Epidemiology and outcomes of acute abdominal pain in a large urban Emergency Department: retrospective analysis of 5,340 cases
Introduction
Acute abdominal pain (AAP), conventionally defined as pain of nontraumatic origin with a maximum duration of 5 days (1), is one of the most common complaints leading people to the Emergency Department (ED), accounting for up to 7–10% of all ED visits (2,3). Despite the relatively high frequency, abdominal pain may be a symptom of a serious underlying disease, and the challenging differential diagnosis may generate both medicolegal litigation and unfavorable outcomes (4,5).
Despite substantial improvement in the diagnostic approach to AAP, mainly attributable to the extensive use of imaging techniques [especially computed tomography (CT)], many diagnostic pitfalls remain, which can be associated with a substantial number of misdiagnoses and/or avoidable surgery (6-8). The differential diagnosis of AAP in the adult population is rather broad, including appendicitis, peptic ulcer, urinary stones, inflammatory bowel disease, hepatobiliary diseases (e.g., biliary colic, cholecystitis, and pancreatitis), referred pain due to pneumonia as well as several other “mimics” of extra-abdominal origin (9-11). In young women, gynecologic disorders (e.g., ectopic pregnancy, endometriosis, and pelvic inflammatory disease) are additional conditions which should be considered in the differential diagnosis (12-14). Since the underlying cause for AAP can entails many different medical specialties such as gynecology, surgery, internal medicine, and urology, expert assessment is an essential requisite that emergency physicians (EPs) should have for the managed care of these patients. Notably, a large heterogeneity exists in the choice of the most appropriate diagnostic approach and treatments, mostly due to personal inclination and expertise instead of applying the available guidelines.
An accurate knowledge of all the different causes of AAP is of paramount importance, and the patients can hence be simply classified as needing urgent management (i.e., requiring treatment within 24 h in order to prevent the onset of severe complications) or not needing urgent management (1). It has been previously reported that the urgent causes most frequently encountered include appendicitis, diverticulitis, cholecystitis, and bowel obstruction, whereas the most common non-urgent cause are nonspecific abdominal pain (NSAP), also known as undifferentiated abdominal pain (UDAP), which is mostly considered as a diagnosis of exclusion (i.e., “per exclusionem”) (2,3). Nevertheless, a relatively low number of studies has been published about the epidemiology of AAP in the ED. Almost all these were based in the USA, and the majority were published between the 1980s and 1990s (15-18). Only one study has been performed in Italy to the best of our knowledge, and was mainly focused on evaluating resource utilization in management of AAP (19). The scarce information available so far is particularly concerning if one considers that abdominal pain represents one of the leading causes of repeated ED visits, often necessitating additional and expensive testing, and sometimes plagued by unfavorable outcomes (20-23). Therefore, the aim of this study was to investigate the epidemiology of AAP in an adult patient population admitted to a large urban ED and, even more importantly, to analyze the clinical outcomes based on patients returning to the ED within 5 and 30 days after first admission and needing surgery.
Methods
The epidemiology and the clinical outcome of AAP was investigated by retrospective analysis of all records of visits for abdominal pain in adult patients (i.e., older than 16 years) during the entire year 2014 at the ED of the Academic Hospital of Parma (Parma, Italy). The Academic Hospital of Parma is a 1,100-bed teaching general hospital, serving a population of about 345,000 inhabitants. The facility is also a level-2 Trauma Center, and is the only hospital in the area. The cases of AAP were extracted from the hospital database using both verbal strings (i.e., “abdominal pain”, “appendicitis”, “cholecystitis”, etc.), and pertinent ICD-IX codes (i.e., 540, 541, 542, 562, 567, 574, 575, 577, 7880, 789). All the cases that could be retrieved were then analyzed by two authors (R Mora and F Catena) to avoid selection errors and exclude erroneous codifications. All selected cases were then classified according to age, gender and final ED diagnosis. All the patients with repeated ED admissions for the same complaint within 5 and 30 days after first ED visit were thoughtfully scrutinized.
