Development and use of a non-biomaterial model for hands-on training of endoscopic procedures
Introduction
The development of endoscopic submucosal dissection (ESD) for early gastrointestinal carcinoma and peroral endoscopic myotomy (POEM) for achalasia are outstanding recent developments in therapeutic endoscopy (1-4). The benefits of these minimally invasive curative treatments could be extended to more patients if training opportunities were more widely available to gastroenterologists and surgeons to ensure safe performance.
Presently, training methods for endoscopic procedures use live animals or extracted animal intestines (5,6). The many barriers related to the use of animals for education have, therefore, limited the availability of endoscopic training workshops. These barriers include: difficulty with infection control; the need for specialized endoscopes for animals; cost associated with obtaining additional endoscopes that are only used with the biomaterial model and not humans; variation in the quality and accessibility to animal models in different countries and states; and ethical issues associated with the use of animal models for clinical training and research. To circumvent barriers associated with the use of animal models, in 2016, we developed a new non-animal ex-vivo training model for ESD and POEM (7,8). The aim of our paper is to describe our novel model and report on feedback received after a hands-on endoscopic training workshop for ESD/POEM using our model.
Methods
Development of a non-biomaterial training model for ESD/POEM
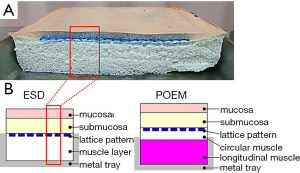
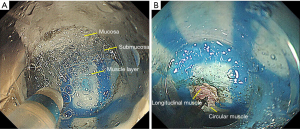
The development of the ex-vivo ESD/POEM training model ‘EndoGel’ was a joint research project between SunArrow Limited and Niigata University. The sheet was developed using polyvinyl alcohol hydrogel (PVA-H). PVA-H, which is largely comprised of water, has a high conductivity and has been shown to be suitable for therapeutic endoscopic procedures, such as mucosal incision, submucosal dissection, and muscle layer myotomy. Moreover, the mechanical properties of PVA-H can be easily modified to achieve the appropriate stiffness to model the intestine. Specifically, each PVA-H layer can be created with a different concentration and tension, and attached together to model each intestinal layer (Figure 1). The first layer is the mucosa in which initial lesion marking and circumferential incision are performed. The second layer is the submucosa, which can expand with submucosal injection. Submucosal dissection for ESD or tunneling for POEM can be performed in the same way as they would be performed in patients. The third layer is the muscle layer. The surface of the muscle layer in the model includes a ‘lattice pattern’, with a white 5 cm × 3 mm rectangle used as an indicator of the direction or width of the submucosal dissection performed in the ESD procedure or tunneling in the POEM procedure. In the POEM model, the muscle layer is composed of two types of smooth muscle layers, the inner circular muscle layer and the outer longitudinal muscle layer, with the inner circular muscle selectively dissected during POEM myotomy training (Figure 2).
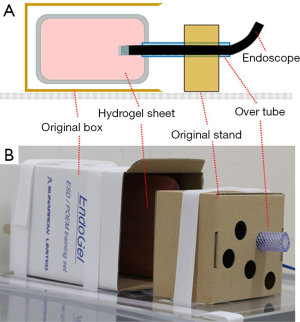
The disposable return electrode (ERBE Elektromedizin GmbH, Tübingen, Germany) is attached below the hydrogel sheet and is connected to a high-frequency generator (VIO 300D; ERBE). The hydrogel sheet is fixed onto an original box, with an over-tube prepared on another original stand. In the original box, the hydrogel sheet can be fastened to any side depending on the clinical case being simulated. To simplify the set-up of the model, an original board was also developed, allowing the model to be fixed on a table without adhesive taping (Figure 3).
Wearing a mask in a ventilated simulation room is recommended although the toxicity of smoke generated during the training is far below the level causing harmful effect to the human body.
