The challenge of early identification of the hospital patient at risk of septic complications
It is evident that the patient with sepsis needs immediate attention to allow rapid and effective intervention. Recently, the Sepsis-3 Definitions task force used multivariable logistic regression to develop the qSOFA—a short sequential organ failure assessment (SOFA) score that incorporates a systolic blood pressure of 100 mmHg or less, a respiratory rate of 22/min or greater and/or an acute alteration in mentation—to be used as a means of identifying infected patients on the general ward who may need urgent attention and further workup for possible sepsis (1,2). In a retrospective analysis of more than 65,000 records from out-of-ICU patients with suspected infection, the task force investigators reported that the qSOFA had a predictive validity for in-hospital mortality [area under the receiver operating characteristics curve (AUROC)] of 0.81 [95% confidence interval (CI): 0.80–0.82]. This was a little better than that of the systemic inflammatory response syndrome (SIRS) criteria (AUROC 0.76; 95% CI: 0.75–0.77; P<0.001) and even the full SOFA score (AUROC 0.79; 95% CI: 0.78–0.80; P <0.001) (2). The authors concluded that these data therefore supported the use of the qSOFA as a prompt to suggest the possible presence of sepsis. However, another article that collected data from 30,677 emergency room and hospital floor patients with suspected infection suggested that the National Early Warning Score (NEWS; AUROC 0.77; 95% CI: 0.76–0.79) and the Modified Early Warning Score (MEWS; AUROC 0.73; 95% CI: 0.71–0.74), two established and widely used scoring systems, were more accurate than the qSOFA (AUROC 0.69; 95% CI: 0.67–0.70) for predicting in-hospital mortality (3).
Indeed, since publication of the Sepsis-3 definitions (1,2), the whole qSOFA concept has created considerable debate and some confusion. I would like to make a few points that I think are important.
The qSOFA is not part of the definition of sepsis
The qSOFA was developed as an alert that a non-ICU patient may be deteriorating and may require ICU admission or further workup for sepsis. The qSOFA is NOT part of the definition of sepsis, as we have already stressed (4). So, why did we add it? Simply because the consensus definition committee felt that just stating that sepsis is organ dysfunction associated with an infection would not have sufficient impact without some additional data: that is the only reason why the qSOFA was added.
What is the real challenge?
The differences between the scores reported by Churpek et al. are relatively small with AUROCs of 0.77, 0.73, and 0.69 for NEWS, MEWS and qSOFA, respectively. Are these differences really clinically important? Do they matter to our patients? And what do they actually represent? The answer to this last question is: prediction of in-hospital mortality. But, if this is really the aim, then by adding age and a couple of serious morbidities, such as chronic renal failure or complicated diabetes, to the qSOFA score, the AUROC will easily be higher than those reported (except perhaps for the APACHE and SAPS scores that were specifically designed for this purpose).
We have focused much on the prediction of hospital mortality in patients with sepsis, when the real issue is how best to identify early a process that should be reversed as rapidly as possible; how best to recognize a patient with suspected infection who requires immediate attention (5,6). The systemic inflammatory response syndrome (SIRS) criteria were not very good for this purpose, with almost 50% of patients hospitalized on the regular floor meeting the SIRS criteria at least once during their hospital stay (7).
There are also some important ethical issues associated with the use of a ‘warning’ score routinely in all patients with suspected infection. Sepsis can affect many people, and treatment may not necessarily be ‘appropriate’ in all of them. Indeed, many people can die of sepsis, not only in the intensive care unit (ICU) but also on the regular floor, for example patients with terminal cancer, massive stroke and other advanced neurologic diseases. In some of these patients with terminal conditions, the sepsis process may represent a way of dying without suffering, and treatment should not be started. These aspects are summarized well in a “perspective” article written by an emergency room doctor confronted with an elderly patient with multiple comorbidities, including advanced dementia, who was admitted from her care home with septic shock (8). The doctor, in a hurry to start vasopressors, was struck by a daughter’s question as to whether this treatment was really necessary. After further discussion, it was decided that the mother would not have wanted to be kept alive in her condition; treatment was deferred and the mother died comfortably the following day. The Surviving Sepsis Campaign guidelines for sepsis management (9) provide good recommendations, but they should only be applied to individuals who can benefit from them. The blind application of a score of deterioration to all patients may not be appropriate.
What is the alternative?
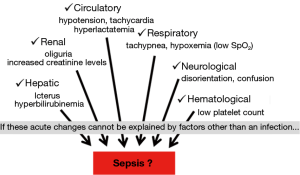
I am personally not convinced that the qSOFA is so important. Rather than relying on a specific score, what we need is more a global “awareness”. Hospital staff, of all levels, need to be trained to recognize the signs of deterioration early. The qSOFA only assesses some of the cardiovascular, respiratory and neurological functions that may be present in a patient with sepsis. Other cardiovascular factors (such as tachycardia or increased lactate levels) or other respiratory (decreased oxygen saturation measured by pulse oximetry), renal (decreased urine output) or hematological (decreased platelet count) signs may also be important warning signs.
What I believe is a more relevant approach, therefore, is that all health care providers are aware of the six organs whose function needs to be checked and the associated indicators of dysfunction (Figure 1). There is no need for everyone to know the full SOFA score by heart, and not even a need to have it as an app on your smartphone or smart watch. Today, at least in high income countries, nurses look at the results of blood tests and play a key role in the identification of deterioration. This was well illustrated in a recent study by Torsvik et al. (10), in which the assessment of a combination of abnormalities (hypo/hyperthermia, leukocyte count, respiratory rate, blood pressure, mental status, oxygen saturation, altered capillary refill, blood lactate level, platelet count, urine output) by nurses helped to identify sepsis patients on the floor and thereby reduced complications and improved survival rates.
In conclusion, recognition of organ dysfunction is the key to early identification of patients who may be deteriorating and need further workup to exclude or include sepsis as a diagnosis. This process does not necessarily require a specific score. If a score is considered necessary, perhaps for those who insist on rigorous protocolized patient management, then several scores are available, and the choice may not be that important.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:801-10. [Crossref] [PubMed]
- Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:762-74. [Crossref] [PubMed]
- Churpek MM, Snyder A, Han X, et al. qSOFA, SIRS, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients Outside the ICU. Am J Respir Crit Care Med 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Vincent JL, Martin GS, Levy MM. qSOFA does not replace SIRS in the definition of sepsis. Crit Care 2016;20:210. [Crossref] [PubMed]
- Vincent JL, Mira JP, Antonelli M. Sepsis: older and newer concepts. Lancet Respir Med 2016;4:237-40. [Crossref] [PubMed]
- Vincent JL. The Clinical Challenge of Sepsis Identification and Monitoring. PLoS Med 2016;13:e1002022. [Crossref] [PubMed]
- Churpek MM, Zadravecz FJ, Winslow C, et al. Incidence and Prognostic Value of the Systemic Inflammatory Response Syndrome and Organ Dysfunctions in Ward Patients. Am J Respir Crit Care Med 2015;192:958-64. [Crossref] [PubMed]
- Manasco AT, Linden JA. Does My Mother Really Need That Central Line? JAMA Intern Med 2015;175:1267. [Crossref] [PubMed]
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013;39:165-228. [Crossref] [PubMed]
- Torsvik M, Gustad LT, Mehl A, et al. Early identification of sepsis in hospital inpatients by ward nurses increases 30-day survival. Crit Care 2016;20:244. [Crossref] [PubMed]