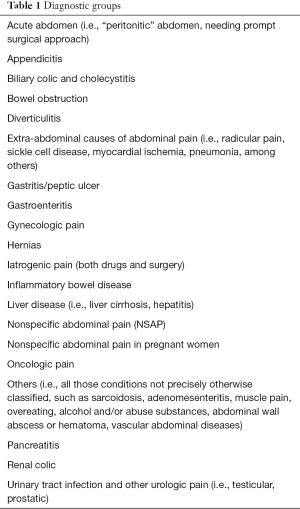
Due to practical purposes, the whole patient sample was classified in 20 different diagnostic groups, as reported in alphabetical order in Table 1. This classification was then applied to both the entire patient population and to selected groups (i.e., males and females, younger than 65 years and older than 65 years, admitted to the hospital or discharged from the ED). The study was performed in accordance with the Declaration of Helsinki, under the terms of relevant local legislation.
Full table
Results
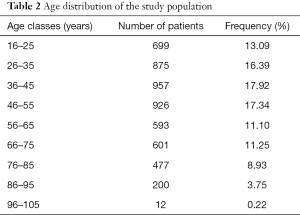
A total number of 93,367 visits have been recorded in the local ED during the year 2014, in 5,340 of which AAP was identified as the leading symptom, thus accounting for 5.76% of the total adult ED visits. The mean age of the patients was 49 years for both genders, and the age distribution of entire patient cohort is summarized in Table 2. Overall, 2,487 patients were men and 2,853 were women, respectively. The length of stay (LOS) in the ED was as follows: 6 hours and 15 min (mean value); 4 hours and 5 min (median value). The retrospective analysis of data showed that 2,561 (47.9%) patients left the ED in <4 hours, 2,016 (37.7%) between 4–8 hours and 763 (14.3%) after >8 hours.
Full table
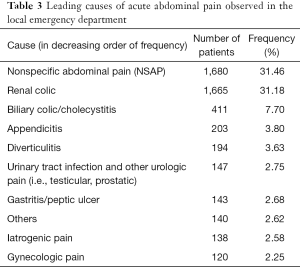
The first ten diagnoses in patients admitted to the ED with AAP are summarized in Table 3. The most frequent cause was NSAP (1,680 visits, 31.46%), followed by renal colic (1,665 visits, 31.18%). These two diagnoses thus represented >60% of all causes. Other less frequent causes included gastroenteritis (1.93%) pancreatitis (1.89%), oncologic pain (1.16%), extra-abdominal causes of abdominal pain (0.86%), hernias (0.82%), bowel obstruction (0.77%), acute abdomen (0.60%), liver disease (0.52%), inflammatory bowel disease (0.52%), and NSAP in pregnant woman (0.43%).
Full table
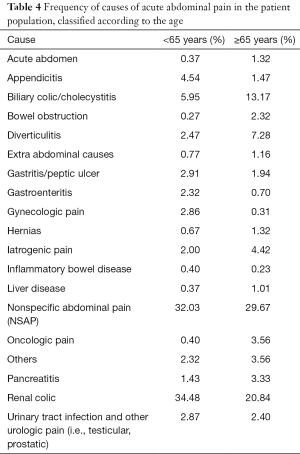
The distribution of the different diagnoses according to the age of the patients (i.e., younger or older than 65) is shown in Table 4. Biliary colic and cholecystitis exhibited a twice higher frequency in patients aged over 65 years (i.e., 13.17% vs. 5.95%), whereas diverticulitis was also found to be 3-time more frequent in this class of elderly patients (i.e., 7.28% vs. 2.47%). At variance with this data, appendicitis (i.e., 4.54% vs. 1.47%) and renal colic (34.48% vs. 20.84%) were found to be more frequent in patients aged <65 years. Notably, the NSAP was the most common cause in both age classes, despite being slightly more frequent in younger patients (32.03% compared to 29.67% in patients aged >65 years).
Full table
Except for gynecologic pain, some minor differences were observed between genders. Renal colic was found to be the most frequent cause of ED admission for AAP in men, whereas NSAP was found to be more prevalent in women. Urinary tract infection was significantly higher in women than in men (see Table 5).
