Barriers and enablers to proper diabetic foot care amongst community dwellers in an Asian population: a qualitative study
Introduction
The global prevalence of diabetic patients with foot ulcers is as high as 25% (1). The lifetime risk of a diabetic patient developing a foot ulcer is 15% (2). The burden of diabetic foot conditions is expected to rise as a result of the rising global prevalence of patients with diabetes mellitus (3). This rise is due to numerous factors, which include our ageing populations and an increasing population of people living sedentary lifestyles. However, not all elderly patients or individuals with sedentary lifestyles sustain diabetic foot conditions. Studies have shown that proper diabetic control and proper foot care are vital for the overall prevention of diabetic foot conditions such as neuropathic ulcers, Charcot’s arthropathy and lower limb infections (such as cellulitis, osteomyelitis and septic arthritis) (4-8). Improper prevention of diabetic foot conditions can result in significant morbidity, decreased function and quality of life (9). If the condition is severe enough, the pathology involved may require radical surgical management in the form of amputations (10,11) and can be life threatening (12,13). Proper foot care is an essential component in both the prevention and management of diabetic foot disease. The importance of self-care behaviors and practices being at the core of diabetic foot management was reinforced in a consensus statement issued by a multi-disciplinary panel and published in 2011 (14). To increase the extent of proper foot care in the diabetic, barriers to proper diabetic foot care should decrease and the enablers increase—the first step is to identify these factors.
In this study, we aim to identify the barriers and enablers to proper diabetic foot care specifically within a multi-ethnic Asian population. It is hoped that these findings will provide a better understanding of the factors which affect the eventual decision making of patients towards proper or improper diabetic foot care.
It was felt that the breadth of views obtained from interviewing healthcare professionals would be greater than interviewing individual patients as healthcare professionals would bring up belief systems and practices of various groups of patients over their years of practice. Furthermore, although there still remains insufficient information regarding factors which affect proper foot care within the current literature, the majority of data that does exist focusses on patient experiences from patient interviews (15-17). There are only few studies which have taken into consideration observations by healthcare professionals (18,19) of patient beliefs and practices in the form of qualitative data. As such, obtaining this data from a multi-disciplinary group of healthcare professionals could contribute usefully to our understanding of the problem.
Methods
Ethical approval
Ethics approval was obtained for this study on 22nd April 2015 via the Singapore National Healthcare Group (NHG) Domain-Specific Review Board (DSRB) (DSRB Reference Code: DSRB 2014/00959). Further details regarding the ethical approval process can be obtained from the corresponding author upon request.
Selection of participants
A qualitative study on 17 healthcare professionals from different sub-specialties, who care for diabetic patients was performed. Healthcare professionals were identified via snowball sampling, in which interviewed healthcare professionals recommended other professionals to be interviewed. A variety of healthcare professionals practicing either within the public and private hospitals were interviewed, including doctors, nurses and podiatrists. We only included healthcare professionals who had a minimum of five years of experience in caring for diabetic patients. All participants were contacted individually.
Interview process
Interviews were performed individually in the form of Key Informant Interviews (KIIs). With the permission of participants, we digitally audio recorded the interviews of 15 participants. For the 2 participants who did not allow for digital audio recording, only field notes were taken during the interview for analysis purposes. Informed consent was obtained before the start of the interview. Both the informed consent taking process and interview were performed in a private and quiet area where participants were able to share their views and observations openly and clarify any of their thoughts and doubts.
The interviews were performed via a one-off semi-structured interview using the phenomenological methodology by three co-investigators (CA, AC and AS). AC and AS have had formal training in qualitative interviewing by the Saw Swee Hock School of Public Health. All interviewers have had previous experiences in qualitative studies. An interview guide was designed to keep interviews as consistent as possible, with potential to explore discussion points deeper when necessary based on themes brought up by participants. The general structure of the interview guide can be found in Table 1. The interview guide was designed to identify the barriers and enablers for proper diabetic foot care of patients, with care to differentiate such factors among diabetic patients without and with foot complications. Field notes were penned down during all the interviews. These notes supplemented the recorded interviews.