Results
Advanced hands-on workshop using the ex-vivo ESD/POEM training model
On July 2016, we held a non-biomaterial endoscopic hands-on workshop at Niigata University for resident doctors working in the Niigata prefecture. Twenty-eight residents, having a range of medical experience of 1 to 3 years, participated in the workshop. Training using the non-biomaterial model was conducted using the same endoscope, high-frequency generator, and therapeutic devices as used for patients. Using a self-report questionnaire, participants provided feedback regarding their satisfaction with using the non-biomaterial model for training (‘satisfied’ or ‘not satisfied’). Participants also provided feedback on the feasibility (‘feasible’ or ‘not feasible) of performing procedures, including lesion marking, circumferential mucosal incision and submucosal dissection. All attendees were satisfied with the training received using the non-biomaterial model (100% satisfaction), with 27 of the 28 participants indicating that all procedures could be performed (96.4% feasibility).
Conclusions
Prior to the development of our EndoGel model, no practical models were available to train surgeons in the use of therapeutic endoscopy. A silicon-based artificial simulator was previously reported (9). However, as silicon is a stiff material, submucosal injection could not be performed in the simulator, although it is a necessary procedure to complete prior to submucosal dissection in ESD or tunneling in POEM. Animal models, which have traditionally been used for training, also do not adequately simulate the human intestine, with different histological features in porcine gastric models and different degree of ESD difficulty having been reported, depending on the lesion (10). Moreover, difficulty in training for the POEM procedure using a porcine esophagus model has also been reported due to the thinness of the submucosa (11). Therefore, the idea of using an artificial material, which has a high conductivity and softness, is clinically acceptable for the training of therapeutic endoscopy.
The feedback provided by the attendees in our hands-on workshop underlines the satisfaction and feasibility of using our non-biomaterial model for ESD/POEM training. Therefore, we consider our model to be effective for therapeutic endoscopy education in any facility equipped for endoscopy, rather than only in those with endoscopic units specialized for animal use. Our EndoGel model holds promise to extend access to endoscopy training, which would improve the therapeutic use of ESD and POEM worldwide. Furthermore, improvement of this initial model based on users’ requests is underway. Therefore, in the near future, the EndoGel model would further better simulate actual practice.
Acknowledgements
This study was supported by SunArrow Limited.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut 2001;48:225-9. [Crossref] [PubMed]
- Ono H, Hasuike N, Inui T, et al. Usefulness of a novel electrosurgical knife, the insulation-tipped diathermic knife-2, for endoscopic submucosal dissection of early gastric cancer. Gastric Cancer 2008;11:47-52. [Crossref] [PubMed]
- Eleftheriadis N, Inoue H, Ikeda H, et al. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag 2012;8:329-42. [Crossref] [PubMed]
- Inoue H, Sato H, Ikeda H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 2015;221:256-64. [Crossref] [PubMed]
- Ohata K, Nonaka K, Misumi Y, et al. Usefulness of training using animal models for colorectal endoscopic submucosal dissection: is experience performing gastric ESD really needed? Endosc Int Open 2016;4:E333-9. [Crossref] [PubMed]
- Hernández Mondragón OV, Rascón Martínez DM, Muñoz Bautista A, et al. The Per Oral Endoscopic Myotomy (POEM) technique: how many preclinical procedures are needed to master it? Endosc Int Open 2015;3:E559-65. [Crossref] [PubMed]
- Mizuno K, Sato H, Hashimoto S, et al. A novel training model composed of nonbiological materials for endoscopic submucosal dissection. Gastrointest Endosc 2016;84:373-4. [Crossref] [PubMed]
- Sato H, Mizuno K, Terai S. Novel ex-vivo training model for peroral endoscopic myotomy using hydrogel. Dig Endosc 2016;28:620. [Crossref] [PubMed]
- Chen MJ, Wang HY, Chang CW, et al. A novel artificial tissue simulator for endoscopic submucosal resection training - a pilot study. BMC Gastroenterol 2016;16:112. [Crossref] [PubMed]
- Horii J, Goto O, Shimoda M, et al. Which part of a porcine stomach is suitable as an animal training model for gastric endoscopic submucosal dissection? Endoscopy 2016;48:188-93. [PubMed]
- Sato H, Sagara S, Suzuki K, et al. Assessments of histologic changes after peroral endoscopic myotomy. Gastrointest Endosc 2016;84:377-8. [Crossref] [PubMed]