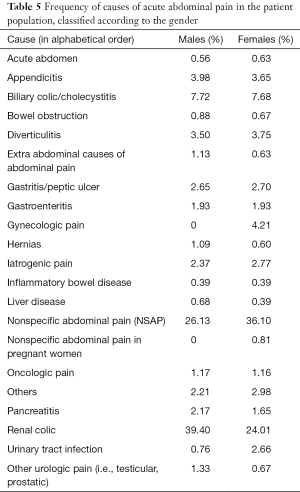
Full table
Overall, 885 patients (16.57%) were hospitalized after the ED visit, 435 of whom were men (17.49%) and 450 were women (15.77%), respectively. The admission rate for each diagnosis group is shown in Table 6. Ninety one patients (5.41%) with a diagnosis of NSAP and 90 patients (5.40%) with renal colic needed hospital admission, mainly for the presence of comorbidities in NSAP patients and for recidivism or complications (e.g., pyelonephritis) in renal colic patients. Biliary colic and cholecystitis accounted for as many as 18% of the total hospital admissions, followed by appendicitis (15%) and diverticulitis (11%). Overall, these three diagnoses represented nearly half of all hospital admissions for AAP.
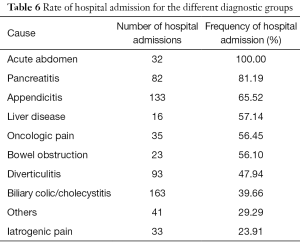
Full table
A total number of 489 patients had repeated ED visits throughout the study period. Among these, 302 patients (6.46%) were readmitted to the ED within 30 days after the first visit (for an overall number of 345 visits), whereas 187 patients (3.82%) were readmitted to the ED within 5 days after the first ED visit (for an overall number of 204 visits). Renal colic was the first cause for ED readmission, followed by NSAP. In particular, 122 patients with renal colic (59.8% of those readmitted to the ED), and 33 patients with NSAP (16.2% of those readmitted to the ED) presented to the ED within 5 days, whereas 179 patients with renal colic (51.9%) and 67 with NSAP (19.4%) presented to the ED within 30 days. Biliary colic/cholecystitis was the third cause leading to ED readmission, both within 5 and 30 days.
Fifty-four out of the 187 patients (28.9%) visiting the ED within 5 days after the first visit needed hospital admission. Among these, 27 had recurrence of renal colic, and 13 were diagnosed with biliary colic/cholecystitis (9 of whom needing surgery). In 13 cases readmitted to the ED within 5 days a different diagnosis was made during the second visit. Interestingly, 8 original diagnoses of NSAP were then readmitted with a new diagnosis of: appendicitis (n=2), diverticulitis (n=3), bowel obstruction (n=1), gynecologic pain (n=1), and other diagnosis (n=1). Thirty one out of the 302 patients (10.2%) visiting the ED between 5–30 days after the first visit needed hospital admission. Among these, 6 had recurrence of renal colic, and 6 were diagnosed with biliary colic/cholecystitis (5 of whom needing surgery). In 16 cases readmitted to the ED between 5–30 days a different diagnosis was made during the second visit. In particular, 13 original diagnoses of NSAP were changed in appendicitis (n=3), diverticulitis (n=4), bowel obstruction (n=1), gynecologic pain (n=1), liver disease (n=1), biliary colic/cholecystitis (n=1), extra-abdominal cause (n=1) and other diagnosis (n=1).
Discussion
Undeniable evidence was brought that AAP of non-traumatic origin is one of the more frequent complaints leading people to EDs. The results of our study show that this condition represented 5.76% of total ED visits during a 1-year period, thus substantially confirming the data earlier published (3,19).
Despite remarkable improvements in the diagnostics approach, entailing the use of useful techniques such as echography and CT, the leading diagnosis remains NSAP, which represented approximately one third of all causes of AAP in our patient population. Notably, the frequency of NSAP diagnoses ranges widely in the published literature (i.e., between 15.5% and 39.9%) (2,15,19,24,25), a heterogeneity mostly depending on the selection criteria used in the individual studies and on the local organization.