Full table
Data analysis
All recorded interviews were transcribed at verbatim. All interviews were thematically coded and analyzed by two investigators (AC and AS) in a structured manner, classifying subthemes into themes. The themes were compiled and analyzed further. This resulted in the emergence of major categorical themes regarding barriers and enablers to proper foot care of diabetes patients in the community setting. These themes were further analyzed in the context of the narratives brought up to understand the overall relationship of identified key points throughout the interviews.
Results
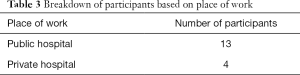
A total of 17 participants were recruited from both the public and private hospitals. Participants selected were from various disciplines, to obtain a sufficiently broad range of viewpoints regarding the various factors which influence proper care of diabetic feet within every point along the care pathway. Only participants who had at least five years of experience caring for diabetic patients were included in the study. The breakdown of participants can be found in Tables 2 and 3. Out of the medical doctors interviewed, there were 2 orthopaedic surgeons, 2 vascular surgeons and 2 endocrinologists. The nurses interviewed consisted of 4 diabetic nurse educators, 2 wound nurses, 1 vascular nurse, 1 advanced practicing nurse (diabetes care), 1 ward nurse, 1 diabetic case manager and 1 podiatrist. Thirteen participants were working in public healthcare institutions, whilst the remaining 4 participants were working in private institutions.

Full table
Full table
Overall framework
We observed certain common factors from our interviews. We initially designed our interview to elicit differences in factors affecting eventual diabetic foot care when comparing diabetic patients without foot complications and diabetic patients with foot complications. However, upon analysis of our results, we noted that the factors obtained in both groups were generally similar. Thus, we have generalized the factors to affect eventual foot care for diabetic patients with and without foot complications.
Firstly, we noted that the eventual extent of the perception of proper or improper foot care of patients by the healthcare professionals were dependent on numerous preceding factors, of which a skeletal diagram of the relationship between the major factors can be found in Figure 1. Secondly, only a few patients were observed to have completely proper or completely improper foot care practices. The majority of patients had a mixture of proper and improper foot care practices. The eventual extent and quality of care a patient had for his or her foot could potentially affect the outcome of the diabetic foot disease being managed. The composition of proper and improper foot care practices were thought by the interviewees to be dependent on belief states of patients, which were determined by the extent and quality of knowledge patients had.
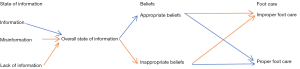
The concept of knowledge was brought up in the interviews with the emphasis of analyzing it from two perspectives. Firstly, the extent of knowledge patients had regarding diabetes, and related matters, such as an understanding of the disease state, potential complications, disease severity, ideal self-care practices and health screening guidelines, was frequently brought up. In general, the interviewees’ experience was that the majority of patients had some form of knowledge and understanding regarding diabetes and its related matters. This information was obtained from various sources, such as healthcare professionals, the internet, print media, friends and relatives. However, certain participants observed that the majority of individuals still had gaps in their knowledge regarding diabetes and related matters. Anecdotally, the presence of major gaps in knowledge was noted to be detrimental to the overall care and eventual outcome of such patients. Furthermore, the quality of information is vital. Numerous patients had some form of misinformation which resulted in them behaving in inappropriate ways. Eventually, this would possibly negatively affect the overall state of information which could result in inappropriate beliefs and thus, improper foot care practices. For instance, misinformation that alternative therapy may be useful for care of diabetic foot conditions could lead to inappropriate management and subsequent exacerbation of the foot condition. This may be despite the fact that the same patients may be well versed with information regarding diabetes and related matters. As such, both the quality and extent of knowledge which a patient possesses has to be considered when understanding the overall state of information a patient may have regarding diabetes and related matters.
