A systematic review of capsule aspiration in capsule endoscopy
Highlight box
Key findings
• Aspiration of capsule endoscopy (CE) is a rare adverse event that can be safely managed.
What is known and what is new?
• CE is widely accepted for intestinal investigations, and extensive research has been conducted on complication rates.
• This review shows that only a small percentage of patients experience capsule aspiration.
What is the implication, and what should change now?
• Aspirations of CE should not discourage patients undergoing the procedure.
• However, in specific patient groups, the possibility of aspiration should be anticipated, and appropriate precautions should be taken beforehand.
Introduction
Capsule endoscopy (CE) is considered a safe and widely accepted first-line method for investigating the small bowel (SB) due to its noninvasive and patient-friendly benefits (1). Recently, CE has been introduced for colon investigations and is considered an alternative to colonoscopy in specific clinical circumstances, with a high success rate, low complication rates and patient preference (2). The most common complication of small bowel capsule endoscopy (SBCE) is capsule retention which occurs in 1–2% of patients being evaluated for obscure gastrointestinal bleeding (OGIB) (3). Therefore, safety measures are established to exclude certain patients, minimizing retention risk. This includes patency capsules and cross-sectional imaging before investigation (4). Given that the capsule is ingested orally, possibility of aspiration should always be taken into consideration. Another study found capsule aspirations to be rare and often reported as isolated cases, mostly in elderly male patients with comorbidities (5). With the accumulating comorbidities, the increasingly prevalent ageing populations, the continuous advancement in CE technology and its increasing utilization as a diagnostic tool for both SB and colon, the number of complications may increase accordingly. Furthermore, it is crucial to identify and anticipate this complication in specific patient populations so that the required precautions can be taken. Therefore, necessary protocols should be established to carefully select the appropriate patients for the correct test. To offer an updated overview of the complication of capsule aspiration in CE, this systematic review collated the existing data. We present this article in accordance with the PRISMA reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-23-763/rc).
Methods
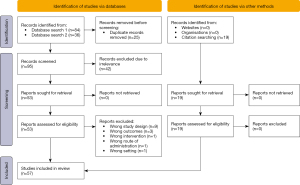
A systematic literature search was performed using the database PubMed with search terms ‘capsule endoscopy’, and ‘aspiration’ searched as keywords and MeSH from January 1, 1996, through October 30, 2022. An additional search was performed in the PubMed database on November 12, 2022. To ensure thoroughness and consistency, the search strategy used in this additional search was borrowed from another article (3). The specific search string, which includes keywords related to CE detection, completion, and/or retention rates based on MeSH, can be found in Appendix 1. By borrowing the search string from a previously published article, we aimed to benefit from an established and effective search strategy that had already been used successfully in the literature. This helps to ensure that the search is comprehensive, and no relevant articles are overlooked. All searches were performed without language restrictions. The initial screening process involved assessing titles and abstracts, followed by retrieving and independently reviewing the full texts of the shortlisted articles by two authors (Thorndal C and Selnes O). Relevant observational cohort studies that reported aspiration as one of the complications/outcomes were included, as well as case reports and case series on capsule aspiration. Manual citation search was also performed. Where appropriate, data extraction and statistical analyses were done using Microsoft Excel 2010 (Microsoft Corp., Redmond, WA, USA). Numerical results are reported as mean ± standard deviation (SD) and/or range.
Results
Using the above search strategy, 57 references were identified, presenting 63 cases of aspirated capsules. A total of 12 references were observational studies that reported information on capsule aspiration and the total number of CE performed in their patient groups; the remaining 45 were case reports or series. Detailed visualization of the search strategy and results are shown in Figure 1. Furthermore, Table 1 presents a detailed summary of all 45 cases of capsule aspiration, along with six of the observational studies that provided comprehensive reporting on aspiration cases. In addition, the 12 observational studies are summarized in Table 2.
Table 1
| References | Age (years), Sex | Comorbidities | History of dysphagia | Indication for CE examination | Difficulty swallowing capsule | Capsule model |
Ingestion symptoms | Symptoms during CE investigation | Symptoms after handling of aspiration | Time CE was aspirated | Anatomical location | Self-resolved or intervention | Identification of aspiration |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schneider et al. (6) | 64, M | MVR (mechanical) underweight | No | IDA | Yes | M2A | Immediate cough | No | No | 2 min | Right main bronchus | Yes | Symptoms |
| Tabib et al. (7) | 87, M | Bladder cancer, CCF, AF, CAD, CKD | No | IDA, FOBT+ | Yes | – | Immediate sensation in throat | Sensation in throat | – | – | Right main bronchus | No, rigid bronchoscopy, grasper forceps, FB basket | Symptoms, fluoroscopy |