The widespread use of sophisticated imaging techniques was found to bring marginal improvements of diagnostic specificity in the last decades, especially for surgical illness (7,8), but has not generated a substantial reduction of the admission rate (3). Despite reliable evidence of scarce diagnostic performance (26-28), plain abdomen X-ray is still widely prescribed in as many as 35–45% of all cases of AAP in different facilities (19,28).
In some previous studies the diagnoses of renal colic were excluded from the final study cohort of patients needed ED visit for AAP (29). Unlike this scenario, patients with renal colic were included in our retrospective investigation, since the clinical presentation is often atypical (i.e., absence of flank pain) and sometimes the pain is irradiated to abdomen thus needing to be carefully considered for the differential diagnosis (30,31). We have hence observed that renal colics accounted for as many as one third of all ED visits for AAP, a frequency that was slightly lower than that of NSAP. Interestingly, these two diagnostic groups, accounting for up to 63% of all causes, have also the highest risk of recurrence counterbalanced by the lowest rate of hospital admission.
Although the overall diagnostic accuracy of combining medical history, physical examination and laboratory testing appears to be insufficient to reach a final correct diagnosis (32-34), this strategy is seemingly useful for discriminating urgent and non-urgent causes of AAP and supports the choice of prescribing additional imaging investigations in patients with a suspect of an urgent disease (28).
Diagnostic delay, late management and the risk of clinical worsening are the leading concerns of many EPs during the evaluation of patients with AAP. A comprehensive physical examination, close observation and serial diagnostic testing were found to be effective means to lower the risk of adverse outcome (35,36). This conclusion is supported by the data of a systematic review and meta-analysis of the scientific literature, showing that the length of hospital stay and the rate of complications or readmission were not significantly different when comparing active observation with early laparoscopic intervention (37). Additional evidence was brought that an observational period of 10 hours enhanced the ability to diagnosing appendicitis in patients with an intermediate probability (38). Interestingly, one study in women with NSAP demonstrated that of the 51% of women randomized to observation, 39.2% of them underwent surgical intervention for worsened symptoms or development of peritonitis, also showing statistically significant shorter hospital stay without any difference in mortality or morbidity, and without statistical significance in the recurrence of abdominal pain within 12 months (39). In another prospective study including 220 patients of all ages admitted with AAP, a substantial decrease (i.e., from a 33% to a 5%) of negative findings on laparotomy was observed at the end of follow-up (40). Interestingly, the data of our retrospective analysis confirms a large use of active clinical observation during ED stay, since 52% of our patients were discharged after more than 4 hours of LOS in the ED.
It has been previously underlined that routinely outpatient re-evaluation of patients suspected of a nonurgent condition after clinical evaluation and ultrasound testing led to a change in diagnosis in diagnosis in a substantial 18%, change in management in 13%, and a change from conservative to surgical treatment in 3% of patients (41). Nevertheless, our data show that a very modest percentage of patients (13 patients reevaluated within 5 days, 6.9%; 16 patients reevaluated between 5–30 days, 7.6%) had the original diagnosis changed during the second visit. This was probably due to a more accurate and extensive evaluation, encompassing higher frequency of observation during ED stay combined with larger use of laboratory and imaging testing.
Despite ED discharge mainly depends on the final diagnosis, the appropriate management of patients without specific diagnoses for abdominal pain (i.e., NSAP, accounting for about one third of all causes) remains challenging, so that several options can be exercised. The patients can be delivered to surgery, admitted for medical management, kept in observation, or even discharged to home with specific precautions and follow-up evaluation. The different decision to discharge the patients or keep them in observation depends on several factors such as the possibility to undergo timely follow-up, and the ability to return to the hospital when the clinical conditions should eventually worsen.
According with the clinical policy in use in the local ED, all patients discharged from the ED with a diagnosis of NSAP receive written instructions, entailing: (I) symptoms needing urgent ED reevaluation; (II) nutritional guidance; (III) pharmacologic treatment; (IV) phone number of the ED, in case additional information may be needed. The high concordance rate between the first and second diagnoses observed in our study, along with the very low number of patients undergoing surgery upon ED readmission are seemingly in support of the safety, effectiveness and efficiency of our clinical pathway.