“ …I have had a few patients who have gone to see traditional practitioners presenting with just swelling and redness, but along with an underlying Charcot’s foot. In certain cultural traditional beliefs, swelling is bad. It is not just a physiological response to injury. So they have moxibustion, cupping, some forms of acupuncture into a diabetic foot with swelling and Charcot’s arthropathy…I have seen infections and ulcers from practices such as that because the traditional practitioner does not necessarily know that the patient has either diabetes or end organ disease. So an acupuncture needle is enough to cause a big problem in a Charcot’s foot…Just because a foot is swollen does not mean that they have to go and get it massaged or ‘moxibusted’ as it can cause a burn, which can cause an ulceration which there on leads to an amputation.” Orthopaedic surgeon 2, interview 4.
The eventual overall state of information determines the composition of appropriate and inappropriate beliefs a patient may have. Commonly, it is assumed that good knowledge equates to proper foot care practices. However, there are various situations in which a good overall state of knowledge does not result in an optimal state of proper foot care. To a large extent, this is because a good overall state of knowledge does not always lead to largely appropriate beliefs. In fact, a patient with a good overall state of knowledge may potentially have a large proportion of inappropriate beliefs. Factors resulting in these observations will be displayed in the later part of the results section in the form of predisposing and precipitating factors. As such, a proper understanding of belief systems of patients is vital in understanding the background of patients which contributes to the extent of proper foot care practiced by that patient. Examples of appropriate belief systems included realizations that diabetic foot complications were potentially severe, perceptions that proper diabetic care and regular follow ups were vital. Examples of inappropriate belief systems included placing health as a lower priority as compared to other factors such as work commitments, underestimation of the severity of diabetes and its complications and having a lack of trust in the healthcare system.
“Patients can understand but it depends on whether they want to change or not. Some of them think that even with late complications, coming here (hospital) is a waste of time.” Diabetes nurse educator 1, interview 5.
“I think the first step is to have the proper beliefs and proper motivation, then it comes to whether or not that person is diligent. Unless it is a habit it will not get attended to, because we have so many things. We might mean well, it doesn’t mean that we purposely put it aside or we ignore it, but because of so many other things it gets pushed to the backburner until something crops up.” Podiatrist 1, interview 15.
In all, whilst navigating through the framework above, it is vital to appreciate that the path leading to the eventual composition of proper and improper foot care has to be analyzed both as a whole and based on its individual components to deeper identify the potential factors which may be resulting in an suboptimal level of foot care. There are also various factors which influence the direction taken by a patient through this pathway, which can be classified as predisposing and precipitating factors.
Factors of influence
Throughout the interviews, numerous points were brought out suggesting that there were factors which influenced the overall state of knowledge and belief systems of patients. There was even suggestion that the overall state of information and eventual belief systems were not pure determinants of the extent of proper foot care practiced by a patient. We grouped these factors of influence into broad categories, and were eventually classified as predisposing and precipitating factors which influenced the path which patients moved along through the overall framework in Figure 1.
