Myocardial bridging with left ventricular hypertrophy presenting as Wellens pattern
Introduction
The course of epicardial coronary arteries into a muscular tunnel under a bridge of myocardium is known as myocardial bridging (MB). This could be a benign anomaly, nevertheless, it could have a great impact on the quality of life in the setting of severe anginal symptoms. The clinical presentation and diagnosis could be challenging in those patients. The treatment options start from simple medical therapy to surgical intervention in refractory cases, the role of percutaneous coronary intervention (PCI) is limited in MB. We are describing a case of severe MB presenting as Wellens pattern with underlying left ventricular hypertrophy (LVH).
Case presentation
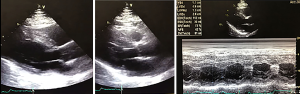
A 45-year-old Hispanic male presented to the emergency department for new onset of chest pain. The pain was described as an intermittent retrosternal chest heaviness, 7 out of 10 in severity, radiating to left arm, which started 20 minutes prior to arrival while the patient was watching TV, was relieved by nitroglycerine and rest, and was associated with shortness of breath. There was no associated orthopnea, paroxysmal nocturnal dyspnoea (PND) or lower limb edema, palpitations, change in mental status, nausea, vomiting or back pain. The patient stated that he had a similar episode 3 days earlier when he was shoveling the snow but was associated with sweating and shortness of breath which resolved at rest. He has been treated for essential hypertension during the last 2 years with losartan 50 mg, hydrochlorothiazide (HCTZ) 12.5 mg, atenolol 100 mg and statins for dyslipidemia. He is a nonsmoker and denied any illicit drug use including cocaine. His grandfather sustained an acute myocardial infarction (MI) in his 50s. On clinical examination was unremarkable except for elevated blood pressure of 160/90 in both arms and body mass index (BMI) of 42. A chest X-ray was normal and 12 leads electrocardiogram (EKG) obtained shows deep asymmetric T wave inversion involving the anterolateral and inferior leads which had biphasic pattern on prior EKG (Figures 1,2). Cardiac marker first set were negative. Echocardiogram (Figure 3) showed no regional wall motion abnormalities, with preserved left ventricular (LV) ejection fraction in addition to moderate LVH. In the setting of typical presenting symptoms and EKG changes concerning of Wellens syndrome, coronary angiogram was done which showed severe bridging of mid left anterior descending (LAD) in addition to ectasia of right coronary artery (RCA) and left circumflex (LCX) (Figures 4,5). The decision was made to proceed with medical treatment including aggressive blood pressure control and risk factor modification, in addition to beta blockers, avoidance of nitrates, and antiplatelet therapy. The patient was discharged from the hospital without complications, repeat EKG showed resolution of ST-T changes, the plan was for outpatient follow-up for possible need of surgical intervention if symptoms are refractory.



Discussion
MB is a relatively frequent finding in postmortem ranging from 15% to 85% of cases (1). However, functional MB is less observed on angiography (0.5% to 2.5%) (2), although detection can increase up to 16% if provocation tests are used (3,4).
MB is defined as a segment of a coronary artery that takes a “tunneled” intramuscular course under a bridge of overlying myocardium, resulting in systolic compression of a coronary artery. The large discrepancy in reported prevalence clearly maybe due to the lack of true gold standard test for the diagnosis of bridging.
Certain population, namely hypertrophic cardiomyopathy (HCM) patients has higher prevalence than general population with rates up to 30% (5). MB has been associated with increased risk of sudden cardiac death (SCD) in pediatric population with HCM. Although Sorajja et al. demonstrated not increased risk of cardiac death or SCD in adult patients with HCM (6).
The most frequent coronary artery involved is the LAD at the middle segment on coronary angiography. In other coronary computed tomography angiography (CTA) case series concluded that the RCA and LCX artery involvement at similar rates (7). In addition, secondary arteries such as diagonal (18%) and marginal (40%) branches are also commonly involved (8). There is difference in prevalence of bridging by gender which is higher in male (7,8).
MB presents with a variety of symptoms varying from angina, atypical chest pain, arrhythmia to sudden death, thus there is no consensus for the clinical diagnosis of this entity without visualization of the coronary arteries.