Acknowledgements
The authors acknowledge Drs. Marco Brambilla and Marco Mignani of the University Hospital of Parma for their kind support in extracting data from electronic databases of the institution.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional ethics approval was applied but waived due to the retrospective nature of the study and to the anonymous way in collecting data.
References
- Gans SL, Pols MA, Stoker J, et al. Guideline for the diagnostic pathway in patients with acute abdominal pain. Dig Surg 2015;32:23-31. [Crossref] [PubMed]
- Powers RD, Guertler AT. Abdominal pain in the ED: stability and change over 20 years. Am J Emerg Med 1995;13:301-3. [Crossref] [PubMed]
- Hastings RS, Powers RD. Abdominal pain in the ED: a 35 year retrospective. Am J Emerg Med 2011;29:711-6. [Crossref] [PubMed]
- Selbst SM, Friedman MJ, Singh SB. Epidemiology and etiology of malpractice lawsuits involving children in US emergency departments and urgent care centers. Pediatr Emerg Care 2005;21:165-9. [PubMed]
- Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med 2007;49:196-205. [Crossref] [PubMed]
- Patterson BW, Venkatesh AK, AlKhawam L, et al. Abdominal Computed Tomography Utilization and 30-day Revisitation in Emergency Department Patients Presenting With Abdominal Pain. Acad Emerg Med 2015;22:803-10. [Crossref] [PubMed]
- Flum DR, Morris A, Koepsell T, et al. Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA 2001;286:1748-53. [Crossref] [PubMed]
- Medford-Davis L, Park E, Shlamovitz G, et al. Diagnostic errors related to acute abdominal pain in the emergency department. Emerg Med J 2016;33:253-9. [Crossref] [PubMed]
- McNamara R, Dean AJ. Approach to acute abdominal pain. Emerg Med Clin North Am 2011;29:159-73. vii. [Crossref] [PubMed]
- Palmer J, Pontius E. Abdominal Pain Mimics. Emerg Med Clin North Am 2016;34:409-23. [Crossref] [PubMed]
- Cervellin G, Lippi G. Abdominal migraine in the differential diagnosis of acute abdominal pain. Am J Emerg Med 2015;33:864.e3-5. [Crossref] [PubMed]
- Tayal VS, Bullard M, Swanson DR, et al. ED endovaginal pelvic ultrasound in nonpregnant women with right lower quadrant pain. Am J Emerg Med 2008;26:81-5. [Crossref] [PubMed]
- Cervellin G, Comelli I, Sartori E, et al. A four-year survey on unexpected pregnancy diagnoses in a large urban emergency department in Parma, Italy. Int J Gynaecol Obstet 2014;127:51-4. [Crossref] [PubMed]
- Kaplan BC, Dart RG, Moskos M, et al. Ectopic pregnancy: prospective study with improved diagnostic accuracy. Ann Emerg Med 1996;28:10-7. [Crossref] [PubMed]
- Brewer BJ, Golden GT, Hitch DC, et al. Abdominal pain. An analysis of 1,000 consecutive cases in a University Hospital emergency room. Am J Surg 1976;131:219-23. [Crossref] [PubMed]
- Lukens TW, Emerman C, Effron D. The natural history and clinical findings in undifferentiated abdominal pain. Ann Emerg Med 1993;22:690-6. [Crossref] [PubMed]
- Graff LG 4th, Robinson D. Abdominal pain and emergency department evaluation. Emerg Med Clin North Am 2001;19:123-36. [Crossref] [PubMed]
- Silen W. Cope’s early diagnosis of the acute abdomen. 19th edition. New York: Oxford University Press, 1996.
- Caporale N, Morselli-Labate AM, Nardi E, et al. Acute abdominal pain in the emergency department of a university hospital in Italy. United European Gastroenterol J 2016;4:297-304. [Crossref] [PubMed]
- Long A, Cambridge R, Rosa M. Physician’s changes in management of return visits to the Emergency Department. Emerg Care J 2016;12:35-9.