| Sinn et al. (8) | 69, F | – | No | IDA, OGIB | Yes | M2A | Immediate cough | No | No | 50 sec | Bifurcation trachea | Yes | Reviewing data |
| Buchkremer et al. (9) | 74, M | Ankylosing spondylitis | No | IDA, weight loss, chronic diarrhoea | No | M2A | Immediate dyspnea | Dyspnea | No | 2 days | Right main bronchus | No, flexible bronchoscopy | Symptoms |
| Sepehr et al. (10) | 67, M | HTN, DM, CVA | Yes | OGIB | Yes | M2A | Immediate cough, dyspnea, tachypneic, tachycardic | No | No | – | Left main bronchus | No, bronchoscopy, Roth net |
Symptoms, real time viewing |
| Nathan and Biernat (11) | 93, M | None | No | OGIB | Yes | – | Immediate cough | No | No | 8 hours | Bronchus (NS) | Yes | Reviewing data |
| Shiff et al. (12) | 75, M | None | No | IDA | Yes | PillCam | Immediate cough | – | – | Sec–min | Right main bronchus | Yes | Symptoms |
| Guy et al. (13) | 90, M | CVA | No | IDA, melena | No | – | No | No | No | 1–2 days | Bronchus (NS) | No, rigid bronchoscopy, FB basket | Reviewing data |
| Leeds et al. (14) | 85, M | – | No | IDA | Yes | – | No | No | No | 8 hours | Bronchus (NS) | Yes | Reviewing data |
| Koulaouzidis et al. (15) | 76, M | – | – | IDA | No | PillCam SB | Immediate cough | No | No | 15 sec | – | Yes | Reviewing data |
| Bredenoord et al. (16) | 65, M | Resection of SC, diverticular disease, carcinoid tumor (ileum) | Yes | Carcinoma investigation | Yes | – | Immediate cough, dysphagia | No | No | – | Right main bronchus | Yes | Reviewing data |
| Jindal et al. (17) | 68, M | – | No | IDA, OGIB | Yes | PillCam | Immediate cough | No | No | 50 sec | Bronchus (NS) | Yes | Reviewing data |
| Fan et al. (18) | 81, M | Emphysema, bronchitis, gastritis, ankylosing spondylitis | No | Weight loss, poor appetite, night sweat | Yes | OMOM | Immediate desaturation, tachypnoea | – | – | – | Right main bronchus | No, bronchoscopy, extraction basket | Real time viewing |
| Hill et al. (19) | 89, M | Anticoagulation treatment | – | IDA, OGIB | Yes | – | No | No | No | 8 hours | Right main bronchus | No, bronchoscopy | Reviewing data |
| Kurtz et al. (20) | 73, M | RCC, MVR (tissue), hyperlipidemia | No | IDA, OGIB | No | – | Cough, sensation in throat after 2 min | No | No | – | Right main bronchus | No, bronchoscopy, FB basket | Real time viewing |
| Depriest et al. (21) | 90, M | CAD, AF, PVD, CVA, COPD | No | IDA, OGIB | No | – | Immediate cough | No | No | – | Left main bronchus | No, bronchoscopy | Initial post procedure chest X-ray |
| Choi et al. (22) | 75, M | CVA | No | OGIB | No | PillCam SB | Immediate cough | No | No | 2 hours | Left main bronchus | No, bronchoscopy, Roth net, grasper forceps | Initial post procedure chest X-ray |
| Pezzoli et al. (23) | 82, M | HTN | No | IDA | No | – | No | Cough | No | 2 days | Left main bronchus | Yes | Reviewing data |
| Lucendo et al. (24) | 80, M | PD, DM | No | IDA, FOBT+ | Yes | PillCam SB | Immediate cough, dyspnea | No | No | 20 sec | Trachea (carina) | Yes | Reviewing data |
| Shafi et al. (25) | 67, M | HH, gastritis, diverticular disease, hemorrhoids | No | IDA, abdominal pain | No | – | No | Dyspnea after a few days | - | – | Right main bronchus | No, bronchoscopy | Symptoms |
| Lu et al. (26) | 85, M | Gastritis and inflammation in descending and SC | No | IDA, melaena | Yes | OMOM | Immediate cough | No | No | – | NS | Yes, with cough encouragement | Real time viewing |
| Girdhar et al. (27) | 83, M | COPD, GORD | No | IDA | – | PillCam SB2 | Cough | Dyspnea after 1 hour | No | – | Left main bronchus | No, bronchoscopy, FB basket | Real time viewing |
| Parker et al. (28) | 77, F | Hysterectomy, HH (oesophagus) | No | IDA, abdominal pain, weight loss | No | – | Immediate choking episode, cough | No | Massive intracranial haemorrhage hours later, deceased | – | NS | Yes | Symptoms |
| Yarlagadda et al. (29) | 80, M | AF, CVA | – | IDA, melena | No | M2A | No | No | – | – | Left main bronchus | No, bronchoscopy, FB basket | Reviewing data |
| Despott et al. (30) | 65, M | ALD, chronic pancreatitis, COPD, gastric varices | No | IDA, OGIB | No | – | No | No | No | – | Right main bronchus | No, grasper forceps | Real time viewing |
| Despott et al. (30) | 73, M | COPD | – | IDA | Yes | – | Immediate cough | No | No | – | Left main bronchus | No, Roth net | Real time viewing |
| Despott et al. (30) | 81, M | None | – | IDA | Yes | – | Immediate choking sensation | No | No | – | Right main bronchus | No, rigid bronchoscopy, grasper forceps | Real time viewing |
| Singh et al. (31) | 56, M | Mild COPD, HTN, Gout, CVA (left) | No | IDA | No | – | No | Progressive dyspnea over 2 weeks, cough | No | 6 weeks | Right main bronchus | No, grasper forceps | Symptoms |
| Sánchez-Chávez and Martínez-García (32) | 78, M | Gastric ulcer | No | OGIB, postprandial fullness, weight loss | Yes | PillCam COLON1 | Immediate sensation in throat, cough | No | No | Few min | Bifurcation trachea | Yes | Reviewing data |
| Pereira et al. (33) | 78, M | CKD on hemodialysis | – | OGIB | Yes | PillCam SB | Immediate cough | No | No | 2 min 15 sec | Bronchus (NS) | Yes | Reviewing data |
| Hall et al. (34) | 69, M | – | – | OGIB | – | PillCam | No | Cough 1 week after | No | 7 days | Right main bronchus | No, flexible bronchoscopy, net | Symptoms |
