A pilot study evaluating biomarker development for drug-induced chronic eczematous eruptions of aging individuals
Introduction
Chronic eczematous eruptions of aging individuals (CEEA) (i.e., ≥50 years) has been a neglected area of clinical research in dermatology. CEEA can result from aging-onset atopic dermatitis, widespread contact dermatitis, cutaneous T cell lymphoma, prodromal/non-bullous pemphigoid, autoeczematization reaction/ID reaction and eczematous drug eruptions. Such eczematous drug eruptions are thought to result from T cell-mediated delayed hypersensitivity reactions (DHR). Drug-induced DHR have been shown to account for approximately 15% of all adverse drug reactions and are of major medical significance (1).
Several aspects of drug-induced CEEA present considerable challenges to clinicians. Aging individuals are typically taking multiple prescription medications, over-the-counter medications, vitamins, and supplements on a daily basis. Thus, when a drug eruption develops in this setting, there is always uncertainty as to its specific cause. In addition, drug-induced CEEA can develop in patients who have been taking the triggering medication for years. Due to this potential delay in development of CEEA, patients and their healthcare providers often do not recognize a causal relationship between taking a medication and the development of a drug-induced CEEA.
In recent work, we confirmed the prior observations by Joly et al. indicating that CEEA can result from DHR to calcium channel blocker (CCB) medications. Our studies also indicated that hydrochlorothiazide (HCTZ) can trigger CEEA (2,3).
Aging individuals being treated with CCB and/or thiazide diuretics are frequently taking other medication classes as well. Identification of the drug(s) responsible for a cutaneous adverse reaction in these patients following onset of the drug eruption poses a significant clinical challenge. The current gold standard for DHR is drug withdrawal and re-challenge, however this method is inefficient for multiple medications and carries the risk of severe clinical reactions resulting from drug withdrawal in patients. Management of drug-induced CEEA would be greatly facilitated by a biomarker for drug class-specific CEEA to identify the offending medication causing the eczematous eruption. We chose to perform a pilot study to examine the feasibility of using in vitro, drug-specific T cell proliferative responses as a biomarker for drug-induced CEEA. We had hoped to use the results of this pilot study to recruit funding for a larger systematic study of this important clinical problem.
Methods
Ethical approval was obtained from the Institutional Review Board at the University of Utah for a single center, proof of concept pilot study. The initial design of this pilot study included ten study subjects and ten matched controls. Biopsy and billing records were searched in order to recruit study subjects and controls.
Study subjects
Inclusion criteria for study subjects were: (I) age 50 or older; (II) a symmetrical eczematous eruption; (III) the eruption evolved continuously or recurrently during a period of at least 3 months before the study period; (IV) affected individuals had taken either a CCB and/or HCTZ for at least 2 months preceding the onset of the eruption; (V) skin biopsy for routine hematoxylin-eosin examination showed presence of spongiotic dermatitis with eosinophils in the inflammatory infiltrate and/or the presence of overlapping elements of other inflammatory histologic patterns; (VI) skin biopsy from direct immunofluorescence (if available) was negative for bullous pemphigoid. Exclusion criteria for study subjects were: (I) a history of atopic dermatitis; (II) leukopenia; (III) systemic immunosuppressive therapy within the 4 weeks prior to initiation of the study; (IV) congenital or acquired immunodeficiency disorders.
Controls
Control subjects were gender and age-matched (±5 years) to a respective study subject. Inclusion criteria for control subjects also included current intake of a CCB or HCTZ, with medication class matched to a respective study subject. Exclusion criteria included the same as those for the case subjects, as well as manifestation of any type of eczematous eruption.
Protocol
Eight study subjects having a history suggestive of chronic eczematous drug eruption suspected to have resulted from CCB and/or HCTZ hypersensitivity plus three control subjects were initially identified. All participants provided their written consent to participate in the study. Following enrollment, patients underwent venipuncture and drug patch testing for either CCB and/or HCTZ.
Purified formulations of HCTZ and the CCB medications were obtained from Sigma Aldrich®. Drug concentrations of 1%, 10%, and 30% in petrolatum were compounded and applied to the medial upper arms of the participants. Patch test readings were performed on day 2 and either day 4 or 5.
In vitro drug antigen-induced lymphocyte proliferation assays and multiplexed-determined cytokine/marker release assays for interferon (IFN)-γ, interleukin (IL)-1b, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12 p70, IL-13, IL-17, tumor necrosis factor (TNF-α), cytokine receptor IL-2r, and soluble CD40 ligand (sCD40L) were performed on HCTZ and/or CCB-stimulated and unstimulated cells after five days of incubation at 37 °C with 5% CO2. Purified formulations of HCTZ and amlodipine besylate were obtained from Sigma Aldrich®, St. Louis, MO and were used for cell challenge. Inhibition studies were performed on control subjects, in which drugs were titrated in two-fold dilutions in cell culture media from 500 to 15.6 ng/mL, adding 100 µL of each dilution per well based on previous studies (4,5). For the study subjects, amlodipine besylate was titrated in cell culture media from 31.25 to 1,000 ng/mL, and HCTZ was titrated from 718 to 50,000 ng/mL. Phytohemagglutinin (PHA) was included as a positive stimulation control for the lymphocyte proliferation assays. Inhibition of lymphocyte proliferation and cytokine release by the drugs themselves was determined by spiking control and patient cells with PHA alone, or PHA plus the drugs. Participants were also screened for BP230 and 180 antibodies by ELISA. Total serum IgE concentrations were determined using ImmunoCAP 1000 instrument (Phadia Uppsala Sweden) (6).
