
Treatment strategies for complex ankle fractures—current developments summarized in a narrative review
Introduction
Besides simple fracture entities resulting from low energy trauma, there are complex ankle fractures ranging from bi- and trimalleolarfractures (AO type 44A-C) up to tibial pilon fractures (AO type 43C), resulting from high-energy (axial) trauma (1).
While ankle fractures in general are very common and account for almost 10% of all fractures, tibial pilon fractures are rather rare, only making up 3–10% of all ankle fractures (2-4).
A bimodal distribution in the occurrence of this trauma entity can be observed. The first peak comprises younger, mostly male patients with high-energy trauma, such as falls from great heights or motor vehicle accidents, approximately 6% of patients with tibial pilon fractures are polytraumatized (5). Additionally, the rate of open fractures has been reported to be as high as 50% in high-energy tibial pilon fractures (6). Especially in these high-energy traumas the soft tissue damage can be severe and soft tissue will dictate the plan of treatment as well as the outcome in complex fracture situations (5).
The second peak includes older, predominantly female patients with often osteoporotic bone structure. Here rotational forces or minor incidents, that would not normally even classify as low-energy trauma, can lead to severe ankle and pilon fractures (1,4,7,8). Due to this high incidence of injuries in older women, some authors have suggested in the past, that ankle fractures, especially tri- and bimalleolar fractures should be regarded as fragility fractures (9,10).
Complex ankle fractures have in common the high significance of soft tissue management, deep wound infections are still reported with a rate of up to 15% in several studies (11-13). Soft tissue status is also an important factor for the exact timing of surgery. Poor quality of bone can further make surgical treatment of complex ankle fractures even more difficult especially in geriatric patients (14). The functional outcome after severe ankle fractures is still moderate to low with over one third of all patients developing osteoarthritis after injury (15). The role of the posterior malleolus in treating complex ankle fractures has been widely discussed in recent years. Outcome has been proven to be worse when posterior malleolus fractures are present and most authors agree that fixation is preferable as the posterior malleolus provides significant stability to the ankle (16,17).
As mentioned above, outcome after complex ankle fractures remain poor and complication rate is high, posing a great challenge to treating surgeons worldwide. Especially with the rising number to complex ankle fractures in the geriatric population an optimized treatment plan with new techniques might become even more important. Therefore, this review aims to summarize the current standard of treatment and to highlight current innovations and new techniques especially in the geriatric population further. We present this article in accordance with the Narrative Review reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1173/rc).
Methods
We conducted a thorough search of PubMed database in December 2022 to identify relevant articles on complex ankle and tibial pilon fractures (Table 1). Articles in English and German were included in this study.
Table 1
| Items | Specification |
|---|---|
| Date of search | 10.12.2022 |
| Database | PubMed |
| Search terms used | “Complex ankle fractures”, “tibial pilon”, “tibial plafond” |
| Timeframe | 2017–2022 |
| Exclusion criteria | Language other than English or German |
| Selection process | Authors read and selected suitable studies |
Initial treatment
Complex ankle fractures should be reduced as quickly as possible. This is the most effective way to minimize tension on neurovascular structures, decelerate swelling and to optimize pain management (see case 1). Timely reduction further decreases the risk of cartilage damage and local tissue necrosis (18). If closed reduction cannot be retained due to high comminution or entrapped soft tissue, treating surgeons should aim for open reduction in the operation room in order to minimize the risk of further complications (19). In case of open fractures, severe soft tissue injury or (impending) compartment syndrome, open reduction and ankle spanning external fixation (EF) is indicated (20,21).
It is imperative to obtain CT scans before definitive treatment as fracture patterns are incomprehensible without. Tornetta and coworkers have shown that treatment plans change in up to 64% of the times, when scans are obtained after temporary fixation (22). The principle of “span, scan and plan” has been proven useful in clinical practice, but timing of CT scan is less important than quality. Therefore, it has been suggested to span the ankle with EF prior to doing a CT scan to then have time to plan the appropriate course of treatment (12,21).
Nonoperative treatment
Overall operative treatment of complex ankle fractures is the method of choice in most industrialized countries according to current literature (1,23). As high mal- and non-union rates have been reported in unstable ankle fractures and secondary operative treatment becomes necessary in up to 19%. However, current literature strongly advocates for operative treatment of complex ankle fractures, especially when the posterior malleolus is affected (21,24-29).
In multimorbid patients nonoperative treatment might be feasible, including immobilization in a well-padded cast under close observation of soft tissue and regular radiographic control of possible secondary dislocation. Yet, minimally invasive surgical techniques, EF as definitive treatment or even tibiocalcaneal nailing are available moving non-operative treatment of tibial pilon fractures further in the background (30,31).
Timing of surgery
Spanning the ankle allows the soft tissue to heal and most importantly the swelling to recline. In less unstable or less comminuted ankle and tibial pilon fractures this period of soft tissue recuperation can also be bridged in a well-padded cast, but it can make monitoring the soft tissue more difficult.
However, the exact timing for definitive treatment for closed complex ankle and tibial pilon fractures is still controversially discussed. While most authors agree that timing of surgery is dictated by the soft tissue, the ideal time of surgery spans from a few hours to multiple days and no clear decision criteria are present (10).
Pilskog and coworkers suggested that in low-energy ankle fractures with involvement of the posterior malleolus the clinical outcome is superior in patients who had surgery within the first 24 to 48 h opposed to after 7 days (32). Multiple other authors support these findings (13,33,34). However, logistical restrictions such as limited availability of surgical capacity especially in smaller hospitals on weekends or at night and a lack of experienced foot and ankle surgeons at such times, need to be taken into consideration as well (13).
In contrast, a Norwegian study group did not find any differences in complication rates, length of hospital stay and patient satisfaction associated to the timing of surgery of unstable ankle fractures (35).
