
Cardiac arrest due to an unexpected inability to ventilate in a tracheostomy patient suggesting the need for a routine anesthesia checklist and an anesthesia relevant emergency pathway for tracheostomy management: a case report
Highlight box
Key findings
• We present a cannot ventilate with cardiac arrest scenario despite following current tracheostomy guidelines.
• As underlying problem, we found a stone like mucus plug in a tracheostomy tube following a coronavirus disease 19 (COVID-19) infection.
What is known and what is new?
• It is known that up to 30% of patients worldwide have a significant complication related to their tracheostomy.
• What is new is that a mucus plug in a tracheostomy had turned into a stone following a COVID-19 infection.
What is the implication, and what should change now?
• We recommend establishing a routine checklist and anesthesia specific guideline for emergencies that follows every patient with a tracheostomy undergoing surgery.
Introduction
Background
Up to 30% of patients worldwide may have a significant complication related to their tracheostomy (1,2). A wide variety of tracheostomy tubes exist, and this can complicate airway management, particularly in an emergency. Common features include an inflatable cuff and an inner cannula, which can be removed (I) for cleaning to minimize risk of blockage, or (II) during an emergency (3). Tracheostomy complications include but are not limited to hemorrhage, aspiration, pneumothorax, blockage, tube displacement or tracheal stenosis. The Royal College of Anaesthetists 4th National Audit Project found that most tracheostomy-related critical incidents are related to displacement of the tracheostomy tube (4). Following the audit, the National Tracheostomy Safety Project developed guidelines to aid in the recognition and management of tracheostomy-related emergencies (5).
Rationale and knowledge gap
In this case report, we present an unexpected airway complication in a brain-injured patient with an established tracheostomy. We were unable to find any case reports in the literature describing a similar scenario, and we were also unable to find a previous report of a tracheostomy mucus plug crystallizing into an impassable stone. The only similar case report described a mucus plug that was distal to the tracheostomy tube, and prevented suctioning but still permitted passage of a suction catheter (6).
Objective
We will discuss the unusual underlying cause in relation to established guidelines, differentials, and treatment options for patients who present to the operating room (OR) with an existing tracheostomy tube. We present this case in accordance with the CARE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1834/rc).
Case presentation
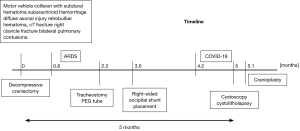
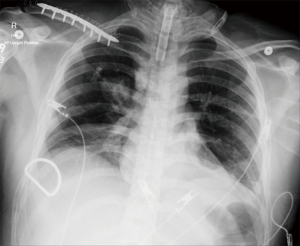
The patient was a young adult male with no comorbidities, 84 kg [body mass index (BMI) 23.9 kg/m2], who suffered a traumatic brain injury after a motor vehicle collision and ejection 5 months prior to this reported event (see Figure 1 for timeline of events). All care he received at that time was outside of our institution, and therefore the specifics of his hospitalization are based solely on the limited records we received after his transfer. The patient was thrown 40 feet from the vehicle, which resulted in extensive head trauma. He first had a decompressive craniectomy for his subdural and subarachnoid hematomas. In addition to his intracranial bleeds, he presented with diffuse axonal injury, retrobulbar hematoma, a C7 fracture, a right clavicular fracture and bilateral lung contusions. After his craniotomy, he underwent open reduction and internal fixation of the right clavicle, and lateral canthotomy to evacuate the retrobulbar hematoma. Later, he suffered from a methicillin-resistant staphylococcus aureus (MRSA) and klebsiella ventilator-associated pneumonia with acute respiratory distress syndrome shortly after admission. After his acute recovery, he remained ventilator dependent, and required surgical tracheostomy placement (see Figure 2 for X-ray). Following surgical tracheostomy without complications, the patient had a cuffed Shiley™ Flexible Adult Tracheostomy (Medtronic, Minneapolis, MN, USA) 7.5 mm I.D. (inner diameter) with disposable inner cannula. Complicating his course, he later developed communicating hydrocephalus for which he was then transferred to our institution a month later for a right-sided occipital shunt placement. Shortly after his surgery, he developed another pneumonia. This time it was a methicillin-sensitive staphylococcus aureus (MSSA) and pseudomonas pneumonia, and 2 months later he endured coronavirus disease 19 (COVID-19) pneumonia. This, along with several recurrent urinary tract infections (UTIs), prevented a planned cranioplasty. He eventually recovered from COVID-19, and he was later deemed appropriate to be brought to the ORs for an elective cystoscopy and cystolitholapaxy to address his recurrent UTIs. Prior to his arrival in the OR, the patient was noted to be at his baseline vegetative state with a Glasgow coma score of 7 for eye opening and unresponsive to commands. While at our institution the patient had no abnormal lab values. There were no obvious concerns regarding the procedure or anesthesia.
