Measuring soluble CD40 ligand: it is a fancy prognostic biomarker in STEMI-patients?
Acute coronary syndromes are accompanied by progressive mechanical obstruction, dynamic obstruction, and plaque inflammation, instability, and rupture, followed by superimposed thrombosis. Myocardial ischemia and necrosis are the sequelae, followed over time by remodeling ventricular. Thus, activation of select markers and enzymes during the different phases of the process can be detected in the peripheral circulation (1).
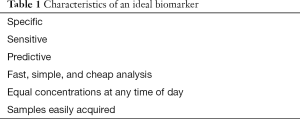
The coronary inflammation is a primary driving force for the development and progression of atherosclerosis and, thus, increased inflammation is also a common indicator of coronary atherosclerosis. An understanding of the pathobiology of atherosclerosis and the molecular events implicated in the progression from subclinical disease to overt disease has enabled the development of biomarkers to cardiovascular diseases (2,3). The vascular wall releases molecules into the bloodstream that can reflect the pathological processes taking place there. On the other hand, blood itself is clearly involved in thrombus formation. Thus, in theory, the concentrations of the molecules involved in the different pathological processes present in atherosclerosis could be biomarkers. However, not all of these molecules are suited to this aim and should fulfil certain conditions (4,5). The characteristics of an ideal biomarker are shown in Table 1. Although most of the biomarkers studied up to now have been based on the possibility of being useful from the diagnostic/prognostic standpoint, it is worth recalling that ideally they would also provide a therapeutic target. Finally, although some have no diagnostic or therapeutic value, they can provide us with information on the origin and formation of atheromatous plaque (6).
Full table
Atherosclerotic plaque instability leading to adverse events is the consequence of a complex inflammatory response of the vessel wall that involves the activation of macrophages and T cells and the production of inflammatory mediators (6). Likewise, increasing evidence suggests that CD40 ligand plays an important part in disease progression and plaque destabilization (7). The CD40-CD40 ligand system is widely distributed on a variety of leukocytic and non-leukocytic cells, including endothelial and smooth muscle cell (8), and on activated platelets (9). The CD40 ligand also occurs in a soluble form that is fully active biologically termed soluble CD40 ligand (sCD40L) (10), which are shed from stimulated lymphocytes and are actively released after platelet stimulation
The study of Napoleão et al. (11) was designed to identify the groups of ST segment elevation myocardial infarction (STEMI) patients with different profiles of sCD40L concentrations and verify how medication, clinical evolution, biochemical data, and markers of regulation of endothelial function at genetic (endothelial nitric oxide synthase polymorphisms) and post-transcriptional levels (circulating microRNAs) affect sCD40L serum levels. The results of this study showed that low levels of SCD40L 1 month after percutaneous coronary intervention distinguish STEMI patients with worse prognosis, a compromised cardiac healing, and a persistent endothelial dysfunction, as given by the association between genetic and post-transcriptional markers (11).
Nonetheless, the suggestion by Napoleão et al. (11) to encourage further studies to evaluate the clinical role of sCD40L may be overenthusiastic. Certainly, further confirmatory data from large prospective studies are needed. In everyday clinical practice, we also need simple pragmatic and practical predictors of adverse outcomes. The cardiac troponins and brain natriuretic peptide are obvious examples that are already in use. The sceptic would therefore argue that it is not only the fancy biomarker (e.g., sCD40L) that can provide clear prognostic information for death or heart failure post-acute myocardial infarction, but even very simple biomarker, such as admission troponin levels can be of value not only in assessing prognosis for cardiac events post-acute myocardial infarction but also the response to treatment. Perhaps we need to concentrate on simple things in life rather than look for too many exotic things that may be complex and expensive to measure.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by Section Editor Zhijun Han, MD (Department of Laboratory Medicine, Wuxi Second Hospital, Nanjing Medical University, Wuxi, China).
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Voudris KV, Chanin J, Feldman DN, et al. Novel Inflammatory Biomarkers in Coronary Artery Disease: Potential Therapeutic Approaches. Curr Med Chem 2015;22:2680-9. [Crossref] [PubMed]
- Rader DJ. Inflammatory markers of coronary risk. N Engl J Med 2000;343:1179-82. [Crossref] [PubMed]
- Morrow DA, Braunwald E. Future of biomarkers in acute coronary syndromes: moving toward a multimarker strategy. Circulation 2003;108:250-2. [Crossref] [PubMed]
- Domínguez-Rodríguez A, Abreu-González P. Inflammatory biomarkers in the acute coronary syndrome. Med Clin (Barc) 2011;136:461-2; author reply 462. [PubMed]
- Martín-Ventura JL, Blanco-Colio LM, Tuñón J, et al. Biomarkers in cardiovascular medicine. Rev Esp Cardiol 2009;62:677-88. [Crossref] [PubMed]
- Lubrano V, Balzan S. Consolidated and emerging inflammatory markers in coronary artery disease. World J Exp Med 2015;5:21-32. [Crossref] [PubMed]
- Dominguez-Rodriguez A, Abreu-Gonzalez P, Garcia-Gonzalez MJ, et al. Diurnal variation of soluble CD40 ligand in patients with acute coronary syndrome. Soluble CD40 ligand and diurnal variation. Thromb Res 2009;123:617-21. [Crossref] [PubMed]
- Schönbeck U, Libby P. The CD40/CD154 receptor/ligand dyad. Cell Mol Life Sci 2001;58:4-43. [Crossref] [PubMed]
- Henn V, Slupsky JR, Gräfe M, et al. CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells. Nature 1998;391:591-4. [Crossref] [PubMed]
- Henn V, Steinbach S, Büchner K, et al. The inflammatory action of CD40 ligand (CD154) expressed on activated human platelets is temporally limited by coexpressed CD40. Blood 2001;98:1047-54. [Crossref] [PubMed]
- Napoleão P, Cabral LB, Selas M, et al. Stratification of ST-elevation myocardial infarction patients based on soluble CD40L longitudinal changes. Transl Res 2016;176:95-104. [Crossref] [PubMed]