| Ding et al. (35) | 80, M | COPD, previous DU and angioectasia | – | IDA | No | – | Immediate cough | No | No | – | Right main bronchus | Yes, but Bronchoscopy, fell into Left main bronchus, then expectorated by patient | Symptoms |
| Ding et al. (35) | 88, M | Previous gastric angiodysplasia | – | IDA | No | – | Immediate cough, dyspnea | No | No | 2 hours 42 min |
Trachea | Yes | Symptoms, reviewing data |
| Hussan et al. (36) | 83, M | CKD, myelodysplasia | Yes | IDA | Yes | – | Immediately regurgitated, before manually pushing capsule down hypopharynx | No | No | 30 hours | Right main bronchus | No, fiberoptic flexible bronchoscopy | Reviewing data |
| Elmunzer et al. (37) | 83, M | Aspiration pneumonia, HH, CAD, AVR, PD, dementia | Yes | IDA, melena | Yes | – | Immediate cough | No | No | 3 hours | Right main bronchus | No, fiberoptic bronchoscopy, endoscopic snare | Real time viewing |
| Mannami et al. (38) | 85, M | DM, HTN, AF, distal gastrectomy | No | IDA, OGIB | Yes | PillCam SB2 | Immediate sensation in throat | No | No | 220 sec | Bronchus (NS) | Yes | Reviewing data |
| Magalhães-Costa et al. (39) | 92, M | PD, DM | No | OGIB | No | PillCam SB2 | No | Dyspnea, cough, capsule expelled | No | 4 hours | Mouth and pharynx | Yes | Symptoms, reviewing data |
| Amarna et al. (40) | 81, M | – | – | – | No | – | Immediate cough | No | No | 110 days | Left main bronchus | No, flexible fiberoptic bronchoscopy, snare wire loop |
Chest X-ray, reviewing data |
| Choi et al. (41) | 82, M | – | No | Chronic diarrhoea, abdominal pain | No | OMOM | Immediate cough | No | No | – | Right main bronchus | No, FB basket | Real time viewing |
| Juanmartiñena Fernández et al. (42) | 82, M | – | No | IDA | Yes | – | Cough | Cough, 12 hours later fever, leukocytosis, dyspnea | Fever, leukocytosis, dyspnea | 25 min | Bronchus (NS) | Yes | Reviewing data |
| Juanmartiñena Fernández et al. (43) | 81, M | Alzheimer, antiplatelet drug therapy | No | Melena | No | – | Immediate cough | No | No | 17 sec | Tracheo-bronchial system | Yes | Reviewing data |
| Buscot et al. (44) | 74, M | CVA, COPD | No | IDA | No | PillCam SB2 | Immediate choking episode, dyspnea, cough, desaturation | Dyspnea, coughing, desaturation | No | – | Left main bronchus | No, FB basket | Real time viewing |
| Ribaldone et al. (45) | 75, M | – | No | IDA+ FOBT+ | No | PillCam SB2 | No | No | No | 7 hours | Trachea | Yes | Reviewing data |
| Skouras et al. (46) | 72, M | IBD, previous SB perforation, ileostomy, DM | No | High output stoma | No | PillCam SB2 | No | No | No | 30 min | Bifurcation trachea | No, retrieved with gastroscope and put into duodenum | Real time viewing |
| Keil-Ríos et al. (47) | 84, M | – | – | Fever, thickening of ileum | No | PillCam SB | No | Cough, capsule expelled | No | 10 hours | Bronchus (NS) | Yes | Symptoms, reviewing data |
| Arroyo-Mercado and Martinez (48) | 84, M | HTN, CAD, CCF, OA | No | IDA | No | – | No | No | No | 9 min | Trachea (carina) | No, cough, hand thrust maneuver to midback, expulsed capsule | Real time viewing |
| Dan et al. (49) | 67, M | Emphysema and cardiomegaly | No | Nausea | No | Ankon | No | Cough, dyspnea | – | 19 min | Bifurcation trachea; then bronchus (NS) | Yes | Real time viewing |
| Hilewitz et al. (50) | 85, M | CAD | – | IDA | No | PillCam | Immediate cough | Cough | – | 5 days | Right main bronchus | No, bronchoscopy, snare | Reviewing data |
| Rutazaana et al. (51) | 67, M | Developmental delay | – | IDA | Yes | PillCam SB3 | Immediate dyspnea | No | – | – | Right main bronchus | No, bronchoscopy | Symptoms |
| Takeda et al. (52) | 77, M | SC and partial SB resection, gastrectomy, chronic right pneumothorax, CVA | – | IDA, OGIB | Yes | PillCam Patency capsule | Immediate dyspnea, desaturation | Dyspnea, desaturation | No | 7 hours | Bronchus (NS) | No, flexible bronchoscopy, balloon catheter | Symptoms |
| Egger et al. (53) | 69, M | Metastatic small cell lung cancer, DVT | No | IDA, melena | No | M2A | Sensation in throat | No | No | 72 min | Pharynx | No, EGD with SDAC, advancing capsule to stomach | Real time viewing |
| Tamang and Mitnovetski (54) | 87, M | – | – | IDA, FOBT+ | No | PillCam SB3 | Immediate cough, desaturation | Cough, desaturation | No | – | Right main bronchus | No, flexible bronchoscopy, endotracheal tube, fogarty catheters | Symptoms, real time viewing |
| Gaisinskaya et al. (55) | 92, M | Gout, myelodysplastic syndrome, CKD | – | IDA, FOBT+ | Yes | – | No | No | No | 1 day | Bronchus (NS) | No, bronchoscopy | Reviewing data |
| Gomez et al. (56) | 83, M | CAD, CVA | – | IDA | No | – | No | Yes | No | 1 day | Right main bronchus | No, bronchoscopy, loop snare | Reviewing data |
M, male; F, female; CE, capsule endoscopy; MVR, mitral valve replacement; IDA, iron deficiency anemia; CCF, congestive cardiac failure; AF, atrial fibrillation; CAD, coronary artery disease; CKD, chronic kidney disease; FOBT+, fecal occult blood test positive; FB, foreign body; OGIB, occult gastrointestinal bleeding; HTN, hypertension; DM, diabetes mellitus; CVA, cerebrovascular accident; NS, not specified; M2A, Mouth to Anus; SC, sigmoid colon; SB, small bowel; RCC, renal cell carcinoma; PVD, peripheral vascular disease; COPD, chronic obstructive pulmonary disease; GORD, gastroesophageal reflux disease; PD, Parkinson disease; HH, hiatal hernia; ALD, alcohol induced liver disease; DU, duodenal ulcer; AVR, aortic valve repair; IBD, inflammatory bowel disease; OA, osteoarthritis; DVT, deep vein thrombosis; EGD, esophagogastroduodenoscopy; SDAC, Steris distal attachment cap.