Myocardial blood flow (MBF) occurs predominantly during diastole while coronary compression of the myocardial bridge is at systole. However, clinical invasive and noninvasive diagnostic tools such as CTA, positron emission tomography (PET) intravascular ultrasound and intracoronary Doppler and percutaneous coronary angiography have contributed greatly to our understanding of the anatomic, hemodynamic, and pathophysiological consequences of systolic compression, which extends to mid/late diastole causing persistent diastolic luminal narrowing with increases both the blood flow velocities and retrograde flow, and a reduced flow reserve. Also, it has been postulated that accelerated atherosclerosis of the proximal segment of coronary artery before the bridged segment contribute to myocardial supply-demand mismatch in patients with MB (8-10).
Although Konen et al. conducted a prospective study with a total sample of 100 patients with intermediate pretest probability of coronary artery disease, and MB identified using CTA, with combination of PET and invasive coronary angiography to identify the systolic compression of coronary artery and measure atherosclerotic burden in coronary artery. Plaque morphology proximal to MB was comparable to other vessels. Therefore, according to this finding, MB is not associated with more advanced atherosclerotic disease (11).
Medical management should be considered in patient like our patient presenting with angina and ischemia induced on stress test or demonstrated systolic vasoconstriction of the intramural coronary artery more than 70% or diastolic vasoconstriction of more than 35% on coronary angiography (12), beta-blockers still first-line therapy which will decrease the heart rate, that in turn increases the diastolic coronary filling period, and decreasing contractility, although there has not been any randomized clinical evaluating the long-term efficacy of beta blockers (13,14). Calcium channel blockers can be used as a second-line (15) or in combination with beta-blockers that may have vasodilator effect segments proximal to the tunneled segment. Nitrates are contraindicated; it has been shown to accentuate systolic compression of bridged segments (16).
Nevertheless, if medical treatment is unsuccessful stent implantation or surgery are therapeutic alternatives however, case reports on stent insertion reported raising the concerns of perforation during stent deployment (17-20), in-stent restenosis (20), stent fracture (21,22), aneurysm formation (22), and stent thrombosis (18) thus avoiding there use in MB is preferable. On the other hand, surgical options for MB include surgical myotomy and coronary artery bypass graft surgery with anastomosis of the left internal mammary artery to the LAD artery can be contemplated for refractory cases. Further research is required to better define the patient population that would derive the greatest benefit from surgical and percutaneous intervention (23,24).
Conclusions
The clinical presentation of MB is variable, thus an appropriate diagnostic test should be chosen with coronary angiography being the gold standard. The cornerstone of treatment of MB is medical with beta blockers and calcium channel blockers being the regimen of choice. The role of PCI is very limited in MB due to the adverse outcome reported in literature and the surgery is reserved for cases refractory to medical therapy, MB is more commonly described in HCM patients and presentation as Wellens pattern is rare in medical literature.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Möhlenkamp S, Hort W, Ge J, et al. Update on myocardial bridging. Circulation 2002;106:2616-22. [Crossref] [PubMed]
- Kim SY, Seo JB, Do KH, et al. Coronary artery anomalies: classification and ECG-gated multi-detector row CT findings with angiographic correlation. Radiographics 2006;26:317-33; discussion 333-4. [Crossref] [PubMed]
- Corban MT, Hung OY, Eshtehardi P, et al. Myocardial bridging: contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. J Am Coll Cardiol 2014;63:2346-55. [Crossref] [PubMed]
