Fatty acid-binding proteins as biomarkers of disease severity and outcome in community-acquired pneumonia
In Western Europe, which is experiencing progressive population ageing, community-acquired pneumonia (CAP) is the leading cause of death due to infection, with approximately 90% of the mortality in adults occurring in those aged >65 years (1). A similar situation exists in the United States of America (2). The increasing frequency of CAP in developed countries, predominantly among the aged, has been paralleled by a growing rate of admissions to intensive care units (ICUs), which has increased significantly over the past 2–3 decades (3). Indeed CAP represents one of the leading causes of admission to ICU, with between 13% and 22% of patients hospitalised with CAP having been reported to require ICU admission (4). Notwithstanding the increasing burden of CAP associated with high-risk, ageing populations, other factors which contribute to this increase in the rate of ICU admissions include improved access to modern health care facilities equipped with sophisticated diagnostic and life-support technologies and staffed by highly-trained critical care physicians and nursing personnel. Another possible contributory factor is the uptake of reliable, predictive clinical scoring systems, specifically the pneumonia severity index (PSI) and the CURB-65 (3-5). Disappointingly, however, overall CAP-related mortality rates remain high, ranging from 5–50% according to geographic region (6,7), with the elderly, not surprisingly, at particularly high risk (8-11).
Several studies, two recent, are particularly noteworthy in respect of the outcome of patients hospitalised with severe CAP. Mongardon and colleagues analysed two prospectively-acquired French multicentre ICU databases covering the period 2001–2008 in relation to the mortality rate of patients with microbiologically-proven pneumococcal CAP (9). The authors reported an in-hospital mortality rate of 28.8% (9). More recently, Walden et al. in a larger study undertaken during the period September 2005 to October 2009, covering 102 centres across 17 countries, encompassing 1,166 CAP patients admitted to ICU, documented 28-day and 6-month mortality rates of 17% and 27%, respectively (10). Of even greater concern is the very recent study by Cavallazzi et al. who investigated the ICU mortality rates of CAP patients (n=800) from three different geographic regions (North America, Latin America, Europe) spanning the periods June 2001 to April 2004 (n=235), May 2004 to January 2008 (n=275) and February 2008 to February 2013 (n=290) (11). The respective overall in-hospital mortality rates increased during these three periods being 15.7%, 22.1% and 24.3%, respectively (11).
Given the ominous nature of the ongoing and seemingly increasing threat posed by CAP worldwide, particularly in the elderly, the identification of reliable host-derived biomarkers of infection-associated inflammatory stress and organ dysfunction remains a priority. Detection of these biomarkers in body fluids, usually serum or plasma, especially when used in combination with the aforementioned clinical scoring systems, should contribute significantly to distinguishing those patients at highest risk for a poor outcome who would benefit most from early ICU admission, as well as implementation of aggressive antimicrobial and possibly adjunctive therapies, such as corticosteroids.
Prominent host-derived biomarkers which have, and continue to attract significant interest are shown in Table 1. Some, such as procalcitonin (PCT) in particular, as well as C-reactive protein (CRP), are commonly used to monitor the need for, and responses to, antimicrobial therapy, and also to distinguish between viral and bacterial infection, while others, such as biomarkers of myocardial injury and platelet activation, appear to be predictive of both the short- and long-term cardiac events which are associated with severe CAP (12-16).
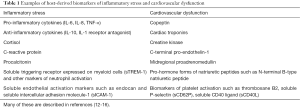
Full table
Although less well characterised in this context, fatty acid-binding proteins (FABPs) have also attracted interest as potential biomarkers of tissue injury in both acute and chronic inflammatory conditions of infective and non-infective origin. FABPs belong to a family of at least nine distinct, intracellular, low molecular weight (about 15 kDa) proteins which promote the trafficking of fatty acids across cell membranes, explaining their relative abundance in cells, tissues and organs involved in lipid metabolism (17,18). Although categorised according to their predominant site of expression and action (adipocyte, brain, epidermal, heart, liver, intestinal etc.), this classification is somewhat misleading as FABP isoform location is not cell or tissue specific. For example, following differentiation of monocytes, the resultant macrophages have been reported to express adipocyte (A)-FABP, which correlates with increased inflammatory activity of these cells (17).
Due to their primary intracellular location, the extracellular release and subsequent detection of FABPs in body fluids represents a potentially useful indicator of tissue and organ damage. Although data are somewhat limited, it is noteworthy in this context that urinary, but not serum, liver (L)-type FABP, has been reported to distinguish patients with septic shock from those with sepsis without shock, as well as from those with acute renal failure and healthy subjects (19). In a separate study, urinary L-type FABP was described as being a novel biomarker of sepsis complicated with acute kidney injury (20). In addition, elevated levels of circulating A-FABP have been reported to be predictive of coronary atherosclerotic burden (21). However, the findings of a systematic review and meta-analysis concluded that heart (H)-FABP was unsuitable as a “stand-alone” biomarker in the early diagnosis of acute myocardial infarction (22).