Table 2
| References | Number of centres | Total CE in cohort | Capsule modality | Number of aspirations | Comments |
|---|---|---|---|---|---|
| Tabib et al. (7) | 1 | 600 | SB | 1 | See Table 1 |
| Rondonotti et al. (57) | 4 | 733 | NR | 1 | Capsule coughed up |
| Shiff et al. (12) | 1 | >1,000 | SB | 1 | See Table 1 |
| Bredenoord et al. (16) | 1 | >1,000 | SB | 1 | See Table 1 |
| Koulaouzidis et al. (15) | 1 | >2,000 | SB | 1 | See Table 1 |
| Girelli et al. (58) | 2 | 267 | SB | 1 | No symptoms before or after; remained in trachea for 18 hours, then expulsed by cough |
| Li et al. (59) | 1 | 427 | SB | 2 | Retrieved via bronchoscopy; both patients were elderly, with a higher risk of laryngeal swallowing difficulty |
| Ding et al. (35) | 1 | About 300 | SB | 2 | See Table 1 |
| Sanchez-Chavez and Martinez-Garcia (32) | 1 | >200 | SB | 1 | See Table 1 |
| Soncini et al. (60) | 30 | 1,667 | SB | 1 | Transient, self-resolved |
| Pezzoli et al. (61) | 1 | 900 | SB | 2 | Tracheal aspiration; both over 80 years of age |
| Fernández-Urién et al. (62) | 12 | 5,428 | Oesophageal, SB & colon | 2 | Both no history of dysphagia |
CE, capsule endoscopy; SB, small bowel; NR, not reported.
Patient and procedural information
Of the 63 cases of capsule aspiration, 52 (82.5%) occurred in male patients, with a mean age of 78.2±8.4 years (range, 56–93). In 19 (30%) patients, comorbidities were not reported; of the remainder (n=44), 40 (63.5%) had comorbidities reported, and 4 (6.3%) had no specified comorbidities. Only 4 (6.3%) patients had a history of previous dysphagia; all were males above 65 years of age with severe preexisting comorbidities. Patient’s physical condition was not well reported, but 6 (9.5%) patients were reported to be frail (6,10,18,24,30,38). Two patients reported physical conditions as good (14,25), and 1 reported intact function based on neurological examination (22). Twenty-four cases (38%) reported patients having difficulties swallowing the capsule, and 6 (9.5%) reported more than one attempt needed. Most reports did not specify the position in which the patient ingested the capsule. Still, 3 reported the patient in an upright position (17,20,30), one standing (24) and one in a supine position with a pillow under the head (49). The most common indication for CE was iron deficiency anemia (IDA), with 39 (61.9%) cases reporting this; secondly was OGIB in 15 (23.8%) cases. In addition, 59 (93.6%) patients had SB investigations; the remaining 4 cases did not specify the modality of the CE.
Models of the CE
In 23 (36.5%) cases, the company and model of CE used were not specified. Thirty-two (50.8%) patients were examined using capsules from Given Imaging Ltd. (now Medtronic, Minneapolis, MN, USA): 7 used Mouth to Anus (M2A) capsules, 6 used PillCam SB, 6 used PillCam SB2, 2 used PillCam SB3, 1 used PillCam COLON1, 1 used PillCam patency capsule and the remainder were unspecified. In addition, there were 3 cases of aspiration of OMOM [Chongqing Jinshan Science and Technology (Group) Co., Ltd., Chongqing, China] and 1 case of aspiration of Ankon Technologies Co., (Shanghai, China).
Presentation of capsule aspiration
Thirty-nine (61.9%) patients experienced symptoms of aspiration as they ingested the capsule. Among the patients, coughing was the most prevalent symptom, reported in 28 cases (71.8%), followed by dyspnea in 7 (17.9%) and 5 (12.8%) patients experiencing a foreign body sensation in the throat. Four patients desaturated, and 2 required supplemental oxygen. In 37 (94.8%) patients, the symptoms of aspiration occurred immediately or within a few minutes following ingestion; in the remaining, the symptoms manifested hours, days or, for some, even weeks later. Thirty-six (57%) patients were reported asymptomatic following the CE investigation, even though 27 (75%) had experienced ingestion symptoms. Fifteen (23.8%) cases were reported as having symptomatic CE investigations, with 6 (53.3%) developing dyspnea. The remaining cases had either a lack of information regarding the outcome of the investigations, or the capsule was removed due to immediate aspiration symptoms. Out of total capsules, 44 (69.8%) were found in the bronchial system, with the right main bronchus being the most common anatomical location in 21 (47.7%) cases. However, in 9 (20.4%) cases, the capsule was detected in the left main bronchus, while 10 (22.7%) capsules were lodged in the trachea, and two were found in the pharynx. The remainder did not specify the bronchial location. Among the patients, 16 (25.4%) experienced transient aspiration that lasted only second to minutes, and all cases resolved spontaneously. The duration of aspiration varied significantly between patients, with the longest recorded case lasting 110 days (40).
