Revisiting the reconstructive ladder for soft tissue reconstruction in the lower extremity
Introduction
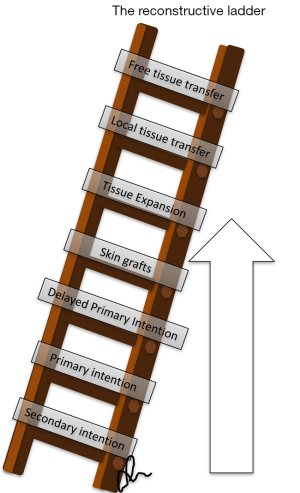
The reconstructive ladder (Figure 1) was borne on the principle of presenting a simple and stepwise algorithm where the simplest method for achieving tension-free closure was utilized (1). Nowhere was this paradigm more evident than lower limb reconstruction. The traditional priorities of reconstruction after composite tissue loss from trauma, tumour or infection were: provide immediate stability, preserve length for a stable gait, and ensure early soft tissue coverage of exposed bone, joints, and implants. In the upper limb, reconstruction is directed towards restoration of function and the aesthetic appearance is an important consideration given its relative visibility. In contrast, reconstruction for the lower limb is typically directed towards coverage. Here, restoration of function implicates coverage of implants and critical structures to enable the orthopedic goals of early weight bearing and range of motion to occur, rather than the restoration of individual small joint and tendon function. Consequently, reconstructive surgeons frequently trade the mobility of individual joints, such as the ankle or toes, for a simpler reconstructive procedure. Such trade-offs include excision of exposed tendons, and transposition of important muscles (such as the tibialis anterior) to cover exposed bone. Prolonging negative-pressure dressings that inevitably obliterate the adipofascial gliding planes is also better tolerated in the lower limb. Given the concealed nature of the lower limb, aesthetic appearance has a much lower priority.
Evolving paradigms in lower limb reconstruction
A few factors have changed the way modern reconstructive surgeons perceive lower limb reconstruction. First, the advances in our understanding of clinical and anatomical vascular territories and tissue perfusion (2) have led to the description of numerous pedicled and free perforator-based flaps (3) that were not in our traditional armamentarium. Concurrent leaps in microsurgical technology, instrumentation and training have made microvascular surgery routine in many parts of the world and most reconstructive surgeons are very comfortable with free tissue transfer (4). The second phenomenon is the shift from objective, physician-reported outcomes to patient-reported outcomes (PROMs). Wound coverage and painless ambulation is no longer the only goal of limb salvage, and functional restoration must consider the various domains of the patient’s life (activities of daily living, work, and recreational pursuits), individual preferences, aesthetics, and costs. The third reason for a change in perspective is the abundance of orthopedic implants and techniques in skeletal reconstruction. Specifically contoured implants, antibiotic-impregnated cement and synthetic bone grafts confer immediate stability in the setting of significant bone loss but demand durable soft tissue cover immediately. In contrast, significant initial limb shortening can be accepted because multi-planar external frames can be used to subsequently lengthen the limb and concomitantly correct deformity. However, subsequent re-elevation of the reconstructed soft tissue is often necessary for staged operations such as bone grafting and internal fixation.
The reconstructive elevator
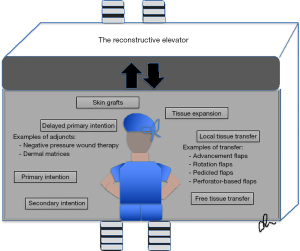
The notion that “simplest may not be best” is not new. Gottlieb and Krieger introduced the “reconstructive elevator” (Figure 2), which highlighted the need to be flexible and innovative to produce better functional and aesthetic outcomes that meet the patient’s individual expectations and functional demands (5). These concepts are widely applied in head and neck, trunk, and upper limb reconstruction, and it is only natural that the lower limb should follow this paradigm shift. We must be cognizant, however, that the metaphorical elevator moves in both directions. Technological and scientific advances have not only enabled us to perform increasingly complex operations. Other advances have also ensured that “simple” treatments are no longer inferior. These include important adjuncts such as negative pressure wound therapy, dermal matrices, and tissue expansion, which were included in the “New Reconstructive Ladder” (6) which sought to incorporate greater surgical options in a similar step-ladder manner with more rungs to the traditional ladder in keeping with modern surgical advances. The elevator differs slightly in that surgical options of similar complexity are presented at the same “level” (Figure 2). Consequently, the modern reconstructive surgeon is faced with a unique dilemma created by an excess of reconstructive options in the toolbox: “What do I choose when I have all the options at my disposal?”.