In tibial pilon fractures there was a shift from the one-staged treatment protocol to a two-staged treatment protocol in the early 2000s. Few authors were able to proof lower complication rates, especially concerning infection, revision surgery and malunion with a two-staged approach (24,36-38).
However, the ideal moment for definitive treatment of tibial pilon fractures is still unclear as well. Soft tissue dictates timing of surgery and fracture blisters or open fracture wounds might compromise approaches and timing of surgery further. In clinical practice “wrinkling of the skin” has proven to be a viable indicator for operability (5,39).
Important aspects of operative treatment
Planning
CT scans need to be studied closely prior to surgery in order to understand the fracture pattern and identify the main fragments. In tibial pilon fractures surgeons need to be paying specific attention to the three main columns: the anterolateral, posterolateral and medial column.
Additionally, soft tissue status, fracture configuration, comorbidities, such as diabetes and osteoporosis and demand of the patient prior to injury need to be taken into close consideration when planning treatment of complex ankle fractures. Primary goal should be anatomic reduction of the articular surface and restoration of rotation and length. ORIF will be the first choice of fracture fixation in most cases (27).
In the last decade intraoperative 3D-imaging has become the standard of care especially in ankle fractures where the tibiofibular syndesmosis is injured. It can be used to assess the correct reduction of the fibula in the tibial incisura and intraoperative revision rates have been reported to be as high as 36% after 3D-scanning of the ankle (40,41).
Approaches
As already stressed before approaches need to be planned carefully. The goal is to identify the main fragments and to choose approaches in order to be able to visualize these main fragments properly. Reduction of complex ankle fractures with joint involvement is usually done sequentially, going from posterior to anterior and lateral to medial fragments (42). 360° fixation of complex ankle fractures is becoming more popular in recent years. Therefore, posterior approaches, such as the posterolateral and posteromedial approach which allow for direct visualization of the posterior joint block have become increasingly important. Many surgeons choose to address the posterior malleolus fragments first, as it provides stability for the rest of the joint block and other fragments can be reduced around it (43,44).
Additionally, minimally invasive techniques and approaches are continuously coming into focus especially in distal tibial fractures. Good results with similar outcome to ORIF could be seen, but minimally invasive osteosynthesis (MIO) was mostly used on non-displaced and non-comminuted fractures (45). The incisions used for MIO usually serve different purposes, e.g., visualization, reduction, fixation, etc. Multiple incisions are typically necessary with the exact location depending on fracture pattern and the location of anatomical structures, the incisions should therefore be carefully planned preoperatively. MIO can also be used in combination with open fixation techniques or arthroscopic inspection of the talocrural joint (46). Authors agree that MIO is not to be used in Gustillo type III open fractures or when concomitant neurovascular injuries are present (47). By utilizing MIO the iatrogenic soft tissue damage is less severe and deperiostation and therefore loss of blood supply at the fracture site less extensive (5). Nevertheless, minimally invasive plate osteosynthesis (MIPO) has shown a higher rate of non-union, delayed union and soft tissue impingement than ORIF (48). Fixation techniques do not vary significantly from the well-known techniques used for intraarticular, multifragmentary fractures, with k-wires, lag screws, buttress plating and use of combinations of the above (49).
The relevance of fibula fractures in complex ankle fractures is well debated , demanding further attention when planning adequate approaches (50). When to address distal fibula fractures in complex ankle fractures has been discussed widely in recent literature, with no consensus so far (51-53). ORIF utilizing a direct lateral, posterolateral or anterolateral approach is the standard of care in distal fibula fractures. The distal fibula is highly relevant for restoration of overall length, lateral column stability, and joint congruency (54). Locking plates provide a better construct stability especially in osteoporotic bone compared to semicircular tubular plates, but can cause additional irritation to soft tissue as they are generally thicker (55-57). Alternatively distal fibula fractures can be addressed with minimally invasive techniques, such as intramedullary nailing. This can be a viable option in severely impacted soft tissue and elderly patients (58). Rouhani and coworkers found no difference in the outcome after tibial pilon fractures with compared to without fixation of the distal fibula in their retrospective study at two-year follow-up (53). These findings are further supported by multiple other authors (59,60). However, most studies are of retrospective character.
Soft tissue impairment, such as fracture blisters or wounds from open fractures might impact this decision further. Therefore, exact preoperative planning and meticulous studying of CT scans is essential prior to surgery (61). Some studies suggest that minimum distance between two incisions should be 5 to 7 cm to provide a safe distance for the skin bridge. For minimally invasive incisions the safe distance is even smaller (62). Esposito et al. were able to show that the approach chosen does not seem to influence complication rate after tibial pilon fractures (11).
Posterior malleolus
In trimalleolar fractures the configuration of the posterior malleolus fragment needs to be studied closely. There is varying evidence and ongoing discussion about the role of fixation of the posterior malleolus in current research. The mere presence of posterior malleolus fractures in complex ankle fractures contributes to a worse outcome (63). However, when and how to surgically fix the posterior malleolus remains unclear. So far, most authors agreed that fragments comprising more than one forth to one third of the articular surface, a dislocation of ≥2 mm on the lateral radiograph or small intraarticular fragments or chondral fragments are an indication for surgical fixation of the posterior malleolus (16). However, interpreting fragment size on lateral radiographs or even CT scans is extremely difficult and unreliable, challenging the theory of size further (64,65).
In the last decade, scientific focus diverted from fragment size towards functional criteria in deciding whether to fix the posterior malleolus. By reducing the posterior malleolus stability of the ankle increases posteriorly and with direct visualization anatomic reduction of the articular surface is possible. Additionally, the posterior tibiofibular ligament (PTFL) inserts on the posterolateral malleolus, so by fixing the posterior malleolus, syndesmotic stability can be restored and trans-syndesmotic fixation might prove redundant. Furthermore, reduction of the fibular notch can facilitate reduction of fibular fractures (16,66-68). Due to all these benefits of reduction and fixation of the posterior malleolus in treatment of complex ankle fractures the current trend clearly goes towards fixation (15,63,69-71).