In the case of CAP, Chen et al. in a prospective, single centre study, investigated the potential of H-FABP, measured in whole blood on arrival of patients with CAP (n=229) at a hospital emergency department, to serve as a predictor of outcome (23). H-FABP was found to be an independent predictor of 28-day mortality the predictive accuracy of which was improved when used in combination with either CURB-65 or PSI (23). Elevated levels of H-FABP were also associated with increased requirement for mechanical ventilation and use of vasopressors within 6 hours of hospital admission (23).
More recently, Tsao et al. investigated the clinical utility of measurement of the concentrations of four different FABPs (adipocyte, heart, liver and intestinal) in urine specimens taken on days 1 and 7 after admission of elderly, critically ill pneumonia patients [n=50, median age with IQR =83.0 (72.8–88.0) years] to a respiratory ICU in assessment of disease severity and prediction of outcome (24). Patients were also categorised into two subgroups (n=25 in each) according to the absence or presence of septic shock. A small control group [n=12, median age 88.0 (78.5–88.0) years] consisted of patients admitted to the ICU with various conditions of non-infective origin, most commonly heart failure. Additional urinary biomarkers measured in the study included interleukins (ILs)-1β, -6, -8 and -10, as well as circulating PCT and CRP.
With respect to comparison between the entire pneumonia and control groups, no statistically significant differences were observed with respect to any of the test biomarkers measured in urine/blood specimens taken on day 1 (no data shown for day 7). However, comparison between the subgroups of pneumonia patients revealed significantly higher concentrations of urinary A-FABP, H-FABP, I-FABP and IL-6, (P values of <0.005, <0.025, <0.020 and <0.019 respectively according to univariate analysis) in the setting of a significantly lower PaO2/FiO2 ratio in the septic shock subgroup (24). According to stepwise regression analysis, only A-FABP was an independent predictor of disease severity (P<0.026). Further categorisation of the pneumonia patients into subgroups demonstrating clinical improvement (n=32) or no improvement (n=18), revealed significantly higher levels of all four urinary FABPs, but not of any of the other biomarkers, in the latter group, measured at day 7, but not day 1, with only A-FADP being an independent predictor of outcome (24).
The authors’ conclusion that “urinary levels of adipocyte-FABP might serve as a new biomarker in assessing the severity of pneumonia and in predicting the outcome of pneumonia in critically ill patients who required admission to ICU” must, however, be viewed in the context of the limitations of their study identified by the authors, specifically: (I) urine as opposed to serum/plasma as the matrix of choice for measurement of FABPs/cytokines; (II) the relatively small number of patients in the pneumonia group; and (III) the small number of patients in the control group, mostly with heart failure, which, as alluded to earlier, may also result in elevated levels of FABPs in body fluids (21,22).
Other aspects of the study which merit consideration include the failure of the test biomarkers measured on day one of ICU admission to distinguish between the pneumonia and control groups, possibly reflecting the very advanced ages and frequencies of comorbidities of both groups. Additional concerns include the absence of data in relation to the causative pathogens, the type of antimicrobial therapy, the use of adjunctive therapies, especially corticosteroids, and the use of other medications administered prior to and at the time of ICU admission, specifically statins, aspirin and other anti-platelet agents, all of which may have impacted on outcome. Inclusion of data derived from clinical scoring systems such as CURB-65 and PSI as comparators may have also been revealing. Finally, the inclusion of a group of healthy control subjects to provide definite basal values for cytokines and FABPs would have been useful. In fairness, however, this may have been difficult given the very advanced ages of both the pneumonia and control groups.
Given these limitations, the findings of the study reported by Tsao and colleagues, although interesting, must be considered preliminary at present, requiring confirmation in larger, stringently controlled clinical trials, incorporating other prognostic biomarkers which have attracted significant interest in CAP, such as midregional proadrenomedullin. Nonetheless, the pro-inflammatory and metabolic regulatory activities of A-FABP (17,18,25) are certainly consistent with its potential to serve as a prognostic biomarker in CAP. On a cautionary note, however, Viasus et al. in a very recent comprehensive systematic review and meta-analysis reported that the clinical utilities of several biomarkers which have attracted considerable interest (CRP, copeptin, PCT, cortisol, prohormone forms of natriuretic peptides, midregional proadrenomedullin), although demonstrating moderate-to-good predictive potential in that order, were not superior to CURB-65 or PSI in predicting short-term mortality in CAP (16). Clearly, a coordinated effort is required to prioritise the most promising biomarkers in CAP and to devise strategies to optimise their predictive potential.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by Section Editor Zhi Mao, MD (Department of Critical Care Medicine, Chinese People’s Liberation Army General Hospital, Beijing, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Torres A, Peetermans WE, Viegi G, et al. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax 2013;68:1057-65. [Crossref] [PubMed]
