Early multifocal recurrence of hepatoblastoma in the residual liver after R0 liver resection with ALPPS procedure: a case report
Introduction
Complete resection for hepatoblastoma is the ultimate goal of treatment. Simple resection may not be possible due to extensive anatomical involvement or central location in liver. Conventionally these patients are candidates for liver transplant once chemotherapy has been completed. We are reporting our experience of a 14-month-old, who underwent associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) procedure for complete resection of extensive hepatoblastoma.
Case presentation
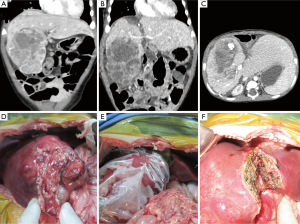
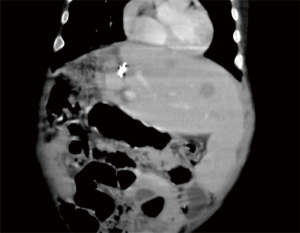
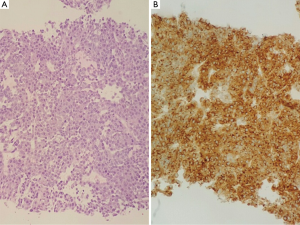
A 10-month-old boy presented with hepatoblastoma, tumour mass involving Couinaud’s segments 4, 5, 6 and 8, 7.2×8.5×11.1 cm3 (Figure 1A) and was staged as pretext III standard risk with tumour limited to the liver. A biopsy confirmed the diagnosis of hepatoblastoma. Segment 2 & 3 with stretched over left portal vein were being indented by the large tumour mass. Serum AFP was more than 30,000 IU/mL. After multidisciplinary team review, chemotherapy with single agent cisplatin 15.6 mg per dose (2.6 mg/kg/dose) was initiated. Reassessment CT scan after five cycles showed gross reduction in the size of tumour from 339 to 88 cm3. Tumour resection became possible by performing a right trisectionectomies segment 4, 5, 6 and 8 were still involved but segment 2 and 3 were clear of tumour. However future liver volume (FLV) measured only 90 mL. Total volume of liver parenchyma was 300 mL and child weighed 8.6 kg. There was significant risk of small for size syndrome and liver failure. Liver transplant was not an option for the parents as there is no local facility and traveling overseas was not a financially viable option for the parents. Considering this we offered parents with an alternative option of ALPPS procedure for a right trisectionectomy. After appropriate consent from parents and ethical considerations, ALPPS procedure was carried out. During 1st stage, right portal vein ligation (PVL) and splitting of liver at falciform ligament was carried out (Figure 1B-F). An extension of the tumour to segment 3 was also included in the resected part. A 1 cm strip of liver parenchyma at the resection margin was sent for frozen section, which confirmed clear margins. The resected part of the liver was packed in a sterile plastic bag (Figure 1E) and abdomen closed. Initial postoperative course was quite eventful with respiratory infection requiring prolonged ICU stay for four days. At day 10 a CT scan was performed to assess hypertrophy of FLV. There was significant hypertrophy of segment 1, 2 and 3 and segment 2 & 3 were measured as 210 mL (an increase of 61%). At day 14 completion phase of procedure was performed by ligating and dividing right hepatic artery, right hepatic duct, right and middle hepatic veins. Peroperative cholangiogram confirmed intact and patent left hepatic duct. Liver parenchymal resection was completed. After second stage, he remained stable and recovered quickly without requiring assisted ventilation. There was transient hyperbilirubinemia up to 8.7 g/dL, which returned to normal within 3 days. He was discharged from hospital on day 19 from first admission. Histopathology confirmed hepatoblastoma, mixed epithelial and mesenchymal type without teratoid feature, with clear resection margins and no evidence of microvascular invasion or intrahepatic micrometastasis. Serum AFP was recorded on 4th and 15th post-operative day as 14,778 and 7,869 IU/mL (preoperative value was more than 30,000 IU/mL). He received last cycle of cisplatin from 16th post-operative day and underwent end of treatment CT imaging on 30th post-operative day. There was gross hypertrophy of residual liver pushing the spleen and left colon down towards pelvis. However a new finding was the development of five hypodense lesions studded in segment 2 and 3, largest being 17×11 mm2 in size, well away from falciform ligament and resection margin (Figure 2). Trucut biopsy confirmed presence of infiltrative hepatoblastoma (Figure 3). Serum AFP shot up again to more than 30,000 IU/mL. At this stage further chemotherapy with doxorubicin and cisplatin was planned. However he developed progressive jaundice and ascites. At this point it was decided to do only palliation and parents opted to do it at home.
Discussion
Ligation of portal vein in association with parenchymal partition was first described by Dr. Hans Schlitt in 2007, discovered accidentally (1). Later in 2012, Schnitzbauer et al. reported application of this procedure in a landmark paper, in 25 patients (2). Procedure was not named until de Santibañes and Clavien proposed the name “ALPPS” in an editorial (3). Main objective of this procedure is to achieve rapid hypertrophy of FLV to avoid liver insufficiency. There is evidence that in comparison with the previous practice of preoperative portal vein embolisation (PVE) or PVL alone, ALPPS provides a stronger stimulus for hypertrophy to future liver (4). Hypertrophy being driven by both vascular and humoral factors, PVL and in situ split of liver leads to stimulate both. Previous studies have documented up to 61% to 80% increase in size between two stages of surgery (4). There are only two reports of application of this procedure in children, youngest being 3 years (5). Although the procedure was technically successful in our patient evidenced by rapid regeneration of liver and progressive drop in serum AFP levels for 3 weeks consecutively after resection of hepatoblastoma, the final outcome was marred by a very early, multifocal recurrence in an uninvolved site. The histopathology report ruled out microvascular invasion and presence of pre-existing micrometastasis in liver parenchyma. This outcome left us with very important questions; should we offer ALPPS again in similar situation? It is difficult to assess if ALPPS procedure itself played role in early recurrence by virtue of a strong stimulus for liver to grow? There are previous reports of recurrence of tumour after ALPPS (6) in adults. It is difficult to conclude from our experience if one should avoid performing ALPPS in a situation like our child or take it as a chance occurrence and be more aggressive in reinstitution of chemotherapy after tumour has been resected using ALPPS procedure.
Conclusions
We conclude that although technically it may be feasible to perform ALPPS procedure even in 1 year old patient but we still need further studies to assess the oncological outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Bertens KA, Hawel J, Lung K, et al. ALPPS: challenging the concept of unresectability--a systematic review. Int J Surg 2015;13:280-7. [Crossref] [PubMed]
- Schnitzbauer AA, Lang SA, Goessmann H, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 2012;255:405-14. [Crossref] [PubMed]
- de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the "ALPPS" approach. Ann Surg 2012;255:415-7. [Crossref] [PubMed]
- Schadde E, Ardiles V, Slankamenac K, et al. ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 2014;38:1510-9. [Crossref] [PubMed]
- Chan A, Chung PH, Poon RT. Little girl who conquered the "ALPPS''. World J Gastroenterol 2014;20:10208-11. [Crossref] [PubMed]
- Oldhafer KJ, Donati M, Jenner RM, et al. ALPPS for patients with colorectal liver metastases: effective liver hypertrophy, but early tumor recurrence. World J Surg 2014;38:1504-9. [Crossref] [PubMed]


