Robotics accuracy in orthopaedics: is it enough for a well-working knee replacement?
Introduction
Continued interest in developing ways to improve reliability and accuracy of implanting joint replacements has been giving a constant boost to cutting-edge technologies designed to assist surgeons and hopefully to improve clinical results.
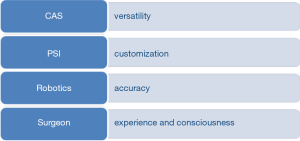
Computer-assisted surgery (CAS), patient specific instrumentation (PSI) and robotic systems have been proposed to aim to that “perfection”, in the attempt to customize the operation to each patient (Figure 1). Although these techniques tend to reduce the number of outliers (thereby making the implant positioning more reliable), each one has its own advantages and disadvantages in terms of clinical results, surgical time and cost-effectiveness. While CAS and PSI are relegated mainly to a passive role, acting as a guidance to the surgeons, robotics achieve an active or semi-active role during the operations, performing or constraining some surgical steps.
In recent years, robotics has been gaining great interest among both caregivers and patients in several fields of medicine including orthopaedics. Robotics has been proposed for many urological, ocular or orthopaedics procedures in a bid to improve their consistency and quality. This is because it’s believed that robotics may reduce the risk of complications improving clinical outcomes of these operations. Around 90% of all radical prostatectomy for cancer of the prostate in the United States are performed with robotics assistance (1) and various studies have proven the safety and efficacy of this technique (2,3). First robotic orthopaedics applications were proposed in 1992 for cementless total hip replacement (Robodoc, ISS, Sacramento, CA, USA) (4). Since then several modifications and further applications have been introduced.
In a broader context, Isaac Asimov firstly realized the emerging role of robotics in everyday life, proposing the “Three laws of robotics” to delimit aims and responsibilities of machines (5). The first law states that a robot may not injure a human being or through inaction, allow a human being to come to harm. We can assume that this is a general rule clearly valid also in medicine. Introducing robots in health care aims to overcome human limits improving accuracy and reliability. Obedience to orders given by human beings except where such orders would conflict with the first law is recommended by the second law. Again, this seems to be pretty obvious and at the beginning orthopaedics robots used to work in complete autonomy carrying out a pre-operative planning proposed by the surgeon. Further evolutions progressively have given more responsibility to robots as they assist the surgeons, being able to actively constrain human hands if the cutting mill is going in a forbidden zone out of the planned target or close to sensitive structures, thus becoming intelligent tools under direct control of the operator. The third law, about self-preservation, hardly fits surgical robots as their existence is determined more by accuracy and clinical results but also commercial interests.
Robotics in knee replacement
Published papers about robotics in knee replacement, both prospective and retrospective with or without a control group, usually agree on better radiological outcomes in terms of alignment and implant positioning (6,7). Major complications are rarely reported in primary joint replacement surgery (either with or without the use of robots) and clinical benefits of the use of the robotics are not so evident. In a recent study, Bell et al. clearly confirm what we might expect (8). Accuracy of component positioning in unicompartmental knee replacement (UKR) is improved in the robot-assisted group, reducing also the number of outliers. As this was the main aim of the study, its design allowed to reach this result. Similar findings have been cited by other surgeons as well, confirming the safety of robotics in joint replacement surgery (9).
On the other hand, this doesn’t mean that robotics is mandatory to replace a joint. It also remains unclear as to whether this technology will bring along improvement in clinical outcomes. As stated in the discussion of this paper, authors are aware that the obtained improvement in positioning may not be strictly correlated to better clinical outcomes or implant survival. This should be the second step of a perspective study but, the results from any study with the use of a specific implant may not be generalizable to other implants. The tolerance for implanting different UKRs varies greatly, e.g., Oxford UKR may tolerate a wider range of component positioning around the intended target as compared to fixed bearing UKR designs. In fact, the relative position of the femoral component in relation to the tibial component is far more crucial than the absolute position of either the femoral or the tibial components themselves.