Handling of capsule aspiration and outcomes
Thirty-one (49.2%) patients needed intervention for retrieval of the capsule. Twenty-one (67.7%) of them were symptomatic at ingestion of the capsule. In 29 (93.5%) patients, bronchoscopy served as the primary approach for managing capsule aspiration. In 1 patient, the bronchoscopy was unsuccessful: the capsule fell into the left bronchus and was expectorated by the patient (35). In 1 patient, the capsule was retrieved with a bronchoscope and a foreign body basket, and then replaced in the gastrointestinal tract using the bronchoscope and forceps (44). Another patient had their capsule replaced by a gastroscope to the duodenum from the trachea (46). Of the 24 (38%) patients with self-resolved cases of aspiration, 15 (62.5%) patients coughed up the capsule resulting in termination of the examination. Thirteen (86.6%) patients coughed up the capsule within minutes, and the remaining 2 (13.4%) coughed up the capsule hours after ingestion. Twenty-five (39.7%) cases detected aspiration from reviewing the capsule data afterwards, and 16 (25.4%) were detected due to real-time viewing. In 2 patients, initial post-procedure chest X-rays were done to locate the capsule, and in 16 (25.4%) cases, the patients were so symptomatic that aspiration was presumed clinically. Post-aspiration outcomes were reported in 47 (74.6%) cases, but only two patients had symptoms. One patient developed aspiration pneumonia 12 hours after the aspiration, which was only noted by reviewing the video. He was effectively treated with antibiotics (42). Another patient managed to cough up the capsule shortly after ingestion, but she died soon after the examination due to a massive intracranial hemorrhage (28). This case represents the sole recorded fatality. The remaining patients (95.7%) experienced recovery without any complications.
Aspiration rate
Twelve studies reported cases of capsule aspiration from a total of 56 centres, see Table 2 for specifications. While the exact number of CE examinations conducted is unknown, there were approximately 14,522 CE examinations, among which only 16 cases of aspiration were reported. This indicates a remarkably low estimated rate of just 0.1%.
Discussion
The present review found that capsule aspiration is rare. It seems that aspiration primarily occurs among elderly male patients who have multiple comorbidities. In total, 39 cases were reported as symptomatic, with cough being the most frequent symptom and 94.8% having symptoms immediately. However, no significant respiratory compromise has ever been recorded. The most frequent indication was IDA, with the right main bronchus being the most common anatomical location involved. Among the patients who experienced capsule aspiration, slightly less than half required an intervention for capsule removal. In this series of capsule aspiration cases, bronchoscopy served as the primary approach for managing capsule aspiration, demonstrating a high success rate. 39.7% of capsules were discovered when reviewing data, and 25.9% with real-time viewing. A total of 95.7% of patients recovered uneventfully. This review outlines a particular patient group where aspirations should be anticipated. Therefore, capsule administration, should be approached with precautions, and the need for stronger justification is indicated in this high-risk group. If specific precaution plans should be made for at-risk patients, the real time viewer would be a great attribute. It shows images during ongoing examination (63) and has been used more frequently in recent years. In this review, a total of 16 capsule aspirations was identified using the real time viewer, which allowed the clinicians to investigate whether the capsule was swallowed correctly. The real-time viewer has primarily been used to monitor the location of the capsule during the phases of the procedure, where delayed transit is common, and coupled it with early preventive interventions, which has significantly enhanced completion rate and positive finding rate (64,65). Real-time viewing could change the management of aspirations, where an immediate reading could save time before interventions and secure early detection, as the European Society of Gastrointestinal Endoscopy recommends (66). This review shows almost no patients experienced complications post-aspiration. However, 1 patient did noteworthy get aspiration pneumonia 12 hours after ingestion, and it was only noted due to reviewing the data. This rare case could potentially have been solved earlier, with the real-time viewer (42). It is noteworthy that the use of real time viewing may also increase the aspirations reporting, because less then would be self-resolved by patients. Another approach could be initial post procedure chest X-rays as 2 reports did (21,22), this is however a slightly more expensive procedure and would require the patients to be in the hospital, which limits the outpatient capsule delivery. Only 5 papers reported the position in which the patient swallowed the capsule. Attention should be drawn to positioning the patient correctly in an upright position when administering capsules to this particular group. To ensure early detection and appropriate management of potential aspirations, it is crucial for a clinician or other trained personnel to monitor the ingestion process closely.
This systematic review aims to provide an updated and comprehensive analysis of published evidence concerning capsule aspiration. Among the 63 cases included in this review, 45 originated from case reports or series. It is important to acknowledge that not all instances of capsule aspiration are reported or published, and our search may have missed some cases due to language and accessibility limitations., which could introduce a potential bias in the selection process and contribute to an underestimation of the true incidence. Additionally, only 12 observational studies reported aspiration as one of their complications or outcomes, suggesting a possible underreporting and missing data on this event. However, despite the retrospective nature of case reports without statistical calculations, the included articles have been deemed suitable for the purpose of this review, indicating their adequacy in terms of quality. While the possibility of undetected or unreported cases is recognized, this systematic review represents the most up-to-date and comprehensive collection of relevant information, allowing for a more accurate estimation of capsule aspiration rates.