Posterior malleolus fragments can be reduced directly using a posterolateral or posteromedial approach. Indirect reduction and screw fixation is possible via and anterior approach, but this tends to be less stable than direct fixation (16). Reduction is done via ligamentotaxis, direct visualization is impossible and intercalary fragments cannot be reduced or removed at all. Therefore, indirect reduction has been proven to be inferior in functional outcome in comparison to a posterolateral direct approach to the posterior malleolus (67,72,73).
Direct visualization aids anatomic reduction and therefore lowers the risk for secondary osteoarthritis. Additionally, distal fibula fractures can also be addressed via the posterolateral approach (10).
Nevertheless, fixation via a posterolateral approach poses surgical risks to the sural nerve and it can cause irritation to the adjacent peroneal tendons. Additionally, injuries to the flexor hallucis longus tendon are reported frequently (74,75).
Postoperative care
While for the past decades weight bearing was usually restricted for six weeks postoperatively, there is a trend towards early weight bearing starting after three postoperative weeks. Several studies were able to show no difference in rates of implant failure, hardware loosening, revision surgery rates and rates of wound complications (76,77). Therefore, especially compliant patients can be considered for an early weight bearing regimen.
Special indications
As explained above, surgical treatment of complex ankle fractures pose a great challenge to treating surgeons. Comminuted intraarticular fractures of the tibial plafond will need anatomic reduction especially of the joint surface in order to reduce the risk for posttraumatic arthrosis. Arthroscopically assisted surgery has been discussed in current literature for intraarticular ankle fractures (78). Some authors have reported favorable outcomes in terms of bone union, postoperative reduction, but no difference was found in patient reported outcome (79,80). However, evidence so far is limited and more randomized controlled trials with larger patient cohorts are necessary.
External fixation as definitive treatment
While ORIF will be the surgical approach of choice for treating tibial pilon fractures, alternative options such as EF might need consideration especially in highly comminuted, Gustillo type III-open ankle fractures with significantly impacted soft tissue envelope or in geriatric patients with a high risk for complications after ORIF (44).
The most obvious advantages of EF compared to ORIF is the minimally invasive incisions used to place k-wires and/or pins, making soft tissue impairments less problematic. Furthermore, immediate weight bearing after surgery, which is possible with Ilizarov/ring EF, can lessen complications related to prolonged immobilization immensely especially in geriatric patients (31,81,82). Ilizarov EF can further be used for distraction osteogenesis when severe bone loss is present (83).
While pin tract infections are a feared problem after prolonged EF, severe complications are rare (27).
Prolonged immobilization of the ankle in ankle spanning EF can lead to significantly reduced outcome and ankle mobility post-treatment, but the use of ankle spearing EF might be possible in some cases (82,84).
One of the major disadvantages of EF is the lack of possibility of anatomical reduction of the articular surface, which is associated with a lower overall functional outcome (51,85-88). However, in patients with extremely severe type AO C3 tibial pilon fractures with badly impacted soft tissue the functional outcome after EF and ORIF are similar (44,89-91).
Complex ankle fractures in the geriatric population
With the aging population the number of complex ankle fractures in geriatric patients is steadily increasing and is anticipated to rise even further in upcoming decades (92). Multiple authors have discussed the specific challenges accompanied in treatment of ankle fractures in the geriatric population. The reoccurring problems with treating ankle fractures in elderly patients are compromised soft tissue, osteoporotic bone and significant comorbidities (58). Due to this combination of problems the treatment of these fractures is particularly difficult. The main goal in elderly patients must be to restore mobility as quickly as possible, reducing mortality and morbidity caused by immobilization and restoring pre-accident self-sufficient living (93).
Preoperatively, patients need to be assessed thoroughly for preexisting conditions, such as diabetes, vascular disease, a history of osteoporosis and additionally, surgeons need to evaluate the patients’ level of physical fitness and demand in everyday life previous to the injury as “golden agers” might need different treatment options than frail, bed-ridden patients (93,94).
Nonoperative treatment utilizing prolonged cast immobilization can be considered in stable, non-comminuted and non-displaced fractures. Nevertheless, prolonged immobilization in casts without the possibility of weight bearing options, such as walkers/boots will lead to increased immobility and higher morbidity and mortality in these patients (94). Secondary dislocation and malunion rates have been reported to be as high as 73% posing a further risk to failure of conservative treatment (94). Additionally, partial weight bearing often cannot be accomplished by elderly patients, posing a further risk to ORIF and prolonging hospital stays significantly (95).
While ORIF is the treatment option of choice for ankle and pilon fractures in younger patients, the known complications can be multiplied in elderly patients. Fixing bulky plates underneath thin subcutaneous and already strained skin often increases swelling severely. Additionally, classical non-locking plating systems might fail in osteoporotic bone. Overall, most authors agree that ORIF in elderly patients tends to have a high complication rate. This is mostly due to the heavily compromised soft tissue envelope leading to known complications such as impaired wound healing, superficial or deep infections of the surgical site and failure of osteosynthesis. When the decision for ORIF in elderly patients is made, surgeons must plan surgical approaches extremely careful and locking-plates should be used in order to increase stability in osteoporotic bone further (14,93).