Restoring a neutral mechanical axis has been usually considered the main aim for a total knee replacement to minimise wear, reduce the risk of aseptic loosening and thereby improve implant survival (10). When approaching unicompartmental osteoarthritis with an UKR, we aim to restore the correct soft tissue balance replacing the worn cartilage and the resected bone, thus trying to reproduce the physiological knee kinematics. This means that an intra-operative step-by-step check has to be carried out to guarantee a well-balanced (and not necessarily a normally aligned) knee. Surgeon’s experience is crucial in performing the optimal choice in terms of implant positioning and sizing or bearing thickness to obtain a stable but mobile knee. Robotics systems based on pre-operative imaging rely mainly on bony structures without considering soft tissues. Last generation robots try to bypass that limit allowing a dynamic ligament balancing to improve implant kinematics (11).
Robotics, with CAS and PSI as well, try to make orthopaedics as quantitative as possible (12), reducing a knee replacement to a well or unwell positioned implant and an aligned or mal-aligned lower limb if it falls within strict tolerance values. Until these are the considered outcomes, new technologies usually succeed to hit the target, forgetting that the outcome that really matters is reducing the revision rate, with a long lasting, painless and stable joint (13).
Robotics may assume an emerging role also in surgical education as it can guarantee high-fidelity simulation for young doctors, giving an immediate and continuous feedback in every step of the procedure. On the other hand, it cannot be seen as an alternative to surgeon’s competence as he/she holds his/her role also in the unexpected event of hardware or software failure which makes necessary to convert to conventional techniques. This means also that traditional tools have to be available in the operating room or nearby just in case the need arises.
Conclusions
Breaking news and advances in medicine are usually burdened by higher costs. Nowadays it becomes a priority to understand if it is really worth to invest large amount of money in this direction. Although preliminary results are promising, long term clinical results are needed to really appreciate robotics benefits. In conclusion, we do not expect that robotics, but either navigation or PSI, make the job easier but at least safer for the patients without forgetting that a good operation begins long before the surgical incision with the right indication.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Commentary commissioned by Section Editor Pengfei Lei, MD (Clinical research fellow at Department of Orthopedic Surgery Brigham and Women’s Hospital, Harvard University, Boston, MA 02115, United States; Surgeon of Department of Orthopaedic Surgery, Central South University Xiangya Hospital, Changsha, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Aron M. Robotic surgery beyond the prostate. Indian J Urol 2014;30:273-4. [Crossref] [PubMed]
- Allan C, Ilic D. Laparoscopic versus Robotic-Assisted Radical Prostatectomy for the Treatment of Localised Prostate Cancer: A Systematic Review. Urol Int 2016;96:373-8. [Crossref] [PubMed]
- Trinh QD, Sammon J, Sun M, et al. Perioperative outcomes of robot-assisted radical prostatectomy compared with open radical prostatectomy: results from the nationwide inpatient sample. Eur Urol 2012;61:679-85. [Crossref] [PubMed]
- Paul HA, Bargar WL, Mittlestadt B, et al. Development of a surgical robot for cementless total hip arthroplasty. Clin Orthop Relat Res 1992.57-66. [PubMed]
- Moran M. Three laws of robotics and surgery. J Endourol 2008;22:1557-60. [Crossref] [PubMed]
- Lonner JH, Smith JR, Picard F, et al. High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res 2015;473:206-12. [Crossref] [PubMed]
- Song EK, Seon JK, Yim JH, et al. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 2013;471:118-26. [Crossref] [PubMed]
- Bell SW, Anthony I, Jones B, et al. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J Bone Joint Surg Am 2016;98:627-35. [Crossref] [PubMed]
- Citak M, Suero EM, Citak M, et al. Unicompartmental knee arthroplasty: is robotic technology more accurate than conventional technique? Knee 2013;20:268-71. [Crossref] [PubMed]
- Abdel MP, Oussedik S, Parratte S, et al. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J 2014;96-B:857-62. [Crossref] [PubMed]
- Plate JF, Mofidi A, Mannava S, et al. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop. 2013;2013:837167.
- Pearle AD, Kendoff D, Musahl V. Perspectives on computer-assisted orthopaedic surgery: movement toward quantitative orthopaedic surgery. J Bone Joint Surg Am 2009;91 Suppl 1:7-12. [Crossref] [PubMed]
- Chun YS, Kim KI, Cho YJ, et al. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty 2011;26:621-5. [Crossref] [PubMed]