The subsequent sections discuss specific considerations that affect decision-making in lower limb reconstruction and highlight situations where the reconstructive approach may need to deviate from the traditional step-wise approach.
Anatomic considerations
Tapered shape of the limb
The upper and lower limbs have a tapering design, with progressively decreasing girth and relative quantity of soft tissue from proximal to distal. There is ample skin and muscle in the thigh, whereas the distal tibia is enveloped by a narrow sleeve of soft tissue and lacks significant muscle bulk. This has implications on the availability of local tissue for coverage. A limb with abnormal or abrupt contours is also less acceptable from an aesthetic perspective.
Mobile skin over joints
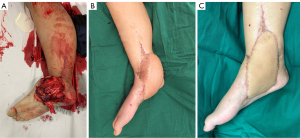
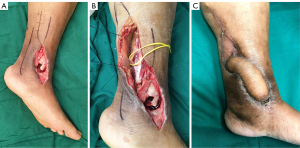
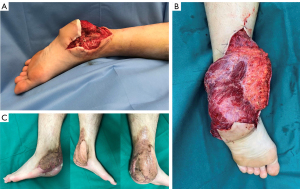
The skin over the joints requires a great deal of mobility. The distal leg and ankle were traditionally recognized as “free flap territory” but the increasing proficiency with free tissue transfer does not mean that these procedures are without problems. The operations are lengthy, require significant manpower and physical resources in the peri-operative period, and often require multiple subsequent procedures (Figure 3). Perforator-based flaps have become a game-changer for resurfacing soft tissue defects around the knee and ankle. Amarante et al. described the posterior tibial artery perforator flap with a narrow pedicle and long arc of rotation allowing versatility of coverage as early as 1986 where perforator dissection revealed relatively constant and predictable anatomy (7,8). Perforator flaps can be performed quickly and limit the potential donor site issues to the same limb. In addition, they provide better tissue match in terms of colour, texture, and contour (9). In their anatomical study, Morris et al. proposed the lower limb as being the largest donor site for perforator flap harvest, with an average of 93 perforators from 21 vascular territories (10). For small to medium size defects up to 50 cm2 in the leg, local perforator-based transposition or propeller flaps have significant utility (11). Figure 4 illustrates the role of perforator flaps in lower limb reconstruction, and the benefits over free tissue transfer.
Dorsum of the foot
The dorsal surface of the foot comprises thin, pliable hair-bearing skin that permits gliding of the digital extensor tendons. Very thin free flaps, such as the radial forearm flap, may be used to resurface dorsal foot defects with good functional and aesthetic outcomes but may incur significant donor site morbidity (Figure 5). In situations where the critical defect involves only tendons without exposure of the joints or implants, we prefer to apply a dermal matrix followed by an unmeshed split-thickness skin graft (Figure 6). This is a situation where intentionally “moving down” the reconstructive elevator achieves comparable results without the problems of a more complex procedure.


Plantar surface
The plantar surface has thick glabrous skin that is designed for weight bearing. Fat lobules and pads (12) help load redistribution, and protective sensation is provided by the plantar nerves (13). Glabrous skin is limited in supply because the only other site where it may be found is the palmar surface of the hand or the other foot. The heel and plantar surfaces of the foot are some of the most challenging areas to reconstruct due to the constant compressive and shear forces. Consequently, even the best reconstructive effort can never recreate the unique properties of this region. In a recent systematic review, Crowe et al. surmised that there was a lack of consensus on the best reconstructive modality for the plantar foot defect (14).
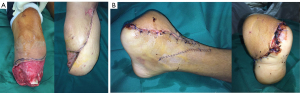
A reconstructive algorithm including the defect location, size and depth (supra-versus sub fascial), the need for sensate coverage, and surgeon preference/comfort should guide reconstruction (15). Our preferred skin flaps include the reverse sural artery flap and free fasciocutaneous flaps such as the anterolateral thigh (ALT), medial sural artery perforator (MSAP), radial forearm and lateral arm flaps. Skin flaps provide a better aesthetic result and are more resistant to shear, but they are difficult to contour. The heel region requires that the flap be contoured around the curve of the calcaneus in both the medio-lateral and proximal-distal axes. Consequently, even the thinnest flap will produce a bulky reconstruction that can make stable weight-bearing an issue (Figure 7). Muscle flaps, such as the free latissimus dorsi flap, are easier to contour but the issues with these flaps include shear and a bulky unsightly appearance (Figure 8). One must also consider that many of these defects are complex with possible foreign materials and plates underlying the reconstruction for bony fixation and stability. As such, propeller flaps, with their potential risk of venous congestion and secondary healing may be avoided and a free flap given higher priority in this context (16).

