Percutaneous tracheostomy—beware of the thyroidea-ima artery
Introduction
Tracheostomy is a minimally invasive operation performed in patients, in order to provide an air passage through the windpipe. Two techniques are mainly used in current practice: percutaneous dilatational tracheostomy and surgical tracheostomy. Approximately 500 patients are reported to die or remain permanently disabled due to complications after tracheostomy in the United States each year. The most common complications, which may lead to death, are dislocation of the tracheal cannula (52.4%), hemorrhage in nominate artery (40.7%), lost airway during the procedure (19%), venous bleeding (18.5%) and tracheal perforation (15.5%). Complications such as pneumothorax, bronchospasm, cardiac arrest and arrhythmia have also been recorded. Another, though rare cause of hemorrhage, is the injury of the thyroidea-ima artery (1-3).
The following case report presents a patient with hemorrhage after thyroidea-ima injury during percutaneous dilatational tracheostomy.
Case presentation
A 66-year-old male with ECOG score 3–4 was admitted to our intensive care unit (ICU) due to acute respiratory distress syndrome (ARDS).
His medical history consisted of arterial hypertension, coronary disease, multiple strokes, chronic renal failure and hyperlipidemia. He had also undergone one surgery for gastrointestinal bleeding in the past, as well as resection of aneurysm of the abdominal aorta.
As a result of hypoxia and hypercapnia, the patient was intubated and set onto synchronized intermittent mechanical ventilation (SIMV). On the 14th day of his hospitalization a percutaneous dilatational tracheostomy was decided, due to long engineering support ventilation. A transverse incision of one centimeter was performed between the 1st and 2nd tracheal ring, followed by the guide-wire placement. During the insertion of the separator there was severe hemorrhage and the patient was immediately transferred to the operating room.
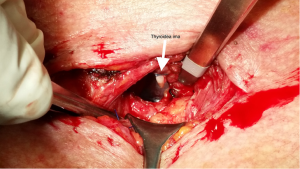
During bleeding control, an injury of the thyroidea-ima was found. The vessel was successfully ligated and surgical tracheostomy under general anesthesia was performed (Figure 1). The patient became haemodynamically stable, with no blood transfusion required and was transferred back to the ICU.
The patient was discharged from our hospital on the 15th postoperative day. Three months post operation, the patient was no longer in need of the tracheostomy and decannulation was performed.
Discussion
Thyroidea-ima is an artery that is normally found during fetal life and occurs as an anatomical variant in 3–10% of the population. Johann E. Neubauer first described it in 1772 and hence it has since been referred to as the thyroid artery of Neubauer. Although thyroidea-ima arises mainly from the brachiocephalic trunk, it may also originate from the aortic arch, the right common carotid artery, the subclavian artery, the cardiophrenic artery, the thyrocervical trunk or the internal mammary artery. Thyroidea-ima ascends in front of the trachea to the bottom of the thyroid gland. It varies greatly in size and ranges from 3–5 mm in diameter. It supplies blood into the thyroid gland mainly as an offset in the absence of the bellow thyroid arteries but it can also perfuse the trachea and the parathyroid glands. Due to its small size and because of its scarce presence it may cause serious complications, such as severe bleeding, during surgical operations (1,4-8).
Knowledge of its existence is very important when performing thyroidectomy or tracheostomy, either percutaneously or with open surgery, especially when in emergency circumstances. In certain cases it may cause serious injury or fatal hemorrhage. To our knowledge, there is not a specific method in order to avoid the injury of the thyroidea-ima artery. This vessel is an anatomic variation and its presence cannot be predicted. Surgeons should always be aware and suspicious of its presence, when operating.
Tracheostomy is an emergency surgical operation performed in order to keep the vents open and can be done either percutaneously or surgically. In percutaneous dilatational tracheostomy the preferred site of entry is between the first and the second or the second and third tracheal rings under sterilized conditions (9). Initial skin incision and blunt preparation of the pretracheal tissue may be helpful to identify the tracheal rings, thus avoiding either too high or too low tracheal puncture. It is of vital importance that before the procedure is carried out, the anatomical landmarks of the cricoid cartilage and the sternal notch must be successfully identified (10).