Aspiration of video capsules is an uncommon event that is scarcely reported on. One of the first reviews since the introduction of SBCE reported that in 22,840 procedures only 1.4% were retained, but no aspirated capsules were mentioned (67). A more recent review investigated the last two decades of distributed CE and reported that in 86,930 procedures only 2% experienced retention, but once again aspiration was not reported (3). However, another recent review does report on aspiration, with a pooled rate of aspiration as 0.00% (68). They found 5/23,449 aspiration cases, all occurring in SB investigations. They point out the risk of elderly age, but also that the rate of retention and SB incomplete examinations has declined over the years (68). In 2017, one review accumulated the data on aspiration of CE and found 37 individual cases (5). They conclude that aspiration is a rare event and safely managed, but the administration should be approached with precautions in certain patient groups. They find 94.6% male predominance and mean age of 78.9±7.81 years (range, 64–93) (5), which correlates well with this review. The fact that with this comprehensive review, only additional 26 cases have been reported in the last 5 years, it is clearer that capsule aspiration is a very rare event.
Conclusions
This systematic review provides an updated and comprehensive analysis of published evidence on capsule aspiration, contributing to the current understanding of this complication. While acknowledging the potential for undetected or unreported cases, this review represents the most recent and extensive collection of relevant information, facilitating a more accurate estimation of capsule aspiration rates. In conclusion, based on the reported literature, capsule aspiration remains a rare adverse event that can be safely managed. It should not discourage patients from undergoing the procedure. However, it is important to anticipate the possibility of aspiration in specific patient groups, and cautious measures should be taken when administering capsules.
Acknowledgments
The authors would like to acknowledge the European Society of Gastrointestinal Endoscopy (ESGE) for providing the opportunity to present an earlier version of this work as an abstract on the ESGE days 2023 conference.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-23-763/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-763/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-763/coif). A.K. serves as an unpaid editorial board member of Annals of Translational Medicine from October 2022 to September 2024. A.K. reports that he is a co-director and shareholder of AJM Medicaps, and iCERV Ltd.; and receiving consultancy fees (Jinshan Ltd. And DiagMed Healthcare Ltd.), travel support (Jinshan, DiagMed Healthcare Ltd.), research support (grant) from ESGE/Given Imaging Ltd. and (material) IntroMedic/SynMed, lecture honoraria (Jinshan, Medtronic). He participated in Advisory board meetings for Tillots, ANKON, Dr Falk Pharma UK. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hong SM, Jung SH, Baek DH. Diagnostic Yields and Clinical Impacts of Capsule Endoscopy. Diagnostics (Basel) 2021;11:1842. [Crossref] [PubMed]
- Deding U, Herp J, Havshoei AL, et al. Colon capsule endoscopy versus CT colonography after incomplete colonoscopy. Application of artificial intelligence algorithms to identify complete colonic investigations. United European Gastroenterol J 2020;8:782-9. [Crossref] [PubMed]
- Cortegoso Valdivia P, Skonieczna-Żydecka K, Elosua A, et al. Indications, Detection, Completion and Retention Rates of Capsule Endoscopy in Two Decades of Use: A Systematic Review and Meta-Analysis. Diagnostics (Basel) 2022;12:1105. [Crossref] [PubMed]
- Nakamura M, Kawashima H, Ishigami M, et al. Indications and Limitations Associated with the Patency Capsule Prior to Capsule Endoscopy. Intern Med 2022;61:5-13. [Crossref] [PubMed]
- Yung DE, Plevris JN, Koulaouzidis A. Short article: Aspiration of capsule endoscopes: a comprehensive review of the existing literature. Eur J Gastroenterol Hepatol 2017;29:428-34. [Crossref] [PubMed]
- Schneider AR, Hoepffner N, Rösch W, et al. Aspiration of an M2A capsule. Endoscopy 2003;35:713. [Crossref] [PubMed]
- Tabib S, Fuller C, Daniels J, et al. Asymptomatic aspiration of a capsule endoscope. Gastrointest Endosc 2004;60:845-8. [Crossref] [PubMed]
- Sinn I, Neef B, Andus T. Aspiration of a capsule endoscope. Gastrointest Endosc 2004;59:926-7. [Crossref] [PubMed]
- Buchkremer F, Herrmann T, Stremmel W. Mild respiratory distress after wireless capsule endoscopy. Gut 2004;53:472. [Crossref] [PubMed]
- Sepehr A, Albers GC, Armstrong WB. Aspiration of a capsule endoscope and description of a unique retrieval technique. Otolaryngol Head Neck Surg 2007;137:965-6. [Crossref] [PubMed]
- Nathan SR, Biernat L. Aspiration--an important complication of small-bowel video capsule endoscopy. Endoscopy 2007;39:E343. [Crossref] [PubMed]
- Shiff AD, Leighton JA, Heigh RI. Pulmonary aspiration of a capsule endoscope. Am J Gastroenterol 2007;102:215-6.