Because of the high complication rate accompanied by standard ORIF and conservative treatment in elderly patients, alternative methods are often utilized. Primary ankle arthrodesis using tibiotalocalcaneal retrograde nailing has become increasingly popular in recent years. So far ankle arthrodesis has mainly been used as a salvage technique for severe osteoarthritis or after failed ORIF. Yet recently multiple authors have presented good results, when using ankle arthrodesis as a primary treatment option (14,30,58,96). The main argument for using a minimally invasive retrograde nail primarily is the limited soft tissue mantle in elderly patients. Furthermore, it can be a viable treatment option in patients with Charcot neurogenic osteoarthropathy and patients with diabetes or chronic venous insufficiency (93). Nevertheless, ankle mobility is lost completely, which can make mobilization of already frail patients even more difficult. On the other hand, full-weight bearing is possible directly after surgery reducing the complications of prolonged immobilization (58).
Another possible salvage technique in elderly patients can be the use of external ring fixation as definitive treatment. Because k-wires and pins utilized to build ring EF are placed minimally invasive, large incisions further compromising soft tissue can be avoided completely. Also, in patients with fracture blisters, open fractures and other soft tissue injuries, using ring EF e.g., the Ilizarov EF can be helpful as well. An additional advantage is the possibility of early weight bearing, short operation time and possibility of early ambulation. Nevertheless, indirect reduction and ligamentotaxis alone cannot address small intraarticular fragments and malalignment. Arthrosis and malunion might reduce outcome significantly. Additionally, cognitive impairment and insufficient hygiene might further increase the risk of pin tract infections (95,97).
Other viable techniques in elderly patients with osteoporotic bone might be the use of intramedullary nailing of the fibula as a minimally invasive technique alternative to ORIF of the fibula or as an additional technique to ORIF of the distal tibia (98).
In case geriatric patients do not have any prior medication for osteoporosis, geriatric patients with osteoporotic bone should postoperatively receive specific treatment as ankle fractures are also considered to be fragility fractures (99).
Overall, this vulnerable group of patients need thorough assessment preoperatively to assess comorbidities, health status and demand in everyday life to evaluate and plan the right treatment method to enable proper individual decision-making process.
Management and approaches—case presentations
Case 1: complex distal tibia fracture
A 70-year-old male presented to the emergency room after twisting his ankle with a severely swollen foot and ankle and no possibility for weight bearing. There was no gross deformity visible on first presentation. The initial radiograph showed a complex, intraarticular distal tibia fracture with a Weber B fracture of the distal fibula (44B3.1o). Due to the dislocation, slight comminution and already severely strained soft tissue the decision for immediate temporary ankle spanning EF was made. After spanning, CT scans were obtained in order to plan approaches and surgical treatment (Figure 1).
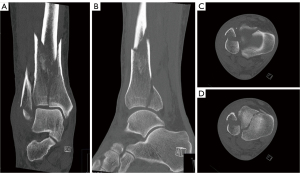
Nine days after initial trauma skin wrinkled around the ankle and therefore allowed for definite treatment.
Firstly, a posterolateral incision was used (Figure 2). With the patient in “instable lateral” position the incision is made between the lateral border of the Achilles tendon and the dorsal edge of the fibula. It is then continued along the dorsal tip of the lateral malleolus. Special consideration should go to identifying and protecting the sural nerve superficially and the peroneal neurovascular bundle on deep dissection. The hallucis longus muscle is elevated from the interosseus membrane and the peroneal tendons can be subluxed over the fibula if necessary to expose the posterolateral portion (Volkmann) of the distal tibia. With a longitudinal incision a posterior arthrotomy can be performed while preserving the posterior syndesmotic ligaments (74).

We used this approach as it allows good visualization of the fractured posterior malleolus and the possibility of simultaneously reducing and stabilizing the fibula fracture (100). After reduction of the posterior malleolar fragment and temporary fixation with a k-wire, it was retained with a 4.0 cannulated screw (Figure 2D).
In a second step, the distal fibula fracture was addressed with a locking plate due to the patient’s high age (Figure 2F). After thorough fluoroscopy and satisfactory reduction and fixation of the posterior malleolus fragment and the distal fibula, the wound was closed with sutures (Figure 3).
The patient was then turned into prone position. The second chosen approach was the anteromedial approach. The incision starts approximately 1.5 cm distal to the medial malleolus and advances proximal over the medial portion of the tibial plafond. The deep dissection then stays medial to the tibialis anterior tendon. The incision can be expanded proximally as far as the metaphyseal fracture line required (Figure 4) (101). An anatomically precontoured locking plate was placed onto the anterior face of the distal tibia and fixed with bicortical screws. No treatment of medial malleolus was necessary (Figure 5).


The patient was mobilized on the first day after surgery with a 20 kg weight bearing regimen and immobilization in a walker for six weeks.
Case 2: trimalleolar fracture
A 28-year-old patient presented to the emergency room after a fall at indoor climbing. Closed reduction was performed immediately on site by paramedics. Due to the high instability and redislocation upon presentation to the emergency room (Figure 6), the patient was transferred to the operation room to have temporary external fixation.
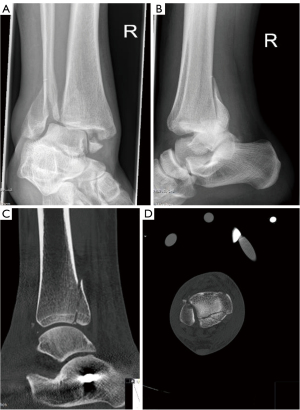
After spanning the ankle, CT was performed and showed a trimalleolar fracture with a multifragmentary, joint depression fracture of the posterior malleolus. Therefore, we chose to use a posterolateral approach for open reduction with direct visualization of the articular surface and the posterior malleolus in order to be able to reduce and fix the multifragmentary fracture in the young patient perfectly. The patient again was first positioned in an “instable lateral” position and after reduction the fracture of the posterior malleolus was fixed using a buttress plate. Secondly, the distal fibula fracture was also fixed via the posterolateral approach using a precontoured locking plate.