The patient was brought to the OR and noted to be spontaneously breathing through the tracheostomy. Of note, at that time, the tracheostomy cuff was not inflated. He was then connected to the anesthesia ventilator circuit. Upon inflation of the tracheostomy cuff, the patient started coughing. Sevoflurane was administered through the circuit; however, spontaneous ventilation or assisted ventilation proved to be ineffective. The patient appeared agitated while the measured oxygen saturation decreased to ~70s% with peak pressures measuring 29 cmH2O. In order to remove a potential mucus plug in the tracheostomy tube, suctioning of the tracheostomy was attempted without successful return of mucus or improvement in ventilation. The oxygen saturation continued to decrease to 64%, and the patient became bradycardic. Anesthesia was deepened using propofol, and the patient was paralyzed with succinylcholine. Eventually, the patient developed profound hypotension then pulselessness and chest compressions were initiated. At this point, the decision was made to perform an oral endotracheal intubation, bypassing the tracheostomy tube. Video laryngoscopy revealed a grade IIa view, and the tracheostomy tube was removed to advance the endotracheal tube from above. Following intubation of the trachea, end-tidal CO2 and ventilation were confirmed, and peak pressures decreased to 15 cmH2O. The patient was noted to have a successful return of spontaneous circulation (ROSC) and his heart rate normalized. Chest compressions were discontinued when a blood pressure of 200/110 mmHg was observed.
Visualization of the tracheostomy tube after removal from the patient showed a mucus plug in the distal portion that had hardened into a “rock-like” appearance. The inner canula was also found to be missing. A subsequent root cause analysis which included discussion with the family revealed that due to a COVID-19 infection, suctioning of the tracheostomy tube had not been performed as regularly, thus eventually resulting in a crystalized mucus formation. Postoperatively, the patient returned to his baseline and was able to be discharged from the hospital to a long-term care facility.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying image. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
Greater than 100,000 tracheostomies are performed annually in the United States and complications are relatively common (7). Anesthesiologists are considered “airway experts”, and as such are often called to emergencies involving a tracheostomy. Nevertheless, the exact details of published guidelines can be difficult to remember during an emergency and anecdotally we find relatively few clinicians, even anesthesiologists who are familiar with tracheostomy management guidelines. Frequently the expectation is that patients with an existing tracheostomy will be a straightforward case, especially if an established tracheostomy tube with an inflatable cuff is present. When coming to the OR these patients are often simply connected to the circuit and a volatile anesthetic is administered until the patient reaches an adequate depth of anesthesia to perform the surgical procedure. Eventually, anesthesia may be supplemented with narcotics and muscle relaxants as needed. However, in our case, the patient started coughing when the cuff was inflated. This is not unusual as the inflated cuff irritates the tracheal mucosa which is sensed as pain. Believing the root cause to be pain, the team believed deepening the anesthetic would solve the problem. However, ventilation continued to be impossible, and at this point, either severe bronchospasm or a mucus plug was suspected. Administering a small amount of intravenous epinephrine and attempts to suction mucus or a mucus plug were unsuccessful. When later reviewing elements of the case, it was found that the provider who attempted to suction may not have realized that the plastic catheter was not advancing down the tracheostomy tube, highlighting that the pressure of emergencies makes even simple things difficult.
Explanations of findings
Current tracheostomy emergency guidelines emphasize the need to evaluate the tracheostomy tube for patency if ventilation is impossible. Reflecting this need, a key question in the guidelines is: “Can you pass a suction catheter?”. However, in our case the provider believed they were able to successfully pass a suction catheter and assumed that the tracheostomy was patent. At this point continuation of ABCDE (Airway, Breathing, Circulation, Disability, Environment) assessment is recommended based on the current guidelines. We indeed followed this concept, performing chest compressions and further assessing the airway. As we assumed that something was wrong with the tracheostomy tube, the decision was ultimately made to orally intubate from above which resolved the problem. However, since we believed that we in fact had initially passed a suction tube, we also were afraid that we could simply lose the airway as the tracheostomy tube could have created a false lumen which would have prevented us to from intubating from above or reinserting the tracheostomy tube. Nevertheless, reintubation from above resolved the issue, the patient recovered instantly, and the elective cystoscopy was successfully performed. Following a cranioplasty the patient was discharged to a nursing facility without any further sequelae.