- Guy T, Jouneau S, D'Halluin PN, et al. Asymptomatic bronchial aspiration of a video capsule. Interact Cardiovasc Thorac Surg 2009;8:568-70. [Crossref] [PubMed]
- Leeds JS, Chew TS, Sidhu R, et al. Asymptomatic bronchial aspiration and retention of a capsule endoscope. Gastrointest Endosc 2009;69:561-2. [Crossref] [PubMed]
- Koulaouzidis A, Pendlebury J, Douglas S, et al. Aspiration of video capsule: rare but potentially life-threatening complication to include in your consent form. Am J Gastroenterol 2009;104:1602-3. [Crossref] [PubMed]
- Bredenoord AJ, Stolk MF, Al-toma A. Unintentional video capsule bronchoscopy. Eur J Gastroenterol Hepatol 2009;21:593. [Crossref] [PubMed]
- Jindal R CH.. An Incidental Capsule Bronchoscopy. Am J Gastroenterol 2009;104:S368.
- Fan ZQ, Lei W, Zhao XY. A case of accidental aspiration of a video capsule endoscope. Acta Acad Med Mil Tertiae 2009;31:289-93.
- Hill E, Vidyarthi G, Boyd W. Video Capsule Endoscopy: A Novel Complication: 1012. Am J Gastroenterol 2009;104:S371.
- Kurtz LE, Devito B, Sultan K. Electronic image of the month. Small bowel video capsule aspiration with bronchoscopic-assisted extraction. Clin Gastroenterol Hepatol 2010;8:e37-8. [Crossref] [PubMed]
- Depriest K, Wahla AS, Blair R, et al. Capsule endoscopy removal through flexible bronchoscopy. Respiration 2010;79:421-4. [Crossref] [PubMed]
- Choi HS, Kim JO, Kim HG, et al. A case of asymptomatic aspiration of a capsule endoscope with a successful resolution. Gut Liver 2010;4:114-6. [Crossref] [PubMed]
- Pezzoli A, Fusetti N, Carella A, et al. Asymptomatic bronchial aspiration and prolonged retention of a capsule endoscope: a case report. J Med Case Rep 2011;5:341. [Crossref] [PubMed]
- Lucendo AJ, González-Castillo S, Fernández-Fuente M, et al. Tracheal aspiration of a capsule endoscope: a new case report and literature compilation of an increasingly reported complication. Dig Dis Sci 2011;56:2758-62. [Crossref] [PubMed]
- Shafi M, Shafi A. A case of wireless small bowel capsule presenting as pulmonary foreign body. Am J Gastroenterol 2011;2:S389.
- Lu XD DH, Zhang ZG. Case of a video capsule endoscope which was accidentally aspirated and successfully coughed out. Chin J Dig Endosc 2011;28:709-10.
- Girdhar A, Usman F, Bajwa A. Aspiration of capsule endoscope and successful bronchoscopic extraction. J Bronchology Interv Pulmonol 2012;19:328-31. [Crossref] [PubMed]
- Parker C, Davison C, Panter S. Tracheal aspiration of a capsule endoscope: not always a benign event. Dig Dis Sci 2012;57:1727-8. [Crossref] [PubMed]
- Yarlagadda R, Poudel A, Lingutla D, et al. Bronchial Aspiration of a Video Capsule: A Rare Complication: 1380. Am J Gastroenterol 2012;107:S549.
- Despott EJ, O'Rourke A, Anikin V, et al. Tracheal aspiration of capsule endoscopes: detection, management, and susceptibility. Dig Dis Sci 2012;57:1973-4. [Crossref] [PubMed]
- Singh RA, Pai KR, Satur CM. Delayed presentation of an aspirated capsule endoscope. J Surg Case Rep 2013;2013:rjt082. [Crossref] [PubMed]
- Sánchez-Chávez X, Martínez-García CL. Capsule endoscope aspiration: a common complication?. Rev Gastroenterol Mex 2013;78:257-8. [Crossref] [PubMed]
- Pereira B, Santos A, Leitão C, et al. Aspiration of capsule endoscope. Rev Esp Enferm Dig 2013;105:438-9. [Crossref] [PubMed]
- Hall JJ, Fischer UM, Shah SK, et al. Video endoscope removal from the right main bronchus using a flexible esophagogastroduodenoscope. Am Surg 2013;79:E185-6.
- Ding NS, Hair C, De Cruz P, et al. Education and Imaging. Gastrointestinal: symptomatic bronchial aspiration of capsule endoscope - a significant complication. J Gastroenterol Hepatol 2013;28:761. [Crossref] [PubMed]
- Hussan H, Paradowski TJ, Prather CM. Unexpected Capsule Endoscopy Images Reveal Aspiration. ACG Case Rep J 2014;1:69. [Crossref] [PubMed]
- Elmunzer J, May K, Assistant M, et al. Bronchial Aspiration of a Video Capsule Endoscope: Report of a Case: 405. Am J Gastroenterol 2014;109:S122.
- Mannami T, Ikeda G, Seno S, et al. Capsule Endoscope Aspiration after Repeated Attempts for Ingesting a Patency Capsule. Case Rep Gastroenterol 2015;9:347-52. [Crossref] [PubMed]
- Magalhães-Costa P, Bispo M, Chagas C. Aspiration of Capsule Endoscopy. GE Port J Gastroenterol 2015;22:178-9. [Crossref] [PubMed]
- Amarna M, Vanlandingham A, Brahmbhatt P, et al. Late presentation of capsule endoscope aspiration with successful extraction by flexible bronchoscopy utilizing a snare wire loop. Endoscopy 2015;47 Suppl 1 UCTN:E6-7.
- Choi YX HT, Ma Y, Liang BS. A case of accidental aspiration of a video capsule endoscope. Chin J Gastrointest Endosc 2015;2:141-2.