After ORIF of the posterior malleolus and the distal fibula via the posterolateral approach the fascia was closed, but wound closure was postponed in order to be able to examine the stability of the syndesmosis after ORIF of the medial malleolus. Therefore, the patient was turned into supine position. The medial malleolus was reduced with a mini-open incision distal to the tip of the medial malleolus and two canulated screws used for definite fixation (Figure 7). Afterwards, the stability of the tibiofibular syndesmosis was examined using fluoroscopy and no instability was detected, so wound closure was finalized.

Conclusions
The incidence of complex ankle fractures is rising and especially with the aging population, more elderly patients will present challenges to orthopedic surgeons.
Soft tissue condition dictates the course of treatment as complications and unfavorable outcome are mainly due to infections and wound healing problems. Thorough examination of preoperative CT scans is extremely important and a two-staged treatment protocol will still most likely be the most practical and valid treatment concept in order to ensure the best outcome.
Alternative treatment methods to ORIF such as EF as definite treatment or tibiotalocalcaneal nailing might present viable options in geriatric patients or in highly comminuted tibial pilon fractures with severe soft tissue injury.
Geriatric patient population will need to be focused on even more in the future and more thorough studies are necessary to reduce complication rates and improve quality of life for elderly patients.
However, further research is need into additional forms of soft tissue conditioning as soft tissue is still the most limiting factor when treating complex ankle fractures. Additionally, new implants and new forms of void filling technique could enhance treatment and allow for quicker mobilization, especially in the rising number of geriatric patients. Furthermore, we believe that improved techniques of MIO, even assisted by intraoperative CT or computer-assisted can present viable options for the future.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Albert T. Anastasio) for the series “Foot and Ankle Surgery” published in Annals of Translational Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1173/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1173/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1173/coif). The series “Foot and Ankle Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in two cases presented in this review were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for the publication of this case report and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Elsoe R, Ostgaard SE, Larsen P. Population-based epidemiology of 9767 ankle fractures. Foot Ankle Surg 2018;24:34-9. [Crossref] [PubMed]
- Luo TD, Eady JM, Aneja A, et al. Classifications in Brief: Rüedi-Allgöwer Classification of Tibial Plafond Fractures. Clin Orthop Relat Res 2017;475:1923-8. [Crossref] [PubMed]
- Chen H, Cui X, Ma B, et al. Staged procedure protocol based on the four-column concept in the treatment of AO/OTA type 43-C3.3 pilon fractures. J Int Med Res 2019;47:2045-55. [Crossref] [PubMed]
- Mauffrey C, Vasario G, Battiston B, et al. Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg 2011;77:432-40.
- Saad BN, Yingling JM, Liporace FA, et al. Pilon Fractures: Challenges and Solutions. Orthop Res Rev 2019;11:149-57. [Crossref] [PubMed]
- Liporace FA, Yoon RS. Decisions and staging leading to definitive open management of pilon fractures: where have we come from and where are we now? J Orthop Trauma 2012;26:488-98. [Crossref] [PubMed]
- Cutillas-Ybarra MB, Lizaur-Utrilla A, Lopez-Prats FA. Prognostic factors of health-related quality of life in patients after tibial plafond fracture. A pilot study. Injury 2015;46:2253-7. [Crossref] [PubMed]
- Juto H, Nilsson H, Morberg P. Epidemiology of Adult Ankle Fractures: 1756 cases identified in Norrbotten County during 2009-2013 and classified according to AO/OTA. BMC Musculoskelet Disord 2018;19:441. [Crossref] [PubMed]
- Thur CK, Edgren G, Jansson KÅ, et al. Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: a population-based study of 91,410 Swedish inpatients. Acta Orthop 2012;83:276-81. [Crossref] [PubMed]
- Pflüger P, Braun KF, Mair O, et al. Current management of trimalleolar ankle fractures. EFORT Open Rev 2021;6:692-703. [Crossref] [PubMed]
- Esposito JG, van der Vliet QMJ, Heng M, et al. Does Surgical Approach Influence the Risk of Postoperative Infection After Surgical Treatment of Tibial Pilon Fractures? J Orthop Trauma 2020;34:126-30. [Crossref] [PubMed]
- Mair O, Pflüger P, Hoffeld K, et al. Management of Pilon Fractures-Current Concepts. Front Surg 2021;8:764232. [Crossref] [PubMed]
- Schepers T, De Vries MR, Van Lieshout EM, et al. The timing of ankle fracture surgery and the effect on infectious complications; a case series and systematic review of the literature. Int Orthop 2013;37:489-94. [Crossref] [PubMed]
- Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: Open reduction and internal fixation versus tibio-talo-calcaneal nailing: Short-term results of a prospective randomized-controlled study. Injury 2017;48:519-24. [Crossref] [PubMed]