- Sauvin G, Freund Y, Saïdi K, et al. Unscheduled return visits to the emergency department: consequences for triage. Acad Emerg Med 2013;20:33-9. [Crossref] [PubMed]
- Wu CL, Wang FT, Chiang YC, et al. Unplanned emergency department revisits within 72 hours to a secondary teaching referral hospital in Taiwan. J Emerg Med 2010;38:512-7. [Crossref] [PubMed]
- Ferlander P, Elfström C, Göransson K, et al. Nonspecific abdominal pain in the Emergency Department: malignancy incidence in a nationwide Swedish cohort study. Eur J Emerg Med 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Irvin TT. Abdominal pain: a surgical audit of 1190 emergency admissions. Br J Surg 1989;76:1121-5. [Crossref] [PubMed]
- Flasar MH, Cross R, Goldberg E. Acute abdominal pain. Prim Care 2006;33:659-84. vi. [Crossref] [PubMed]
- van Randen A, Laméris W, Luitse JS, et al. The role of plain radiographs in patients with acute abdominal pain at the ED. Am J Emerg Med 2011;29:582-589.e2. [Crossref] [PubMed]
- Paolillo C, Spallino I, Cervellin G, et al. Is There Still a Role for Abdominal Plain X-ray in Acute Abdomen? Emerg Care J 2015;11:50-1. [Crossref]
- Laméris W, van Randen A, van Es HW, et al. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ 2009;338:b2431. [Crossref] [PubMed]
- Macaluso CR, McNamara RM. Evaluation and management of acute abdominal pain in the emergency department. Int J Gen Med 2012;5:789-97. [Crossref] [PubMed]
- Shokeir AA. Renal colic: new concepts related to pathophysiology, diagnosis and treatment. Curr Opin Urol 2002;12:263-9. [Crossref] [PubMed]
- Worcester EM, Coe FL. Clinical practice. Calcium kidney stones. N Engl J Med 2010;363:954-63. [Crossref] [PubMed]
- Kraemer M, Yang Q, Ohmann C, et al. Classification of subpopulations with a minor and a major diagnostic problem in acute abdominal pain. Theor Surg 1993;8:6-14.
- Hancock DM, Heptinstall M, Old JM, et al. Computer aided diagnosis of acute abdominal pain. The practical impact of a ‘theoretical exercise’. Theor Surg 1987;2:99-105.
- Laurell H, Hansson LE, Gunnarsson U. Diagnostic pitfalls and accuracy of diagnosis in acute abdominal pain. Scand J Gastroenterol 2006;41:1126-31. [Crossref] [PubMed]
- Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg 2006;244:656-60. [Crossref] [PubMed]
- Agresta F, Ansaloni L, Catena F, et al. Acute appendicitis: position paper, WSES, 2013. World J Emerg Surg 2014;9:26. [Crossref] [PubMed]
- Maggio AQ, Reece-Smith AM, Tang TY, et al. Early laparoscopy versus active observation in acute abdominal pain: systematic review and meta-analysis. Int J Surg 2008;6:400-3. [Crossref] [PubMed]
- Graff L, Radford MJ, Werne C. Probability of appendicitis before and after observation. Ann Emerg Med 1991;20:503-7. [Crossref] [PubMed]
- Morino M, Pellegrino L, Castagna E, et al. Acute nonspecific abdominal pain: A randomized, controlled trial comparing early laparoscopy versus clinical observation. Ann Surg 2006;244:881-6; discussion 886-8. [Crossref] [PubMed]
- Thomson HJ, Jones PF. Active observation in acute abdominal pain. Am J Surg 1986;152:522-5. [Crossref] [PubMed]
- Toorenvliet BR, Bakker RF, Flu HC, et al. Standard outpatient re-evaluation for patients not admitted to the hospital after emergency department evaluation for acute abdominal pain. World J Surg 2010;34:480-6. [Crossref] [PubMed]