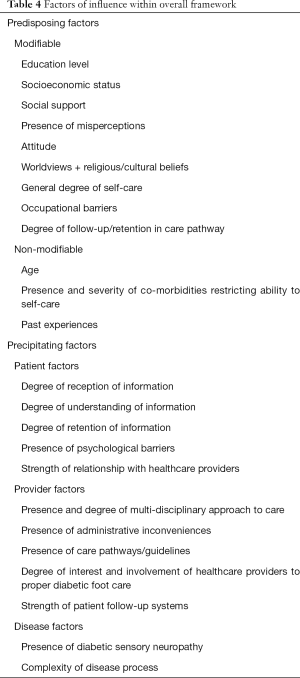
Predisposing factors refer to factors which increase the vulnerability of patients to be directed along a certain way through the overall framework in Figure 1. These predisposing factors dictate the background state of the patient, leading to observed reactions based on given situations. We categorized these factors into modifiable and non-modifiable factors with the intention of increasing the convenience of clinical practitioners in identifying factors which could be adjusted throughout the care of the patient. A lower education level, lower socioeconomic status, lower level of social support (whether by family members or other forms of caregivers), higher presence of misperceptions, poor attitude, non-synergistic worldviews, religious or cultural beliefs, lower general degree of self-care, higher level of occupational barriers (such as job commitments and job requirements) and lower degree of follow-up or retention of care within the healthcare system were considered to be modifiable predisposing barriers to eventual proper diabetic foot care. An older age, higher presence and increased severity of co-morbidities restricting ability to self-care and non-synergistic past experiences were considered non-modifiable predisposing barriers to proper diabetic foot care. On the other hand, a higher education level, higher socioeconomic status, better social support structure, lower presence of misperceptions, better attitude, synergistic worldviews, proper self-care, low level of occupational barriers and high degree of follow-up or retention within the healthcare system were considered modifiable predisposing enablers to proper diabetic foot care. A younger age, and decreased presence, with lower severity of co-morbidities restricting ability to self-care and synergistic past experiences were considered non-modifiable predisposing enablers to proper diabetic foot care.
“..patients from higher socioeconomic groups tend to be better read, more knowledgeable, more willing to ask questions and have more insight into the disease at hand. From my point of view, it is easier in that sense to get your point across and try to manage these patients.” Vascular surgeon 1, interview 2.
“I have to say the hardest part of diabetic foot management is foot care. Patients have to check their feet regularly every day. Sometimes their vision is not good. As such, they won't be able to pick up problems properly. They may have neuropathy so they may not be able to feel wounds.” Vascular nurse, interview 9.
“Generally most of them are compliant and can follow instruction. They can take care of themselves. However, there are a small number of patients who maybe have knowledge but do not apply it sometimes because of financial or poor support from family. As such, some of them are not compliant to medicine, not following up with doctors regularly.” Diabetes nurse educator 3, interview 12.
Precipitating factors, on the other hand, refer to factors which exist only due to interaction with either healthcare providers or their disease state, in this case, diabetic foot conditions. Precipitating factors are the factors, which initiate the eventual movement of patients along the overall framework in Figure 1. We categorized these factors into patient, provider and disease factors so as to simplify understanding of the interactions which occur amongst patients, providers and disease states. These precipitating factors either contribute to or are a result of particular interactions. A lower degree of reception of information, lower degree of understanding of information, lower degree of retention of information, large presence of psychological barriers and weak relationship between patient and healthcare providers were considered precipitating patient barriers to proper diabetic foot care based on our interviews. An absence or low degree of multi-disciplinary approach to diabetic care within healthcare institutions, high degree of administrative inconveniences, absence of proper care pathways or guidelines, poor interest and involvement of healthcare providers to proper diabetic foot care and poor patient follow-up systems were considered precipitating provider barriers to proper diabetic foot care. The presence of diabetic sensory neuropathy, and a perceived complexity of diabetes disease process were precipitating disease state barriers. On the other hand, a high degree of reception of information, high degree of understanding of information, high degree of retention of information, low degree of psychological barriers and strong relationship with healthcare providers served as precipitating patient enablers to proper diabetic foot care. A high degree of multi-disciplinary care for diabetic foot patients, low degree of administrative inconveniences, strong presence of care pathways and guidelines, high degree of interest and involvement of healthcare providers to proper diabetic foot care and strong patient follow-up systems serve as precipitating provider enablers. The absence of diabetic sensory neuropathy and absence of perceived complexity of disease process both are precipitating disease state enablers to proper diabetic foot care.
“…changing beliefs and false perceptions is what we all try to do, but it requires a lot of time, effort and indoctrination. But if we just see them once in three months, and try to tell them these things, it may not be enough. Because for that three months, they are left on their own. You have to really spend some time with them.” Orthopaedic surgeon 1, interview 1.