- Swierstra BA, van Enst WA. The prognosis of ankle fractures: a systematic review. EFORT Open Rev 2022;7:692-700. [Crossref] [PubMed]
- Bartoníček J, Rammelt S, Tuček M. Posterior Malleolar Fractures: Changing Concepts and Recent Developments. Foot Ankle Clin 2017;22:125-45. [Crossref] [PubMed]
- Mason LW, Marlow WJ, Widnall J, et al. Pathoanatomy and Associated Injuries of Posterior Malleolus Fracture of the Ankle. Foot Ankle Int 2017;38:1229-35. [Crossref] [PubMed]
- Dean DB. Field management of displaced ankle fractures: techniques for successful reduction. Wilderness Environ Med 2009;20:57-60. [Crossref] [PubMed]
- Ellanti P, Hammad Y, Kosutic D, et al. Irreducible tibial pilon fracture caused by incarceration of the fibula in the tibial medullary canal. J Foot Ankle Surg 2012;51:362-4. [Crossref] [PubMed]
- Cross WW 3rd, Swiontkowski MF. Treatment principles in the management of open fractures. Indian J Orthop 2008;42:377-86. [Crossref] [PubMed]
- Stapleton JJ, Zgonis T. Surgical treatment of tibial plafond fractures. Clin Podiatr Med Surg 2014;31:547-64. [Crossref] [PubMed]
- Tornetta P 3rd, Gorup J. Axial computed tomography of pilon fractures. Clin Orthop Relat Res 1996;273-6. [Crossref] [PubMed]
- Donken CC, Al-Khateeb H, Verhofstad MH, et al. Surgical versus conservative interventions for treating ankle fractures in adults. Cochrane Database Syst Rev 2012;CD008470. [Crossref] [PubMed]
- Blauth M, Bastian L, Krettek C, et al. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma 2001;15:153-60. [Crossref] [PubMed]
- Sitnik A, Beletsky A, Schelkun S. Intra-articular fractures of the distal tibia: Current concepts of management. EFORT Open Rev 2017;2:352-61. [Crossref] [PubMed]
- Newman SD, Mauffrey CP, Krikler S. Distal metadiaphyseal tibial fractures. Injury 2011;42:975-84. [Crossref] [PubMed]
- Zelle BA, Dang KH, Ornell SS. High-energy tibial pilon fractures: an instructional review. Int Orthop 2019;43:1939-50. [Crossref] [PubMed]
- Larsen P, Rathleff MS, Elsoe R. Surgical versus conservative treatment for ankle fractures in adults - A systematic review and meta-analysis of the benefits and harms. Foot Ankle Surg 2019;25:409-17. [Crossref] [PubMed]
- Xia X, Yang Z, Zhang Y, et al. Systematic review and meta-analysis: surgical reparative treatment for orthopedic patients with ankle fracture complicated by peripheral tissue injury. Ann Palliat Med 2021;10:8869-80. [Crossref] [PubMed]
- Lu V, Tennyson M, Zhang J, et al. Ankle fusion with tibiotalocalcaneal retrograde nail for fragility ankle fractures: outcomes at a major trauma centre. Eur J Orthop Surg Traumatol 2023;33:125-33. [Crossref] [PubMed]
- Haller JM, Githens M, Rothberg D, et al. Pilon Fractures in Patients Older Than 60 Years of Age: Should We Be Fixing These? J Orthop Trauma 2020;34:121-5. [Crossref] [PubMed]
- Pilskog K, Gote TB, Odland HEJ, et al. Association of Delayed Surgery for Ankle Fractures and Patient-Reported Outcomes. Foot Ankle Int 2022;43:762-71. [Crossref] [PubMed]
- Adamson S, Trickett R, Hodgson P, et al. Ankle fractures: impact of timing of surgery. Inj Extra 2009;10:224.
- Singh RA, Trickett R, Hodgson P. Early versus late surgery for closed ankle fractures. J Orthop Surg (Hong Kong) 2015;23:341-4. [Crossref] [PubMed]
- Naumann MG, Sigurdsen U, Utvåg SE, et al. Associations of timing of surgery with postoperative length of stay, complications, and functional outcomes 3-6 years after operative fixation of closed ankle fractures. Injury 2017;48:1662-9. [Crossref] [PubMed]
- Sirkin M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 1999;13:78-84. [Crossref] [PubMed]
- Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma 1999;13:92-7. [Crossref] [PubMed]
- Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma 1999;13:85-91. [Crossref] [PubMed]
- Tang X, Liu L, Tu CQ, et al. Comparison of Early and Delayed Open Reduction and Internal Fixation for Treating Closed Tibial Pilon Fractures. Foot Ankle Int 2014;35:657-64. [Crossref] [PubMed]
- Franke J, von Recum J, Suda AJ, et al. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am 2012;94:1386-90. [Crossref] [PubMed]
- Beck M, Brunk M, Wichelhaus A, et al. Intraoperative three-dimensional imaging in ankle syndesmotic reduction. BMC Musculoskelet Disord 2021;22:116. [Crossref] [PubMed]
- Assal M, Ray A, Stern R. The extensile approach for the operative treatment of high-energy pilon fractures: surgical technique and soft-tissue healing. J Orthop Trauma 2007;21:198-206. [Crossref] [PubMed]
- Tomás-Hernández J. High-energy pilon fractures management: State of the art. EFORT Open Rev 2016;1:354-61. [Crossref] [PubMed]
- Krettek C, Bachmann S. Pilon fractures. Part 2: Repositioning and stabilization technique and complication management. Chirurg 2015;86:187-201; quiz 202-3. [Crossref] [PubMed]
- Biz C, Angelini A, Zamperetti M, et al. Medium-Long-Term Radiographic and Clinical Outcomes after Surgical Treatment of Intra-Articular Tibial Pilon Fractures by Three Different Techniques. Biomed Res Int 2018;2018:6054021. [Crossref] [PubMed]
- Wu D, Peng C, Ren G, et al. Novel anterior curved incision combined with MIPO for Pilon fracture treatment. BMC Musculoskelet Disord 2020;21:176. [Crossref] [PubMed]
