Patient is free of recurrence within 12 months follow-up, doing his normal active life without symptoms.
Discussion
Endobronchial lipoma represents an uncommon lung tumor (less than 0.5%), although its real prevalence remains unknown due to the low rate of reported cases. It usually presents with endobronchial symptoms such as cough, progressive dyspnea and recurrent infections. Difficulty in diagnosis lies on unspecific symptoms and appearance, so other more prevalent neoplasms are initially suspected (3,5). There are several reported cases of endobronchial lipoma mimicking other entities, such as carcinoid tumors (4). CT scan is very sensitive and specific for adipose tissue density (6). Diagnosis is usually set by bronchoscopic biopsy (7), and then first-line treatment is bronchoscopic resection due to its benign nature. Nevertheless, surgical resection can be also considered in some situations such as anatomic difficulties, endoscopic complications or unclear diagnosis being unable to run out other low-grade malignances.
SI-VATS approach theoretically decreases postoperative pain and fastens recovery (8,9), although multicenter randomized clinical trials lack when we search for evidence. With the suspicion of a low-grade malignancy (carcinoid tumor) we proposed SI-VATS anatomical segmentectomy in order to provide the least invasive approach with a lung-sparing anatomical resection. Need for handsewn bronchial suture or a bronchoplasty is not an indication for conversion to multiport VATS or thoracotomy. Absence of postoperative complications, and low pain score proves this approach is feasible and safe even for anatomical resections needing bronchial sutures or bronchoplasties.
Sublobar anatomical resections such as segmentectomies are appropriate for benign and low-grade malignant tumors if nodal involvement is excluded. Bronchial lipomas can be a diagnostic challenge, although in these cases, minimally invasive lung-sparing techniques make surgery a suitable diagnostic and therapeutic option.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Jensen MS, Petersen AH. Bronchial lipoma. Scand J Thorac Cardiovasc Surg 1970;4:131-4. [Crossref] [PubMed]
- Muraoka M, Oka T, Akamine S, et al. Endobronchial lipoma: review of 64 cases reported in Japan. Chest 2003;123:293-6. [Crossref] [PubMed]
- Sacristán Bou L, Fernández Robledo E, Peña Blas F. Endobronchial lipoma: an unusual cause of bronchial obstruction. Arch Bronconeumol 2014;50:78-9. [Crossref] [PubMed]
- Nussbaumer-Ochsner Y, Rassouli F, Uhlmann F, et al. Endobronchial lipoma mimicking bronchial carcinoid tumour. Thorax 2015;70:809. [Crossref] [PubMed]
- Wang H, Du Z, Li A, et al. Surgical treatment of an endobronchial lipoma obstructing the right upper bronchus: Imaging features with pathological correlation. Pak J Med Sci 2013;29:1447-9. [Crossref] [PubMed]
- Cao D, Sun Y, Yang S. Endobronchial lipoma: an unusual cause of bronchial obstruction. Case Rep Med 2011;2011:939808.
- Leichtle SW, McCabe V, Gupta A. Obstructing endobronchial lipoma. Ann Thorac Surg 2014;97:714. [Crossref] [PubMed]
- Li C, Ma H, He J, et al. Clinical analysis of thoracoscopic lobectomy in the treatment of peripheral lung cancer with single utility port. Zhongguo Fei Ai Za Zhi 2013;16:487-91. [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]


