Successful surgical treatment of a complicated esophageal perforation, by use of primary closure and lung parenchyma reinforcement
Introduction
Esophageal perforation (EP) is an uncommon medical condition which demands an urgent confrontation, as it has high rate mortality. Specific studies mention that the mortality rate varies from 30% during the first 30 days and 38.8% during the first 90 days (1). The most significant complications of this condition are mediastinitis and pyothorax, caused by the leakage of gastric content and food into the mediastinum. As the disease develops, systemic sepsis and shock may evolve within hours.
The cause of the perforation of the esophagus may be rather common (existence of tumor, ulceration), spontaneous or iatrogenic (47.6%). The spontaneous rupture appears at a frequency of 31.1%, while other causes, such as a surgical intervention, at a rate of 3.1% (2). The interval between the injury and its following treatment is the most important factor in the confrontation of the EP, with its prognosis deteriorating when diagnosis and treatment are delayed past the first 24–48 hours (3). The therapeutic strategy may be conservative, mostly in cases of iatrogenic EP (4), or invasive. Surgical intervention is needed in the majority of incidents, having as main goal the drainage of the mediastinum. There are different surgical approaches, depending on the characteristics of the lesion (5,6).
Case presentation
A 68-year-old man was admitted to our hospital due to diarrhea, nausea and vomiting. The patient’s initial clinical examination detected increased intestinal sounds, without a certain imaging of intestinal obstruction on a simple X-ray.
His personal medical history indicated operated carcinoma of the colon, performed 12 months ago and followed by consecutive chemotherapy, transurethral prostatectomy due to benign prostate hyperplasia and daily abuse of alcohol (before the diagnosis of the colon cancer).
Three days after his hospitalization, the patient was submitted to esophagogastroduodenoscopy, during which an ulcerative lesion was found at a distance 31 cm approximately from the dental barrier, with a coexistent stenosis that did not prevent the transit of the endoscope. A biopsy from the lesion area was performed. On the 5th day, the patient complained of asphyxiation during eating. A thorax CT scan was performed, depicting a sizable fluid and gas collection in the mediastinum, due to abnormal communication between the esophagus and the mediastinum, and co-existing pleural effusion bilaterally. The CT findings confirmed the existence of mediastinitis, while an antibiotic therapy was prescribed. A naso-gastric tube was placed, followed by the patient’s transfer to the thoracic surgery department. It is believed that the perforation of the esophagus probably took place within the previous 24–48 hours before the final diagnosis. Due to the patient’s critical condition, the outcome of any surgical intervention was extremely unpredictable.
Despite the uncertainty of the surgical outcome, after a full appraisal of the gathered facts the decision to move on to a surgical intervention was immediate. The patient was submitted to a right posterolateral thoracotomy, which highlighted an extensive purulent necrotic mediastinitis. The main goals of this surgery were the removal of the tissues which were affected by the infection, the successful and efficient drainage of the mediastinum, the assurance of an efficient respiratory function and finally the overall restoration of the esophagus.
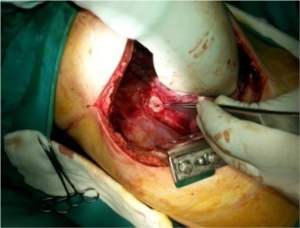
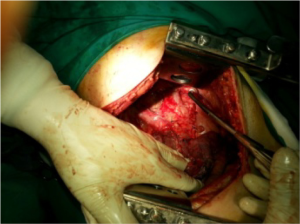
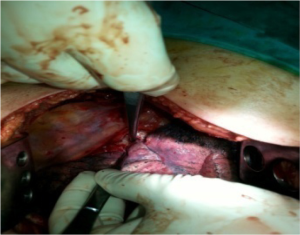
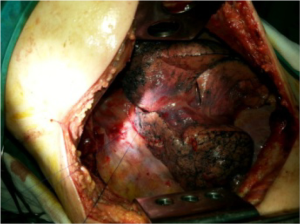
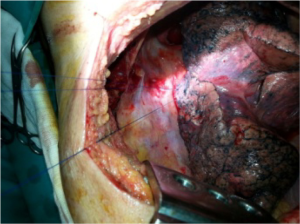
The procedure’s first step was the administration of general anesthesia with a double-lumen endotracheal tube. A right posterolateral thoracotomy was performed via the right 5th intercostal space and the entrance in the pleural cavity revealed an image of advanced mediastinitis as well as the existence of pneumopyopericardium. The point of the esophageal rupture was discovered in the lower 1/3 of the esophagus, with a deficit of 3 cm diameter (Figure 1). The infection extended in the pleural cavity with the presence of scattered outbreaks. The infected tissues were removed and the co-existing effusion was drained, followed by a total decortication of the parietal pleura and partial decortication of the visceral pleura. Additionally, a partial removal of the pericardium took place along with some necrotic sections at the point of the rupture. In order to ensure a safe restoration of the esophagus, infection-free lung parenchyma was sutured in direct contact with the rupture point, a procedure that achieved better reinforcement and its eventual tamponade. This procedure is consisted of four stitches passing through three points, the two edges of the rupture and the visceral pleura of the right lung (Figures 2-5). Pleural flap was not possible due to severe inflammatory condition of the pleura, which made it fragile. Intercostal muscle flap could be an alternate choice but we preferred the use of lung parenchyma which covered totally and in a complete tension-free anatomic way the sutured perforation. Furthermore, a wedge resection of the right upper lobe was performed along with a contained emphysematous cyst. Supplemental biopsies were taken from the parietal and visceral pleura, the pericardium, the resected part of the right upper lobe and regional lymph nodes. Finally, three thoracic drainage tubes were placed, the first one directly at the point of the rupture into the mediastinum, the second one reached the right costophrenic angle, and the third one was directed towards the apex of the pleural cavity.