Comparison with similar case reports
We were unable to find any case reports in the literature describing a similar scenario, and we were also unable to find a previous report of a tracheostomy mucus plug crystallizing into an impassable stone. The only similar case report described a mucus plug that was distal to the tracheostomy tube, and prevented suctioning but still permitted passage of a suction catheter (6). Interestingly, discussing the problem with the family revealed that the development of such a mucus plug might have been caused by COVID-19 pneumonia during the pandemic. Due to fear of COVID-19, suctioning was performed less regularly than it would have without such a devastating infection. This also resulted in a missing inner cannula. In fact, one of the functions of the inner cannula is to avoid an accumulation of mucous plugs or other obstructions.
Limitations
As this patient was bedridden, succinylcholine was in theory contraindicated (8). However, as some motor activity and low potassium prior to inducing had been noted, we decided to give succinylcholine. In theory, this can lead to hyperkalemic cardiac arrest. However, as intubation and re-oxygenation resolved the issue instantly combined with the absence of hyperkalemia, this seems very unlikely.
Conclusions
Implications and actions needed
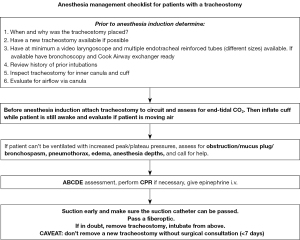
In summary, this case highlights the often-quoted phrase, “if in doubt, take it out”, and reminds us of the importance of modifying the differential diagnosis based on response/non-response to specific therapeutic airway interventions. Based on the lack of an Anesthesia specific pathway for these scenarios, a proposed airway checklist and pathway has been designed and attached (Figure 3). We would like to emphasize though, that the concept “if in doubt, take it out” is somehow simplified and under certain circumstances this might not be the best approach. E.g., a tracheostomy that is younger than 7 days could be such a scenario: here, removing the tracheostomy tube might result in a complete loss of the airway and death (9). As this patient was transferred from a nursing facility it is important to follow the initial checks as outlined on our airway pathway. E.g., initial evaluation of the tracheostomy regarding inner cannula might have been able to prevent the events in the OR. Nevertheless, it highlights that checklists and improved understanding of tracheostomies are important for tracheostomy patients and should be used whenever patient care is transferred from one team to another.
Acknowledgments
Funding: Research reported in this publication was supported by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1834/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1834/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1834/coif). T.E. serves as an unpaid editorial board member of Annals of Translational Medicine from November 2021 to October 2025. T.E. reports receiving funding from National Heart, Lung, and Blood Institute under Award Number: R56HL156955 for this study. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying image. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rosero EB, Corbett J, Mau T, et al. Intraoperative Airway Management Considerations for Adult Patients Presenting With Tracheostomy: A Narrative Review. Anesth Analg 2021;132:1003-11. [Crossref] [PubMed]
- McGrath BA, Wilkinson K. The NCEPOD study: on the right trach? lessons for the anaesthetist. Br J Anaesth 2015;115:155-8. [Crossref] [PubMed]
- Lewith H, Athanassoglou V. Update on management of tracheostomy. BJA Educ 2019;19:370-6. [Crossref] [PubMed]
- Cook T, Woodall N, Frerk C. Fourth National Audit Project of the Royal College of Anaesthetists and Difficult Airway Society. Major Complications of Airway management in the United Kingdom. Report and Findings. London: Royal College of Anaesthetists; 2011.
- McGrath BA, Bates L, Atkinson D, et al. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia 2012;67:1025-41. [Crossref] [PubMed]
- Law JA, Mariotti C, Mullen T. Failure of both suction catheter passage and bronchoscopy to diagnose an obstructing tracheal mucus plug. Can J Anaesth 2012;59:911-2. [Crossref] [PubMed]
- Cheung NH, Napolitano LM. Tracheostomy: epidemiology, indications, timing, technique, and outcomes. Respir Care 2014;59:895-915; discussion 916-9. [Crossref] [PubMed]
- Hager HH, Burns B. Succinylcholine Chloride. 2023.
- Simon M, Metschke M, Braune SA, et al. Death after percutaneous dilatational tracheostomy: a systematic review and analysis of risk factors. Crit Care 2013;17:R258. [Crossref] [PubMed]