“I think we are quite lucky in this hospital because we have a team that is interested. When we say coordinated care, we say patients usually come in through either an orthopaedic consultant or a vascular consultant. So when they come in, we are in charge of coordinating the care. We are in charge of coordinating the podiatrists, diabetologists, nurses, wound care nurses on the ward. And in that way the patient gets a multidisciplinary service where they may not elsewhere. I think that is probably the best chance these patients have of salvage or at least avoiding further problems. So by the time a patient has got to that stage, that is what the patient needs. You need multidisciplinary care.” Orthopaedic surgeon 2, interview 4.
In all, the individual components of the overall framework in Figure 1 have to be analyzed in tandem with the factors of influence to better appreciate the reasoning for eventual extent of proper foot care practiced by a patient. At times, the root cause for improper foot care may not be particular components of the overall framework. Instead, the root cause may be either a predisposing or precipitating factor. In such cases, the objective of the healthcare professional is to target such factors of influence, as stated in Table 4, to influence the eventual extent of foot care by a patient.
Full table
Discussion
Foot conditions are highly prevalent amongst diabetic patients. Globally the lifetime risk of a diabetic patient developing a foot ulcer is 15% (2). They potentially result in decreased function and quality of life for patients. They result in either loss of limb and loss of life and diabetes is by far the leading cause of amputation in the developed world (20). Such negative outcomes are preventable (21). To a large extent, these negative outcomes occur due to late diagnosis and improper diabetic foot care. In fact, the majority of people with diabetes do not receive or practice the foot care recommended by current guidelines (22).
The aim of this study was to identify the barriers and enablers to proper foot care practices amongst diabetic patients. Through our study findings, we described an overall framework to understand the behavior which underpins the eventual extent of proper foot care practices of diabetic patients. Diabetic patients generally have a mixture of proper and improper diabetic foot care practices. The extent of proper foot care practices is dependent on several factors. Within the overall framework were individual components as well as factors of influence. Factors of influence were further classified into predisposing and precipitating factors. Any of the above mentioned factors could either serve as barriers or enablers to proper foot care practices.
This is one of the few studies to have studied factors which affect proper diabetic foot care practices based on observations of a multi-disciplinary group of healthcare professionals. Our results corroborate findings currently present within the literature. For instance, our findings are consistent in identifying limited knowledge and poor understanding of disease state and related matters as a barrier to eventual proper foot care (23,24). Conversely, the presence of strong education programs serves as enablers to proper diabetic foot care (25). Similarly, a higher education level has been shown to be positively associated with better foot care knowledge (26-30). We also noted that the overall state of knowledge is a poor determinant of eventual behavior and foot care practices (31,32). In fact, belief systems play a far greater role than knowledge states in eventually influencing practices, as suggested by Leventhal’s Common Sense Model (CSM) (33), which has been extensively used in the study of self-management behaviors of people with diabetes (34). In general, the CSM suggests that how people interact with and manage their illness is highly dependent on their disease and related matters. Other conclusions such as the importance of strong relationships between healthcare providers, the influence of background socioeconomic status as well as attitudes of patients (35) and a need to decrease misinformation and misperceptions so as to increase proper diabetic foot care were also brought up similarly in other studies.
We suggest a structured framework to understand the background of a patient which results in the eventual extent of proper foot care amongst diabetic patients. We also suggest a classification of factors which influence the various components of this framework into predisposing and precipitating factors. The idea that beliefs are influenced by overall knowledge states is not new. It has been reported previously in other qualitative studies on diabetic foot care as well as behavioral studies with regard to other disease states and healthcare systems. Regardless, a diagrammatic representation of the relationship between knowledge, beliefs and eventual practices, together with the various factors which influence each of these components serve as a backbone to further appreciation of the background of patients in a structured method. Furthermore, such a framework serves as scaffold for further research to build upon as well as for solutions to be designed to holistically tackle the challenge of improper foot care amongst diabetic patients.