Plantar arch
From a biomechanical perspective, restoration of the arches of the foot for stable weight bearing and ambulation is the priority of the orthopedic surgeon (17). Deformity or an imbalance of the static and dynamic stabilizers of the foot would predispose to uneven contact pressures, callosities, and eventual skin breakdown. It is important to work with the orthopedic team to anticipate and circumvent this in the joint operative plan.
Injury considerations
Size of defect
It is important to remember that a hemi-gastrocnemius or hemi-soleus flap is only large enough to cover an area equivalent to the width of the subcutaneous border of the tibia, and larger defects frequently require alternative methods of reconstruction. Random pattern fasciocutaneous flaps, perforator-based propeller flaps and keystone flaps are useful in small to medium sized defects, provide better tissue match and associated with a lower donor site morbidity (9). Large defects typically require free tissue transfer but tissue expansion may be employed in more elective settings, such as excision of benign cutaneous masses and congenital malformations.
Location of defect
The leg has thus been traditionally divided into thirds based on the most feasible method of soft tissue coverage—the proximal third (gastrocnemius flap), the middle third (soleus flap) and the distal third (free flaps) (4). However, small- to medium-sized defects in the distal leg can be successfully resurfaced with perforator-based flaps when the zone of injury is small.
Zone of injury
A larger zone of injury may necessitate a longer bridge segment for pedicled flaps or free flaps with longer pedicles, such as the ALT and MSAP flaps.
Loss of functional units
Besides skin and soft tissue, additional components may need to be replaced (8), and this is often the premise of composite tissue transfer (18). The ALT flap has proven to be versatile in this respect with the concomitant harvest of the fascia lata, which can be folded and used to reconstruct tendinous structures (19). The fascia lata can be also harvested in isolation and used for composite reconstruction of the Achilles tendon defect, with a turndown gastrocnemius facial flap which is less bulky (20). Another example is the use of a free functional gracilis transfer for restoration of foot dorsiflexion in a highly functional patient who has lost muscles in the anterior compartment of the leg (21). In cases where a skin graft is chosen, grafting over tendon can be precarious even when there is a matrix as a buffer. Placement of a negative pressure wound therapy device over the graft can significantly improve graft take with the application of a uniform pressure (22) and we typically use this at a low pressure for approximately 5–7 days to prevent shear even as some patients start mobilizing with a portable device.
Other considerations
Amputation stump
Traumatic lower limb amputations typically involve a great degree of force and a wide zone of injury. This often leaves very little skin and muscle available to resurface the amputation stump. There is a temptation to shorten the part further to achieve coverage with adjacent tissue because it is a simpler option, but this may leave the stump too short and functionless. In this situation, performing an immediate or early free tissue transfer provides abundant well-padded tissue that is resistant to shear, and is a much better option than using skin grafts and precarious adjacent muscle as flaps that will eventually break down and prevent a good fit for a prosthesis (Figure 9).
Need for secondary procedures
There are a variety of secondary orthopedic and soft tissue procedures that are necessary after initial limb salvage. These include bone grafting, corrective osteotomy, internal fixation, selective joint arthrodesis, and procedures for re-animation such as nerve, tendon, and free functional muscle transfers. Even though muscle flaps, such as a hemisoleus flap, provide good soft tissue cover, they are not as easy to elevate as fasciocutaneous flaps because they tend to become adherent. It is important to establish a clear treatment plan with the orthopedic team and anticipate any secondary procedures. Where knee arthroplasties have become extremely common operations, one does have to deal with the occasional infected arthroplasty. Sapino et al. found the pedicled chimeric gastrocnemius MSAP flaps safer to re-raise compared to gastrocnemius muscle flaps as the skin paddle scarred more reliably and did not incur shrinkage (23). Our preference is also to use local, regional, or free fasciocutaneous flaps when staged operations are necessary, and the specific choice depends on the size of the defect and required pedicle length (Figure 10). Some of these options, such as perforator-based flaps and free tissue transfer, are more time- and resource-intensive compared to a local muscle flap but this highlights the importance of flexibility when faced with a specific situation.