- Juanmartiñena Fernández JF, Fernández-Urien I, Vila Costas JJ. Asymptomatic bronchial aspiration of capsule endoscope: a significant complication. Rev Esp Enferm Dig 2016;108:605. [Crossref] [PubMed]
- Juanmartiñena Fernández JF, Fernández-Urién Sainz I, Zabalza Ollo B, et al. Transient tracheo-bronquial aspiration of capsule endoscope. Acta Gastroenterol Belg 2017;80:441.
- Buscot M, Leroy S, Pradelli J, et al. Bronchial Aspiration of Capsule Endoscope. Respiration 2017;93:122-5. [Crossref] [PubMed]
- Ribaldone DG, Bruno M, Solidoro P, et al. Real time visualization may be advisable to exclude aspiration in patients undergoing capsule endoscopy examination. Rev Esp Enferm Dig 2017;109:878-9. [Crossref] [PubMed]
- Skouras T, Sawbridge D, Steel A, et al. Aspiration of a small bowel video capsule: a rare complication. BMJ Case Rep 2018;2018:bcr2018224538. [Crossref] [PubMed]
- Keil-Ríos D, Angulo-Molina D, Farca-Belsaguy A. Ten-hour asymptomatic bronchoaspiration of a capsule endoscopy camera. Rev Gastroenterol Mex (Engl Ed) 2018;83:451-2. [Crossref] [PubMed]
- Arroyo-Mercado FM, Martinez M. Asymptomatic Tracheal Aspiration of Capsule Endoscopy in a Patient Without Dysphagia. ACG Case Rep J 2019;6:e00237. [Crossref] [PubMed]
- Dan T, Dandan S, Enqiang L. Aspiration of a Magnetically Controlled Capsule Endoscopy. Gastroenterology 2023;164:e30-1. [Crossref] [PubMed]
- Hilewitz A, Agrawal A, Lakticova V. Capsule bronchoscopy: a pill endoscopy gone wrong. Chest 2019;156:A55.
- Rutazaana D, Nawaz A. 1899 Bronchial Aspiration of Capsule Endoscopy: A Rare but Potentially Fatal Complication. Am J Gastroenterol 2019;114:S1062-S3.
- Takeda K, Tashimo H, Miyakawa K, et al. Patency Capsule Aspiration. Intern Med 2020;59:1071-3. [Crossref] [PubMed]
- Egger KM, Tse CS, Rupawala A. S2019 Successful Endoscopic Management of a Video Capsule Retained in the Pharynx. Am J Gastroenterol 2021;116:S877-S8.
- Tamang S, Mitnovetski S. Capsule endoscopy in airway: a difficult extraction. J Surg Case Rep 2022;2022:rjac385. [Crossref] [PubMed]
- Gaisinskaya P, Yoshinaga K, Hernandez OL. Necessity of Swallow Evaluations in the Elderly Prior to Capsule Endoscopy. Cureus 2022;14:e24138. [Crossref] [PubMed]
- Gomez P, Arce V, Zucker K, et al. S2669 Video Capsule Bronchoscopy: A Rare Complication of Video Capsule Endoscopy. Am J Gastroenterol 2022;117:e1762.
- Rondonotti E, Herrerias JM, Pennazio M, et al. Complications, limitations, and failures of capsule endoscopy: a review of 733 cases. Gastrointest Endosc 2005;62:712-6; quiz 752, 754.
- Girelli CM, Maiero S, Porta P, et al. Small bowel capsule endoscopy performance in octogenarians: a case-control study. J Gerontol A Biol Sci Med Sci 2011;66:68-73. [Crossref] [PubMed]
- Li Y, Wang L, Fan C, et al. Diagnostic value of OMOM capsule endoscopy in 159 patients with unexplained abdominal pain. J Third Mil Med Univ 2012;34:254-6.
- Soncini M, Rondonotti E, Girelli CM, et al. Small bowel capsule endoscopy (SBCE) complications: frequency, management and policy to prevent them. Prospective data from a regional registry (Registro Lombardo Delle Complianze). Dig Liver Dis 2013;45:S135-6.
- Pezzoli A, Guarino M, Fusetti N, et al. Efficacy and safety of capsule endoscopy in octogenarian patients: a retrospective study. Minerva Gastroenterol (Torino) 2023;69:388-95. [Crossref] [PubMed]
- Fernández-Urién I, Carretero C, González B, et al. Incidence, clinical outcomes, and therapeutic approaches of capsule endoscopy-related adverse events in a large study population. Rev Esp Enferm Dig 2015;107:745-52. [Crossref] [PubMed]
- Kim SH, Kim JW. Small Bowel Malignancies in Patients Undergoing Capsule Endoscopy for Iron Deficiency Anemia. Diagnostics (Basel) 2021;12:91. [Crossref] [PubMed]
- Freitas M, Macedo Silva V, Xavier S, et al. Prolonged Gastric Transit Time in Small-Bowel Capsule Endoscopy: Which Patients Are at Risk and What Are the Implications? Turk J Gastroenterol 2023;34:227-33. [Crossref] [PubMed]
- Shiotani A, Honda K, Kawakami M, et al. Use of an external real-time image viewer coupled with prespecified actions enhanced the complete examinations for capsule endoscopy. J Gastroenterol Hepatol 2011;26:1270-4. [Crossref] [PubMed]
- Rondonotti E, Spada C, Adler S, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy 2018;50:423-46. [Crossref] [PubMed]
- Liao Z, Gao R, Xu C, et al. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc 2010;71:280-6. [Crossref] [PubMed]
- Wang YC, Pan J, Liu YW, et al. Adverse events of video capsule endoscopy over the past two decades: a systematic review and proportion meta-analysis. BMC Gastroenterol 2020;20:364. [Crossref] [PubMed]