In percutaneous tracheostomy the use of bronchoscope improves the safety of the procedure by facilitating direct internal visualization of the needle or cannula in the tracheal lumen and optimal positioning. It also helps in patients with a difficult anatomy, and to remove aspirated blood. However, the routine use of bronchoscopy in percutaneous dilatational tracheostomy is not yet established, as there are reports of complications under bronchoscopic guidance in the literature. The physician’s experience, the anatomic variations and the individualization of patients are the factors that should define the use of bronchoscopy or not. Nevertheless, a bronchoscope must always be stand-by, in case of emergency (10).
In surgical tracheostomy the incision is done in the middle of the distance between the cricoid cartilage and the sternal notch. The isthmus of thyroid is prepared and a tracheal window is formed with subtraction of a circular area between 2nd and 3rd or 3rd and 4th tracheal rings (11). Injury of the thyroidea-ima can arise followed by excessive hemorrhage. In such cases urgent sternotomy is usually required to control the bleeding. However, in our case the hemodynamic vital signs of the patient, yet crucial, allowed us to try a less minimally invasive method, in order to avoid an extensive surgery that the patient couldn’t probably tolerate. In case of failing to control bleeding, an urgent sternotomy would be necessary nonetheless.
This case report presents a patient with hemorrhage after thyroidea-ima injury during percutaneous dilatational tracheostomy. The technique that was used was a single tapered dilatational method, which is a modification of the Ciaglia technique and uses a single tapered dilator. This technique is a safe and reliable method with the minimum time required. There are many different techniques that are widely used, such as the Ciaglia’s technique with serial dilation, the Grigg’s technique and lately the translaryngeal tracheostomy. All the above techniques use the Seldinger method to insert a guide wire into the trachea (12).
It is widely accepted that the use of percutaneous dilatational tracheostomy has improved several aspects of patient care. However, it is not without risk and should be carefully considered in all cases. The method of choice should be based on the physician’s experience and expertise.
In conclusion, it should be taken into account that the injury of the thyroidea-ima while performing percutaneous dilatational or surgical tracheostomy is one of the most unusual, yet fatal, causes of hemorrhage. Effective treatment requires the patient’s immediate transfer into the operating room. Surgeons should always be aware of such anatomic variation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Singh V. Clinical and Surgical Anatomy (2nd ed.). Elsevier Health Sciences, 2012:301-3.
- Shlugman D, Satya-Krishna R, Loh L. Acute fatal haemorrhage during percutaneous dilatational tracheostomy. Br J Anaesth 2003;90:517-20. [Crossref] [PubMed]
- Simon M, Metschke M, Braune SA, et al. Death after percutaneous dilatational tracheostomy: a systematic review and analysis of risk factors. Crit Care 2013;17:R258. [Crossref] [PubMed]
- McKenzie GA, Rook W. Is it possible to predict the need for sternotomy in patients undergoing thyroidectomy with retrosternal extension? Interact Cardiovasc Thorac Surg 2014;19:139-43. [Crossref] [PubMed]
- Banneheka S, Chiba S, Fukazawa M, et al. Middle thymothyroid artery arising from the common carotid artery: case report of a rare variation. Anat Sci Int 2010;85:241-4. [Crossref] [PubMed]
- Bergman RA, Afifi AK, Miyanchi R. Thyroidea Ima (of Neubauer) Artery. Illustrated Encyclopedia of Human Anatomic Variation: Opus II: Cardiovascular System: Arteries: Head, Neck, and Thorax. Available online: http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Text/Arteries/ThyroideaIma.shtml
- Moore NA, Roy W. Rapid Review Gross and Developmental Anatomy, 3rd Edition. Elsevier Health Sciences, 2010:220.
- Barbetakis N, Asteriou C, Paliouras D, et al. eComment. Substernal goiter. Beware of the thyroidea ima artery. Available online: https://www.academia.edu/14652799/eComment._Substernal_goiter._Beware_of_the_thyroidea_ima_artery?auto=download
- Brand-Saberi BE, Schäfer T. Trachea: Anatomy and Physiology. Thorac Surg Clin 2014;24:1-5. [Crossref] [PubMed]
- Petros S. Percutaneous tracheostomy. Crit Care 1999;3:R5-R10. [Crossref] [PubMed]
- ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg 2013;74:1363-6.
- Batuwitage B, Webber S, Glossop AJ. Percutaneous tracheostomy. Contin Educ Anaesth Crit Care Pain 2014;14:268-72. [Crossref]