Aesthetic and patient driven factors
The final cosmetic outcome after reconstruction is paramount, particularly for children and young patients. Local random pattern and perforator-based flaps provide good tissue match and minimize the additional donor site morbidity that free flaps involve. As discussed above, perforator-based propeller flaps combine the advantages of local flaps with good tissue match and contour while providing tissue away from the zone of injury. Yet the flap design entails considerable dissection and lengthening of the defect (21). This additional incision may not be amenable to primary closure and can be unsightly. It is very important to present the whole range of options to patients, including photographs of prior reconstructive cases. The surgeon and patient may eventually choose more conservative options that avoid additional incisions, such as prolonged negative-pressure dressings, dermal matrices, and healing by secondary intention. A subgroup of patients may prefer this trade-off between prolonged wound healing and less extensive scars, provided the risks of infection are comparable.
There are additional patient-centric factors that are also very important. The patient profile we now deal with is increasingly complex. Oncological surgeries that were not possible before are now being performed due to better diagnostic modalities, neoadjuvant and adjuvant therapy. However, radiation, chemotherapy, and immunotherapy themselves pose unique challenges to wound healing. The surgeon may lean towards a robust workhorse flap to expedite wound healing so that adjuvant therapy may be initiated in a timely manner. Complications such as flap failure, wound breakdown, infection, and repeat coverage procedures inevitably delay definitive oncological treatment and ultimately compromise the overall prognosis. Chronic wounds in the elderly have been proposed as a “geriatric syndrome” and surgeons must account for the higher prevalence of chronic conditions that affect both flap survival and wound healing, such as cardiovascular disease, diabetes, poor nutrition, and impaired mobility (24). Diminished reserves and higher peri-operative risks implicate a poorer tolerance to long and complex procedures. The challenges to reconstruction in these patients should not be underestimated and even the most “reliable” flap is prone to failure in unfavorable recipient conditions. Simpler modalities may ultimately produce comparable outcomes and the surgeon must be prepared to take a step back and appreciate the situation in a holistic manner.
Footwear
An additional consideration in the foot is footwear. A foot that is too broad or bulky will make it difficult to find appropriate footwear and eventually predispose to pain and ulceration. In the distal foot where tissue pliability is also key in allowing a good toe-off phase of gait, V-Y advancements and local flaps based on the dorsalis pedis (25) and first dorsal metatarsal artery (26,27) may be utilized.
Conclusions
Reconstruction of soft tissue defects in the lower limb is clearly not a “one size fits all” approach. Careful staging of complex reconstructive procedures, judicious selection of microsurgery and wound care adjuncts, and using biology to our advantage will ultimately result in better patient outcomes. While the reconstructive ladder serves as a conceptual guide to treatment, the actual decision-making process depends on multiple factors and the reconstructive surgeon must be able to expertly maneuver around the available options to achieve the desired objective.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Johnny Ionut Efanov) for the series “The Modern Plastic and Reconstructive Surgeon – Collaborator, Innovator, Leader” published in Annals of Translational Medicine. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1445/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1445/coif). The series “The Modern Plastic and Reconstructive Surgeon – Collaborator, Innovator, Leader” was commissioned by the editorial office, Annals of Translational Medicine without any sponsorship or funding. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from patients for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Simman R. Wound closure and the reconstructive ladder in plastic surgery. J Am Col Certif Wound Spec 2009;1:6-11. [Crossref] [PubMed]