- Dresing K. Minimally invasive osteosynthesis of pilon fractures. Oper Orthop Traumatol 2012;24:368-82. [Crossref] [PubMed]
- Vidović D, Matejčić A, Ivica M, et al. Minimally-invasive plate osteosynthesis in distal tibial fractures: Results and complications. Injury 2015;46:S96-9. [Crossref] [PubMed]
- Vicenti G, Bizzoca D, Nappi VS, et al. The impact of lag screw in the healing time of distal tibia fractures treated with minimally invasive plate osteosynthesis: A randomized clinical trial. Injury 2020;51:S80-5. [Crossref] [PubMed]
- Millington SA, Grabner M, Wozelka R, et al. Quantification of ankle articular cartilage topography and thickness using a high resolution stereophotography system. Osteoarthritis Cartilage 2007;15:205-11. [Crossref] [PubMed]
- Erichsen JL, Andersen PI, Viberg B, et al. A systematic review and meta-analysis of functional outcomes and complications following external fixation or open reduction internal fixation for distal intra-articular tibial fractures: an update. Eur J Orthop Surg Traumatol 2019;29:907-17. [Crossref] [PubMed]
- Faber RM, Parry JA, Haidukewych GH, et al. Complications after fibula intramedullary nail fixation of pilon versus ankle fractures. J Clin Orthop Trauma 2021;16:75-9. [Crossref] [PubMed]
- Rouhani A, Elmi A, Akbari Aghdam H, et al. The role of fibular fixation in the treatment of tibia diaphysis distal third fractures. Orthop Traumatol Surg Res 2012;98:868-72. [Crossref] [PubMed]
- Goost H, Wimmer MD, Barg A, et al. Fractures of the ankle joint: investigation and treatment options. Dtsch Arztebl Int 2014;111:377-88. [Crossref] [PubMed]
- Huang Z, Liu L, Tu C, et al. Comparison of three plate system for lateral malleolar fixation. BMC Musculoskelet Disord 2014;15:360. [Crossref] [PubMed]
- Nguyentat A, Camisa W, Patel S, et al. A Biomechanical Comparison of Locking Versus Conventional Plate Fixation for Distal Fibula Fractures in Trimalleolar Ankle Injuries. J Foot Ankle Surg 2016;55:132-5. [Crossref] [PubMed]
- White TO, Bugler KE, Appleton P, et al. A prospective randomised controlled trial of the fibular nail versus standard open reduction and internal fixation for fixation of ankle fractures in elderly patients. Bone Joint J 2016;98-B:1248-52. [Crossref] [PubMed]
- Herrera-Pérez M, Martín-Vélez P, González-Martín D, et al. Tibiotalocalcaneal nailing for osteoporotic ankle fractures in the frail patient: a narrative review with a clinical score proposal for the decision-making process. EFORT Open Rev 2022;7:328-36. [Crossref] [PubMed]
- Hong CC, Tan SHS, Saha S, et al. Fibula fixation in the treatment of tibial pilon fractures - Is it really necessary? Foot Ankle Surg 2022;28:891-7. [Crossref] [PubMed]
- Bear J, Rollick N, Helfet D. Evolution in Management of Tibial Pilon Fractures. Curr Rev Musculoskelet Med 2018;11:537-45. [Crossref] [PubMed]
- Krettek C, Bachmann S. Pilon fractures. Part 1: Diagnostics, treatment strategies and approaches. Chirurg 2015;86:87-101; quiz 102-4. [Crossref] [PubMed]
- Howard JL, Agel J, Barei DP, et al. A prospective study evaluating incision placement and wound healing for tibial plafond fractures. J Orthop Trauma 2008;22:299-305; discussion 305-6. [Crossref] [PubMed]
- Bartoníček J, Rammelt S, Kostlivý K, et al. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 2015;135:505-16. [Crossref] [PubMed]
- Büchler L, Tannast M, Bonel HM, et al. Reliability of radiologic assessment of the fracture anatomy at the posterior tibial plafond in malleolar fractures. J Orthop Trauma 2009;23:208-12. [Crossref] [PubMed]
- Meijer DT, de Muinck Keizer RJ, Doornberg JN, et al. Diagnostic Accuracy of 2-Dimensional Computed Tomography for Articular Involvement and Fracture Pattern of Posterior Malleolar Fractures. Foot Ankle Int 2016;37:75-82. [Crossref] [PubMed]
- Gardner MJ, Brodsky A, Briggs SM, et al. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2006;165-71. [Crossref] [PubMed]
- Baumbach SF, Herterich V, Damblemont A, et al. Open reduction and internal fixation of the posterior malleolus fragment frequently restores syndesmotic stability. Injury 2019;50:564-70. [Crossref] [PubMed]
- Verhage SM, Hoogendoorn JM, Krijnen P, et al. When and how to operate the posterior malleolus fragment in trimalleolar fractures: a systematic literature review. Arch Orthop Trauma Surg 2018;138:1213-22. [Crossref] [PubMed]
- Odak S, Ahluwalia R, Unnikrishnan P, et al. Management of Posterior Malleolar Fractures: A Systematic Review. J Foot Ankle Surg 2016;55:140-5. [Crossref] [PubMed]
- Terstegen J, Weel H, Frosch KH, et al. Classifications of posterior malleolar fractures: a systematic literature review. Arch Orthop Trauma Surg 2023;143:4181-220. [Crossref] [PubMed]
- Marques Ribeiro H, Silva J, Teixeira R, et al. Clinical outcomes and trans-syndesmotic screw frequency after posterior malleolar fracture osteosynthesis. Injury 2021;52:633-7. [Crossref] [PubMed]
- Shi HF, Xiong J, Chen YX, et al. Comparison of the direct and indirect reduction techniques during the surgical management of posterior malleolar fractures. BMC Musculoskelet Disord 2017;18:109. [Crossref] [PubMed]
- Vidović D, Elabjer E, Muškardin IVA, et al. Posterior fragment in ankle fractures: anteroposterior vs posteroanterior fixation. Injury 2017;48:S65-9. [Crossref] [PubMed]