We acknowledge that there are certain limitations to our study. Firstly, we only interviewed healthcare professionals. We did not include patients within our study population. This resulted in responder bias within our study. However, it was the intention of this study to only include healthcare professionals within this study so as to compare their opinions with viewpoints of patients currently present within the literature. As much as possible, we attempted to include a wide variety of healthcare professionals which are usually present in the multi-disciplinary teams which cares for diabetic foot patients. However, we did not include all allied health members of the multi-disciplinary team, such as physiotherapists and occupational therapists.
Conclusions
In conclusion, we note that there is an overall pattern to understand the extent of proper foot care practices of diabetic patients. This is influenced by components such as the overall state of knowledge and belief states of patients and these components, in turn are influenced by predisposing and precipitating factors. A careful appreciation of the factors which influence the eventual extent of proper foot care of diabetic patients needs to take into consideration all of these factors. It is hoped that with such appreciation of factors, the overall influence of behavior and practices of patients can be tackled in a more holistic approach. Further studies can look at further development of the above described structure as well as quantitatively defining the various components and factors which make up the described system.
Acknowledgements
We would like to acknowledge Candy Au, research coordinator within Jurong Health Services, who assisted with the administrative aspects of the study. We would also like to acknowledge the multidisciplinary diabetic foot team within Jurong Health Services for their kind support and assistance throughout the study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics approval was obtained for this study on 22nd April 2015 via the Singapore National Healthcare Group (NHG) Domain-Specific Review Board (DSRB) (DSRB Reference Code: DSRB 2014/00959) and informed consent was obtained from the participants.
References
- Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA 2005;293:217-28. [Crossref] [PubMed]
- Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, et al. The global burden of diabetic foot disease. Lancet 2005;366:1719-24. [Crossref] [PubMed]
- Wild S, Roglic G, Green A, et al. Global Prevalence of Diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047-53. [Crossref] [PubMed]
- van Netten JJ, Price PE, Lavery LA, et al. Prevention of foot ulcers in the at-risk patient with diabetes: A systematic review. Diabetes Metab Res Rev 2016;32 Suppl 1:84-98. [Crossref] [PubMed]
- Dorresteijn JA, Kriegsman DM, Assendelft WJ, et al. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev 2014;12:CD001488. [PubMed]
- Bus SA, Valk GD, van Deursen RW, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev 2008;24 Suppl 1:S162-80. [Crossref] [PubMed]
- Paton J, Bruce G, Jones R, et al. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review. J Diabetes Complications 2011;25:52-62. [Crossref] [PubMed]
- Bowling FL, Rashid ST, Boulton AJ. Preventing and treating foot complications associated with diabetes mellitus. Nat Rev Endocrinol 2015;11:606-16. [Crossref] [PubMed]
- Armstrong DG, Wrobel J, Robbins JM. Are diabetes-related wounds worse than cancer? Int Wound J 2007;4:286-7. [Crossref] [PubMed]
- Nather A, Siok Bee C, Keng Lin W, et al. Value of team approach combined with clinical pathway for diabetic foot problems: a clinical evaluation. Diabet Foot Ankle 2010.1. [PubMed]
- Wong KL, Nather A, Chanyarungrojn AP, et al. Clinical Outcomes of Ray Amputation in Diabetic Foot Patients. Ann Acad Med Singapore 2014;43:428-32. [PubMed]
- Lavery LA, Hunt NA, Ndip A, et al. Impact of chronic kidney disease on survival after amputation in individuals with diabetes. Diabetes Care 2010;33:2365-9. [Crossref] [PubMed]