- Taylor GI, Corlett RJ, Dhar SC, et al. The anatomical (angiosome) and clinical territories of cutaneous perforating arteries: development of the concept and designing safe flaps. Plast Reconstr Surg 2011;127:1447-59. [Crossref] [PubMed]
- Saint-Cyr M, Wong C, Schaverien M, et al. The perforasome theory: vascular anatomy and clinical implications. Plast Reconstr Surg 2009;124:1529-44. [Crossref] [PubMed]
- Pu LL. A Comprehensive Approach to Lower Extremity Free-tissue Transfer. Plast Reconstr Surg Glob Open 2017;5:e1228. [Crossref] [PubMed]
- Gottlieb LJ, Krieger LM. From the reconstructive ladder to the reconstructive elevator. Plast Reconstr Surg 1994;93:1503-4. [Crossref] [PubMed]
- Janis JE, Kwon RK, Attinger CE. The new reconstructive ladder: modifications to the traditional model. Plast Reconstr Surg 2011;127:205S-12S. [Crossref] [PubMed]
- Jones EB, Cronwright K, Lalbahadur A. Anatomical studies and five years clinical experience with the distally based medial fasciocutaneous flap of the lower leg. Br J Plast Surg 1993;46:639-43. [Crossref] [PubMed]
- Amarante J, Costa H, Reis J, et al. A new distally based fasciocutaneous flap of the leg. Br J Plast Surg 1986;39:338-40. [Crossref] [PubMed]
- AlMugaren FM, Pak CJ, Suh HP, et al. Best Local Flaps for Lower Extremity Reconstruction. Plast Reconstr Surg Glob Open 2020;8:e2774. [Crossref] [PubMed]
- Morris SF, Tang M, Almutari K, et al. The anatomic basis of perforator flaps. Clin Plast Surg 2010;37:553-70. xi. [Crossref] [PubMed]
- Bajantri B, Bharathi RR, Sabapathy SR. Wound coverage considerations for defects of the lower third of the leg. Indian J Plast Surg 2012;45:283-90. [Crossref] [PubMed]
- Cavanagh PR. Plantar soft tissue thickness during ground contact in walking. J Biomech 1999;32:623-8. [Crossref] [PubMed]
- Robbins S, Gouw GJ, McClaran J, et al. Protective sensation of the plantar aspect of the foot. Foot Ankle 1993;14:347-52. [Crossref] [PubMed]
- Crowe CS, Cho DY, Kneib CJ, et al. Strategies for Reconstruction of the Plantar Surface of the Foot: A Systematic Review of the Literature. Plast Reconstr Surg 2019;143:1223-44. [Crossref] [PubMed]
- Low OW, Sebastin SJ, Cheah AEJ. A Review of Pedicled Perforator Flaps for Reconstruction of the Soft Tissue Defects of the Leg and Foot. Indian J Plast Surg 2019;52:26-36. [Crossref] [PubMed]
- Guillier D, Sapino G, Schaffer C, et al. Lower limb reconstruction involving osteosynthesis material: A retrospective study on propeller flaps outcomes. Injury 2021;52:3117-23. [Crossref] [PubMed]
- Donatelli RA. Abnormal biomechanics of the foot and ankle. J Orthop Sports Phys Ther 1987;9:11-6. [Crossref] [PubMed]
- Heller L, Levin LS. Lower extremity microsurgical reconstruction. Plast Reconstr Surg 2001;108:1029-41; quiz 1042. [Crossref] [PubMed]
- di Summa PG, Sapino G, Cherubino M, et al. Reconstruction of complex soft tissue defects including tendons with anterolateral thigh flap extended to fascia lata: Long term recovery and functional outcomes. Microsurgery 2019;39:405-15. [Crossref] [PubMed]
- Maruccia M, Tedeschi P, Caizzi G, et al. Graft and flap. A novel orthoplastic approach to achilles tendon secondary rupture. Plast Reconstr Surg 2023;152:1359-64. [Crossref] [PubMed]
- Pederson WC, Grome L. Microsurgical Reconstruction of the Lower Extremity. Semin Plast Surg 2019;33:54-8. [Crossref] [PubMed]
- Sapino G, Lanz L, Roesti A, et al. One-Stage Coverage of Leg Region Defects with STSG Combined with VAC Dressing Improves Early Patient Mobilisation and Graft Take: A Comparative Study. J Clin Med 2022;11:3305. [Crossref] [PubMed]
- Sapino G, Guiller D, Osinga R, et al. Muscle-only versus chimeric musculocutaneous gastrocnemius pedicled flap in complex orthoplastic reconstructions of the knee region: A retrospective study. J Plast Reconstr Aesthet Surg 2023;77:298-308. [Crossref] [PubMed]
- Ono S, Sebastin SJ, Yazaki N, et al. Clinical applications of perforator-based propeller flaps in upper limb soft tissue reconstruction. J Hand Surg Am 2011;36:853-63. [Crossref] [PubMed]
- Alam W, Hasson J, Reed M. Clinical approach to chronic wound management in older adults. J Am Geriatr Soc 2021;69:2327-34. [Crossref] [PubMed]
- Koul AR, Patil RK, Philip VK. Coverage of defects over toes with distally based local flaps: A report of four cases. Indian J Plast Surg 2008;41:62-6. [Crossref] [PubMed]
- Hayashi A, Maruyama Y. Reverse first dorsal metatarsal artery flap for reconstruction of the distal foot. Ann Plast Surg 1993;31:117-22. [Crossref] [PubMed]