- Tornetta P 3rd, Ricci W, Nork S, et al. The posterolateral approach to the tibia for displaced posterior malleolar injuries. J Orthop Trauma 2011;25:123-6. [Crossref] [PubMed]
- Heyes GJ, Khashkhusha TR, Mason L. Posterolateral Approach to Posterior Malleolar Fractures: A Literature Review. Foot Ankle Spec 2023;16:149-58. [Crossref] [PubMed]
- Passias BJ, Korpi FP, Chu AK, et al. Safety of Early Weight Bearing Following Fixation of Bimalleolar Ankle Fractures. Cureus 2020;12:e7557. [Crossref] [PubMed]
- Myers DM, Pulido SH, Forsting S, et al. Effect of Early Weight Bearing on Outcomes After Open Reduction and Internal Fixation of Trimalleolar Ankle Fractures. Orthopedics 2021;44:160-5. [Crossref] [PubMed]
- Williams CE, Joo P, Oh I, et al. Arthroscopically Assisted Internal Fixation of Foot and Ankle Fractures: A Systematic Review. Foot Ankle Orthop 2021;6:2473011420950214. [Crossref] [PubMed]
- Feng SM, Sun QQ, Wang AG, et al. "All-Inside" Arthroscopic Treatment of Tillaux-Chaput Fractures: Clinical Experience and Outcomes Analysis. J Foot Ankle Surg 2018;57:56-9. [Crossref] [PubMed]
- Chiang CC, Tzeng YH, Jeff Lin CF, et al. Arthroscopic Reduction and Minimally Invasive Surgery in Supination-External Rotation Ankle Fractures: A Comparative Study With Open Reduction. Arthroscopy 2019;35:2671-83. [Crossref] [PubMed]
- Galante VN, Vicenti G, Corina G, et al. Hybrid external fixation in the treatment of tibial pilon fractures: A retrospective analysis of 162 fractures. Injury 2016;47:S131-7. [Crossref] [PubMed]
- Papadokostakis G, Kontakis G, Giannoudis P, et al. External fixation devices in the treatment of fractures of the tibial plafond: a systematic review of the literature. J Bone Joint Surg Br 2008;90:1-6. [Crossref] [PubMed]
- Osman W, Alaya Z, Kaziz H, et al. Treatment of high-energy pilon fractures using the ILIZAROV treatment. Pan Afr Med J 2017;27:199. [Crossref] [PubMed]
- Endres T, Grass R, Biewener A, et al. Advantages of minimally-invasive reposition, retention, and Ilizarov-(hybrid)fixation for pilon-tibial-fractures fractures with particular emphasis on C2/C3 fractures. Unfallchirurg 2004;107:273-84. [Crossref] [PubMed]
- Harris AM, Patterson BM, Sontich JK, et al. Results and outcomes after operative treatment of high-energy tibial plafond fractures. Foot Ankle Int 2006;27:256-65. [Crossref] [PubMed]
- Pugh KJ, Wolinsky PR, McAndrew MP, et al. Tibial pilon fractures: a comparison of treatment methods. J Trauma 1999;47:937-41. [Crossref] [PubMed]
- Richards JE, Magill M, Tressler MA, et al. External fixation versus ORIF for distal intra-articular tibia fractures. Orthopedics 2012;35:e862-7. [Crossref] [PubMed]
- Wang C, Li Y, Huang L, et al. Comparison of two-staged ORIF and limited internal fixation with external fixator for closed tibial plafond fractures. Arch Orthop Trauma Surg 2010;130:1289-97. [Crossref] [PubMed]
- Lim JA, Thahir A, Zhou AK, et al. Definitive management of open pilon fractures with fine wire fixation. Injury 2020;51:2717-22. [Crossref] [PubMed]
- Mehta N, Graham S, Lal N, et al. Fine wire versus locking plate fixation of type C pilon fractures. Eur J Orthop Surg Traumatol 2022;32:875-82. [Crossref] [PubMed]
- Daniels NF, Lim JA, Thahir A, et al. Open Pilon Fracture Postoperative Outcomes with Definitive Surgical Management Options: A Systematic Review and Meta-analysis. Arch Bone Jt Surg 2021;9:272-82. [Crossref] [PubMed]
- Kannus P, Palvanen M, Niemi S, et al. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970-2000 and projections for the future. Bone 2002;31:430-3. [Crossref] [PubMed]
- Rammelt S. Management of ankle fractures in the elderly. EFORT Open Rev 2016;1:239-46. [Crossref] [PubMed]
- Meijer RPJ, Halm JA, Schepers T. Unstable fragility fractures of the ankle in the elderly: Transarticular Steinmann pin or external fixation. Foot (Edinb) 2017;32:35-8. [Crossref] [PubMed]
- Nozaka K, Miyakoshi N, Saito H, et al. Effectiveness of Ilizarov external fixation in elderly patients with pilon fractures. J Orthop Sci 2021;26:254-60. [Crossref] [PubMed]
- Grote CW, Tucker W, Stumpff K, et al. Primary Arthrodesis for Diabetic Ankle Fractures. Foot Ankle Orthop 2020;5:2473011420908841. [Crossref] [PubMed]
- Hennings R, Spiegl UJ, Fakler JKM, et al. The AO triangular external fixator: a backup option in the treatment of ankle fractures in geriatric patients? Eur J Orthop Surg Traumatol 2021;31:719-27. [Crossref] [PubMed]
- Zyskowski M, Wurm M, Greve F, et al. A Prospective Randomized Study Comparing Functional Outcome in Distal Fibula Fractures between Conventional AO Semitubular Plating and Minimal Invasive Intramedullary "Photodynamic Bone Stabilisation". J Clin Med 2022;11:7178. [Crossref] [PubMed]
- Roux S, Cabana F, Carrier N, et al. Risk of Subsequent Fragility Fractures Observed After Low-Trauma Ankle Fractures. Calcif Tissue Int 2018;103:62-70. [Crossref] [PubMed]
- Amorosa LF, Brown GD, Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma 2010;24:188-93. [Crossref] [PubMed]
- Assal M, Ray A, Stern R. Strategies for surgical approaches in open reduction internal fixation of pilon fractures. J Orthop Trauma 2015;29:69-79. [Crossref] [PubMed]