After the surgery, the patient was admitted and remained for 6 days in the intensive care. His condition progressively stabilized and gradually improved, without any fever after the 4th post-operative day, while the amount of the draining pleural fluid decreased daily. The 7th post-operative day he was transferred in the thoracic surgery department, and an immediate successfully performed patency control took place, along with his initial mobilization and respiratory physiotherapy. The 12th post-operative day, after three negative cultivations collected of the drainage fluid, the first drainage tube was abstracted and subsequently the other two, one every each of the following days. The patient exited the hospital the 18th post-operative day after another successful patency control, fully mobilized and his per os feeding fully restored.
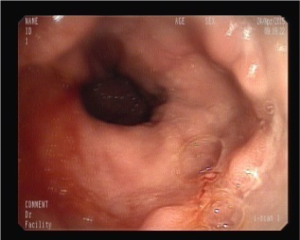
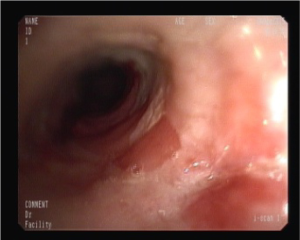
Two weeks after his discharge from the hospital, an esophagogastroduodenoscopy was performed again, showing a stenosis at the point of the rupture, while the clinical findings were the same during the next examinations (Figures 6-8).
Discussion
EP is a clinical manifestation, associated with a high mortality rate and the need of an immediate reaction. The first step for the appropriate treatment is the early diagnosis. An intervention within the first 24 hours clearly displays a better prognosis, compared with a delayed one (during the first 1–3 days), while the outcomes of a confrontation after 72 hours are disappointing (1,3). In our case, the surgical procedure that was performed between 24 to 48 hours after the rupture, forced us to a direct repair with a reinforcement technique. The severe local infection was a negative predictive factor. Nonetheless, the result was satisfactory. That means that a severe local infection does not exclude a direct surgical repair if possible.
The restoration of the damage and the ensurement of an appropriate drainage are the key points which are demanded for a positive outcome. We did not use a less invasive treatment as a first approach strategy, because our main goal was to treat mediastinitis as well as thoracic empyema. Intraoperatively, the direct suture of the perforation was technically possible. We decided to keep the stenting repair in case of a persistent leakage. However, stent insertions as well as a T tube placement are reported in the literature. Type of surgery should depend on clinical factors and surgical judgement and expertise (5-7).
Three drainage tubes are placed to ensure safe observation and count of the fluid material produced by the infection, in order to prevent complications such as mediastinitis and pyothorax. A significant point, equally critical for the post-operative evolution, is the removal of the drainage tubes. In our case, the drainage tubes were removed consecutively from the 12th to the 14th post-operative day, after the acquirement of three negative cultivations of the drained fluid. After the necessary endoscopic control, the patient began to feed gradually, initially with small portions of fluids, until the point of a fully normal diet program. He was discharged from the hospital the 18th postoperative day, totally mobilized without limitations regarding his diet. We have to point out the importance of the immediate postoperative observation control and the following long-term “follow-up” of the patient, which are absolutely necessary procedures and are performed with frequent scheduled endoscopies and depiction of the thorax.
Conclusions
The early diagnosis of an EP, followed by an immediate surgical procedure and a frequent observation and follow-up of the patient, are the main factors which significantly eliminate the risks for the patient’s life and ensure a satisfactory outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Markar SR, Mackenzie H, Wiggins T, et al. Management and Outcomes of Esophageal Perforation: A National Study of 2,564 Patients in England. Am J Gastroenterol 2015;110:1559-66. [Crossref] [PubMed]
- Ryom P, Ravn JB, Penninga L, et al. Aetiology, treatment and mortality after oesophageal perforation in Denmark. Dan Med Bull 2011;58:A4267. [PubMed]
- Lin Y, Jiang G, Liu L, et al. Management of thoracic esophageal perforation. World J Surg 2014;38:1093-9. [Crossref] [PubMed]
- Tullavardhana T. Iatrogenic Esophageal Perforation. J Med Assoc Thai 2015;98 Suppl 9:S177-83. [PubMed]
- Shen G, Chai Y, Zhang GF. Successful surgical strategy in a late case of Boerhaave's syndrome. World J Gastroenterol 2014;20:12696-700. [Crossref] [PubMed]
- Seo YD, Lin J, Chang AC, et al. Emergent Esophagectomy for Esophageal Perforations: A Safe Option. Ann Thorac Surg 2015;100:905-9. [Crossref] [PubMed]
- Santini M, Fiorello A, Cappabianca S, et al. Unusual case of Boerhaave syndrome, diagnosed late and successfully treated by Abbott's T-tube. J Thorac Cardiovasc Surg 2007;134:539-40. [Crossref] [PubMed]