- Buse JB, Ginsberg HN, Bakris GL, et al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American heart association and the American diabetes association. Diabetes Care 2007;30:162-72. [Crossref] [PubMed]
- McInnes A, Jeffcoate W, Vileikyte L, et al. Foot care education in patients with diabetes at low risk of complications: a consensus statement. Diabet Med 2011;28:162-7. [Crossref] [PubMed]
- Hjelm K, Beebwa E. The influence of beliefs about health and illness on foot care in Ugandan persons with diabetic foot ulcers. Open Nurs J 2013;7:123-32. [Crossref] [PubMed]
- Hjelm K, Nambozi G. Beliefs about health and illness: a comparison between Ugandan men and women living with Diabetes Mellitus. Int Nurs Rev 2008;55:434-41. [Crossref] [PubMed]
- Hjelm K, Mufunda E. Zimbabwean Diabetics’ beliefs about health and illness: an interview study. BMC Int Health Hum Rights 2010;10:7. [Crossref] [PubMed]
- Guell C, Unwin N. Barriers to diabetic foot care in a developing country with a high incidence of diabetes related amputations: an exploratory qualitative interview study. BMC Health Serv Res 2015;15:377. [Crossref] [PubMed]
- Aliasgharpour M, Nayeri N. The care process of diabetic foot ulcer patients: A qualitative study in Iran. J Diabetes Metab Disord 2012;11.-27 [Crossref] [PubMed]
- The Diabetes Control and Complications Trail Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977-86. [Crossref] [PubMed]
- Morey-Vargas OL, Smith SA. BE. SMART: strategies for foot care and prevention of foot complications in patients with diabetes. Prosthet Orthot Int 2015;39:48-60. [Crossref] [PubMed]
- Barshes NR, Sigireddi M, Wrobel JS, et al. The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabet Foot Ankle 2013.4. [PubMed]
- Searle A, Gale L, Campbell R, et al. Reducing the burden of chronic wounds: prevention and management of the diabetic foot in the context of clinical guidelines. J Health Serv Res Policy 2008;13 Suppl 3:82-91. [Crossref] [PubMed]
- Gale L, Vedhara K, Searle A, et al. Patients’ perspectives on foot complications in type 2 diabetes: a qualitative study. Br J Gen Pract 2008;58:555-63. [Crossref] [PubMed]
- Delea S, Buckley C, Hanrahan A, et al. Management of diabetic foot disease and amputation in the Irish health system: A qualitative study of patients’ attitudes and experiences with health services. BMC Health Serv Res 2015;15:251. [Crossref] [PubMed]
- Khamseh ME, Vatankhah N, Baradaran HR. Knowledge and practice of foot care in Iranian people with type 2 diabetes. Int Wound J 2007;4:298-302. [Crossref] [PubMed]
- Desalu OO, Salawu FK, Jimoh AK, et al. Diabetic foot care: self reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J 2011;45:60-5. [Crossref] [PubMed]
- Hasnain S, Sheikh NH. Knowledge and practices regarding foot care in diabetic patients visiting diabetic clinic in Jinnah Hospital, Lahore. J Pak Med Assoc 2009;59:687-90. [PubMed]
- Salmani N, Hosseini SV. Foot Self Care in Diabetic Patients. IJDO 2010;2:37-40.
- Viswanathan V, Shobhana R, Snehalatha C, et al. Need for education on foot care in diabetic patients in India. J Assoc Physicians India 1999;47:1083-5. [PubMed]
- Gabbay RA, Kaul S, Ulbrecht J, et al. Motivational interviewing by podiatric physicians a method for improving patient self-care of the diabetic foot. J Am Podiatr Med Assoc 2011;101:78-84. [Crossref] [PubMed]
- Aljasem LI, Peyrot M, Wissow L, et al. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ 2001;27:393-404. [Crossref] [PubMed]
- Leventhal H, Benyamini Y, Brownlee S, et al. Illness representations: theoretical foundations. In: Petrie KJ, Weinman JA. editors. Perceptions of health and illness: current research and applications. Amsterdam: Harwood Academic Publishers, 1997:19-45.
- Hampson SE. Illness representations and the self-management of diabetes. In: Petrie KJ, Weinman JA. editors. Perceptions of health and illness. Amsterdam: Harwood Academic, 1997:323-47.
- Egede LE, Bonadonna RJ. Diabetes self-management in African Americans: an exploration of the role of fatalism. Diabetes Educ 2003;29:105-15. [Crossref] [PubMed]


