Multi-vessel giant coronary artery aneurysm in an elderly female
Introduction
Coronary artery aneurysms (CAAs) are coronary artery segments 1.5 times the normal size. In various series of performed coronary angiographies, CCAs comprise 0.3–5.3%. The right coronary artery is usually the most commonly affected (40–87%), followed by the left circumflex (LCX), or the left anterior descending artery (LAD) (1). Three-vessel disease or left main (LM) involvement is extremely rare (0.1%) (2). CAA is a variant of coronary artery disease (CAD) with a prevalence of 4.9% and accounts for 50% of all cases found during angiography (2,3). Other potential etiologies include congenital, inflammatory such as Kawasaki disease, connective tissue disease, infectious, drug-related, traumatic, or iatrogenic. The gold standard for diagnosis is a left heart cardiac catheterization. A giant coronary artery aneurysm (GCAA) is even rarer and has a prevalence of 0.02–0.2%. It refers to an aneurysm that is 20 mm or greater in size (4). Patients with CAA are typically asymptomatic, as most are found incidentally during coronary angiography. When manifest, males with three-vessel disease, and a history of myocardial infarction (MI) are usually most commonly affected. Multiple studies have shown varying mortality rates among patients diagnosed with CAA. Whereas a study from Emory University reported 29.1% mortality from 1995–2003, the European Coronary study, a study from Greece of 3,900 patients and Coronary Artery Surgical Study (CASS) registry, from 1974–1979, reported no mortality difference (5-8). The retrospective analysis from Emory University reported that the 5-year mortality of 29.1% was irrespective of concomitant atherosclerotic CAD, but notable survival improvement was associated with those that did not have underlying CAD.
Management of symptomatic patients presenting as acute coronary syndrome (ACS) or stable ischemic heart disease (SIHD); where the CAA is the culprit lesion causing symptoms, includes either medical, percutaneous, or surgical options (2). Acute thrombosis within the aneurysm can lead to distal embolization and occasionally MI, thus depending on the severity of coronary stenosis, may need medical treatment using anticoagulation or antiplatelet therapy, and occasionally percutaneous or surgical intervention. Management of patients with LM CAAs can either be surgical or medical (2).
On the other hand, management of asymptomatic cases, or patients where CAAs are found incidentally during coronary angiogram is less clear (3).
Case presentation
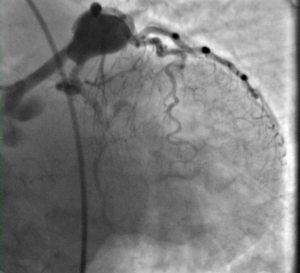
We herein describe a case of a 90-year-old female who presented with an inferior ST elevation myocardial infarction (STEMI). Coronary angiogram of the left coronary artery revealed a GCAA, 30 mm × 20 mm in size, involving the LM, LAD, and LCX (Figure 1), and angiogram of the right coronary artery revealed the culprit lesion; a significant proximal-RCA 99% sub-total occlusion, distal to an ostial mild ectatic section (Figure 2). The culprit lesion was treated by percutaneous balloon angioplasty. Heavy calcification prevented successful passage and deployment of a stent to the proximal RCA. Based on the patient’s age and clinical presentation and recovery after treatment of the RCA, it was concluded that the left coronary GCAA involvement was not generating any significant symptoms. In view of the large size of the GCAA and its involvement of the LAD and LCX, and ostial RCA, the GCAAs were deemed not suitable for a percutaneous coronary intervention, and the patient was considered too high risk for additional surgical management. She was therefore treated medically using dual antiplatelet therapy (DAPT) including aspirin and clopidogrel as well as statin therapy.

Discussion
CAA is a rare coronary abnormality with high mortality. Our case represents a unique presentation of a surviving elderly female with significant asymptomatic coronary aneurysmal involvement of all the major vessels. The incidental finding of the GCAAs in our 90-year-old female and absence of any major symptoms at follow up, suggest that conservative management is an acceptable approach while treating patients with this condition. It should be noted however, that therapy should be guided by the patient’s clinical presentation and at the discretion of the physician managing the patient. Our patient continued to do well on conservative medical therapy, at 3, 6 and 12 months follow up visits.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cohen P, O'Gara PT. Coronary artery aneurysms: a review of the natural history, pathophysiology, and management. Cardiol Rev 2008;16:301-4. [Crossref] [PubMed]
- Lima B, Varma SK, Lowe JE. Nonsurgical management of left main coronary artery aneurysms: report of 2 cases and review of the literature. Tex Heart Inst J 2006;33:376-9. [PubMed]
- Marla R, Ebel R, Crosby M, et al. Multiple giant coronary artery aneurysms. Tex Heart Inst J 2009;36:244-6. [PubMed]
- Boyer N, Gupta R, Schevchuck A, et al. Coronary artery aneurysms in acute coronary syndrome: case series, review, and proposed management strategy. J Invasive Cardiol 2014;26:283-90. [PubMed]
- Baman TS, Cole JH, Devireddy CM, et al. Risk factors and outcomes in patients with coronary artery aneurysms. Am J Cardiol 2004;93:1549-51. [Crossref] [PubMed]
- Demopoulos VP, Olympios CD, Fakiolas CN, et al. The natural history of aneurysmal coronary artery disease. Heart 1997;78:136-41. [Crossref] [PubMed]
- Prospective randomized study of coronary artery bypass surgery in stable angina pectoris: a progress report on survival. Circulation 1982;65:67-71. [Crossref] [PubMed]
- Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation 1983;67:134-8. [Crossref] [PubMed]