- Jain S, Self WH, Wunderink RG, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med 2015;373:415-27. [Crossref] [PubMed]
- Vohra AS, Tak HJ, Shah MB, et al. Intensive Care Unit Admission With Community-Acquired Pneumonia. Am J Med Sci 2015;350:380-6. [Crossref] [PubMed]
- Marrie TJ, Shariatzadeh MR. Community-acquired pneumonia requiring admission to an intensive care unit: a descriptive study. Medicine (Baltimore) 2007;86:103-11. [Crossref] [PubMed]
- Welte T. Risk factors and severity scores in hospitalized patients with community-acquired pneumonia: prediction of severity and mortality. Eur J Clin Microbiol Infect Dis 2012;31:33-47. [Crossref] [PubMed]
- Arnold FW, Wiemken TL, Peyrani P, et al. Mortality differences among hospitalized patients with community-acquired pneumonia in three world regions: results from the Community-Acquired Pneumonia Organization (CAPO) International Cohort Study. Respir Med 2013;107:1101-11. [Crossref] [PubMed]
- Welte T, Torres A, Nathwani D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax 2012;67:71-9. [Crossref] [PubMed]
- Naucler P, Darenberg J, Morfeldt E, et al. Contribution of host, bacterial factors and antibiotic treatment to mortality in adult patients with bacteraemic pneumococcal pneumonia. Thorax 2013;68:571-9. [Crossref] [PubMed]
- Mongardon N, Max A, Bouglé A, et al. Epidemiology and outcome of severe pneumococcal pneumonia admitted to intensive care unit: a multicenter study. Crit Care 2012;16:R155. [Crossref] [PubMed]
- Walden AP, Clarke GM, McKechnie S, et al. Patients with community acquired pneumonia admitted to European intensive care units: an epidemiological survey of the GenOSept cohort. Crit Care 2014;18:R58. [Crossref] [PubMed]
- Cavallazzi R, Wiemken T, Arnold FW, et al. Outcomes in patients with community-acquired pneumonia admitted to the intensive care unit. Respir Med 2015;109:743-50. [Crossref] [PubMed]
- Chang CL, Mills GD, Karalus NC, et al. Biomarkers of cardiac dysfunction and mortality from community-acquired pneumonia in adults. PLoS One 2013;8:e62612. [Crossref] [PubMed]
- Kolditz M, Ewig S, Höffken G. Management-based risk prediction in community-acquired pneumonia by scores and biomarkers. Eur Respir J 2013;41:974-84. [Crossref] [PubMed]
- Florin TA, Ambroggio L. Biomarkers for community-acquired pneumonia in the emergency department. Curr Infect Dis Rep 2014;16:451. [Crossref] [PubMed]
- Lee YJ, Lee H, Park JS, et al. Cardiac troponin I as a prognostic factor in critically ill pneumonia patients in the absence of acute coronary syndrome. J Crit Care 2015;30:390-4. [Crossref] [PubMed]
- Viasus D, Del Rio-Pertuz G, Simonetti AF, et al. Biomarkers for predicting short-term mortality in community-acquired pneumonia: A systematic review and meta-analysis. J Infect 2016;72:273-82. [Crossref] [PubMed]
- Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov 2008;7:489-503. [Crossref] [PubMed]
- Thumser AE, Moore JB, Plant NJ. Fatty acid binding proteins: tissue-specific functions in health and disease. Curr Opin Clin Nutr Metab Care 2014;17:124-9. [Crossref] [PubMed]
- Nakamura T, Sugaya T, Koide H. Urinary liver-type fatty acid-binding protein in septic shock: effect of polymyxin B-immobilized fiber hemoperfusion. Shock 2009;31:454-9. [Crossref] [PubMed]
- Doi K, Noiri E, Maeda-Mamiya R, et al. Urinary L-type fatty acid-binding protein as a new biomarker of sepsis complicated with acute kidney injury. Crit Care Med 2010;38:2037-42. [Crossref] [PubMed]
- Miyoshi T, Onoue G, Hirohata A, et al. Serum adipocyte fatty acid-binding protein is independently associated with coronary atherosclerotic burden measured by intravascular ultrasound. Atherosclerosis 2010;211:164-9. [Crossref] [PubMed]
- Bruins Slot MH, Reitsma JB, Rutten FH, et al. Heart-type fatty acid-binding protein in the early diagnosis of acute myocardial infarction: a systematic review and meta-analysis. Heart 2010;96:1957-63. [Crossref] [PubMed]
- Chen YX, Li CS. The prognostic and risk-stratified value of heart-type fatty-acid-binding protein in community acquired pneumonia in emergency department. Biomed Res Int 2014;2014:753070.
- Tsao TC, Tsai HC, Chang SC. Clinical Usefulness of Urinary Fatty Acid Binding Proteins in Assessing the Severity and Predicting Treatment Response of Pneumonia in Critically Ill Patients: A Cross-Sectional Study. Medicine (Baltimore) 2016;95:e3682. [Crossref] [PubMed]
- Hui X, Li H, Zhou Z, et al. Adipocyte fatty acid-binding protein modulates inflammatory responses in macrophages through a positive feedback loop involving c-Jun NH2-terminal kinases and activator protein-1. J Biol Chem 2010;285:10273-80. [Crossref] [PubMed]