- Kim PJ, Hur G, Kim SY, et al. Frequency of myocardial bridges and dynamic compression of epicardial coronary arteries: a comparison between computed tomography and invasive coronary angiography. Circulation 2009;119:1408-16. [Crossref] [PubMed]
- Alegria JR, Herrmann J, Holmes DR Jr, et al. Myocardial bridging. Eur Heart J 2005;26:1159-68. [Crossref] [PubMed]
- Sorajja P, Ommen SR, Nishimura RA, et al. Myocardial bridging in adult patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2003;42:889-94. [Crossref] [PubMed]
- Jodocy D, Aglan I, Friedrich G, et al. Left anterior descending coronary artery myocardial bridging by multislice computed tomography: correlation with clinical findings. Eur J Radiol 2010;73:89-95. [Crossref] [PubMed]
- Uusitalo V, Saraste A, Pietilä M, et al. The Functional Effects of Intramural Course of Coronary Arteries and its Relation to Coronary Atherosclerosis. JACC Cardiovasc Imaging 2015;8:697-704. [Crossref] [PubMed]
- Herrmann J, Higano ST, Lenon RJ, et al. Myocardial bridging is associated with alteration in coronary vasoreactivity. Eur Heart J 2004;25:2134-42. [Crossref] [PubMed]
- Samady H, Eshtehardi P, McDaniel MC, et al. Coronary artery wall shear stress is associated with progression and transformation of atherosclerotic plaque and arterial remodeling in patients with coronary artery disease. Circulation 2011;124:779-88. [Crossref] [PubMed]
- Konen E, Goitein O, Sternik L, et al. The prevalence and anatomical patterns of intramuscular coronary arteries: a coronary computed tomography angiographic study. J Am Coll Cardiol 2007;49:587-93. [Crossref] [PubMed]
- Bourassa MG, Butnaru A, Lespérance J, et al. Symptomatic myocardial bridges: overview of ischemic mechanisms and current diagnostic and treatment strategies. J Am Coll Cardiol 2003;41:351-9. [Crossref] [PubMed]
- Schwarz ER, Klues HG, vom Dahl J, et al. Functional, angiographic and intracoronary Doppler flow characteristics in symptomatic patients with myocardial bridging: effect of short-term intravenous beta-blocker medication. J Am Coll Cardiol 1996;27:1637-45. [Crossref] [PubMed]
- Nair CK, Dang B, Heintz MH, et al. Myocardial bridges: effect of propranolol on systolic compression. Can J Cardiol 1986;2:218-21. [PubMed]
- Alessandri N, Dei Giudici A, De Angelis S, et al. Efficacy of calcium channel blockers in the treatment of the myocardial bridging: a pilot study. Eur Rev Med Pharmacol Sci 2012;16:829-34. [PubMed]
- Ishimori T, Raizner AE, Chahine RA, et al. Myocardial bridges in man: clinical correlations and angiographic accentuation with nitroglycerin. Cathet Cardiovasc Diagn 1977;3:59-65. [Crossref] [PubMed]
- Hering D, Horstkotte D, Schwimmbeck P, et al. Acute myocardial infarct caused by a muscle bridge of the anterior interventricular ramus: complicated course with vascular perforation after stent implantation. Z Kardiol 1997;86:630-8. [Crossref] [PubMed]
- Haager PK, Schwarz ER, vom Dahl J, et al. Long term angiographic and clinical follow up in patients with stent implantation for symptomatic myocardial bridging. Heart 2000;84:403-8. [Crossref] [PubMed]
- Zhang M, Kang WC, Moon CI, et al. Coronary artery perforation following implantation of a drug-eluting stent rescued by deployment of a covered stent in symptomatic myocardial bridging. Korean Circ J 2010;40:148-51. [Crossref] [PubMed]
- Broderick TM, Kereiakes DJ, Whang DD, et al. Myocardial Bridging May Predispose to Coronary Perforation During Rotational Atherectomy. J Invasive Cardiol 1996;8:161-3. [PubMed]
- Kunamneni PB, Rajdev S, Krishnan P, et al. Outcome of intracoronary stenting after failed maximal medical therapy in patients with symptomatic myocardial bridge. Catheter Cardiovasc Interv 2008;71:185-90. [Crossref] [PubMed]
- Srinivasan M, Prasad A. Metal fatigue in myocardial bridges: stent fracture limits the efficacy of drug-eluting stents. J Invasive Cardiol 2011;23:E150-2. [PubMed]
- Sun X, Chen H, Xia L, et al. Coronary artery bypass grafting for myocardial bridges of the left anterior descending artery. J Card Surg 2012;27:405-7. [Crossref] [PubMed]
- Betriu A, Tubau J, Sanz G, et al. Relief of angina by periarterial muscle resection of myocardial bridges. Am Heart J 1980;100:223-6. [Crossref] [PubMed]