In vitro stimulation assays
Peripheral blood mononuclear cells (PBMC’s) were obtained from anticoagulated peripheral blood by Ficoll-Paque density gradient centrifugation. The cells were counted and adjusted to a concentration of 1×106/mL in RPMI 1640 medium containing 10% heat-inactivated pooled normal human serum, antibiotic/antimycotic, and L-glutamine. Cell cultures were set up in 96-well microtiter plates using 100 µL (1×105 PBMC’s/well). PBMC’s were stimulated with PHA as a positive control, and cells in medium alone as a background/endogenous stimulation control. Cells were cultured for 3 and 5 days at 37 °C with 5% carbon dioxide, after which the plates were either pulsed with titrated thymidine for lymphocyte proliferation studies or the supernatant was harvested and stored at −20 °C until cytokine studies were performed.
Multiplexed cytokine assay
A multiplexed fluorescent microsphere immunoassay system was developed in house and utilized in this study to simultaneously assess the concentrations of 14 cytokines/markers including IFN-γ, IL-1b, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12, p70, IL-13, IL-17, TNF-α, cytokine receptor IL-2r, and sCD40L in only 100 µL of tissue culture supernatant and 75 µL serum sample using optimized protocols for each sample type (7-9).
Results
A total of eight study subjects and three control subjects were enrolled. All study and control subject blood samples tested failed to demonstrate any detectable enhanced in vitro lymphocyte proliferation or cytokine release following challenge with CCBs or HCTZ, even when tested with a wide range of drug concentrations. In addition, none of the eight study subjects and three control subjects tested developed a positive patch test to CCBs and/or HCTZ. As this was a pilot study, we chose to discontinue enrolling study and control subjects given the uniformly negative T cell stimulation results. Even if positive results had been obtained with the additional study and control subjects according to initial study design, the pilot study would still have ended with negative results overall.
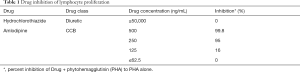
Inhibition studies were performed to determine the non-specific effects of the included drugs on in vitro cell proliferation and cytokine stimulation. The amount of inhibition due to the drug compared to PHA alone is shown in Table 1. HCTZ showed no inhibition up to 50,000 ng/mL, which is 100 times greater than peak physiologic blood concentrations. Amlodipine showed significant inhibition at a concentration of 500 ng/mL. Cytokine responses were also similarly suppressed at these same concentrations (data not shown).
Full table
One study patient tested positive for BP 180 antibody, indicating an underlying possible diagnosis of eczematous bullous pemphigoid (Table 2). However, bullous pemphigoid autoantibodies detected by solid phase immunoassay can be seen in clinical settings other than bullous pemphigoid.

Full table
Three study subjects had an elevated blood IgE level suggesting the possibility of aging onset atopic dermatitis rather than drug-induced CEEA (Table 2). However, two control subjects also had elevated levels of IgE.
Discussion
Dermatologists are frequently challenged with identifying the drug(s) responsible for adverse cutaneous reactions in patients taking multiple medications. The current gold standard for diagnosing drug eruptions in this setting is drug withdrawal and re-challenge. This method is inefficient for patients on numerous medications and increases risk in patients who may need the discontinued drug(s). Other diagnostic procedures, including patch testing, prick testing, and intracutaneous prick testing have proven to have a low sensitivity for detection of T cell-mediated drug eruptions. Lymphocyte transformation testing (LTT) and in vitro drug-induced T cell cytokine production studies have shown promise in the detection of T cell sensitization in a wide variety of drug eruptions (4,10,11). Our experimental study protocol for drug-induced CEEA was designed using the approaches that were employed in these earlier studies.
Our pilot study was designed to test the hypothesis that CEEA occurring in individuals taking CCB or HCTZ have circulating T cells that can be shown to display specific proliferative responses to the drug antigenic structures. We had also hoped to develop a clinically useful in vitro assay that could efficiently confirm a drug-specific cause for CEEA occurring in individuals on multiple medications. Unfortunately, our pilot study was unsuccessful in this regard.
The in vitro lymphocyte transformation assays and T cell cytokine release assays employed in this study were the same as those used in the Cellular and Innate Immunology Laboratory of ARUP Laboratories, a national reference laboratory. These assays are routinely standardized with the appropriate positive and negative stimuli. It was unfortunate that none of the eight CEEA study subjects displayed a positive drug patch test. Negative or positive in vitro lymphocyte transformation assays and T cell cytokine release assays would have been more informative in a patient with a positive drug patch test.
Although prior studies have shown an association between CEEA and CCB and HCTZ medications, it is plausible that these medications are not truly causative in our study (2,3). A weakness of our study was that we did not re-challenge study subjects with CCBs or HCTZ to confirm drug causation. One of our study subjects tested positive for bullous pemphigoid autoantibodies, raising the possibility that the chronic eczematous eruption in this setting was not caused by an eczematous drug eruption. However, as previously noted, circulating bullous pemphigoid autoantibodies detected by solid-phase immunoassay are not specific for bullous pemphigoid. Also, it is possible that some of our study subjects may have been suffering from aging-onset atopic dermatitis, chronic contact dermatitis, or autoeczematization/ID reaction rather than eczematous drug eruptions. Several of our study subjects and control subjects did have elevated IgE blood levels. However, none of the study or control subjects had in vitro drug-induced positive T-cell proliferative responses/cytokine production or drug patch tests, so the question of aging-onset atopic dermatitis being a confounder in our study is moot.
Additionally, our identification of study participants was based upon skin biopsy for routine hematoxylin-eosin examination showing presence of spongiotic dermatitis with eosinophils in the inflammatory infiltrate and/or the presence of overlapping elements of other inflammatory histologic patterns. Seitz et al. recently performed a study in which 91 patients with skin biopsy specimens suggestive of an acute exanthem temporally related to an identifiable medication were allergy tested to the possible offending medication (12). Prick testing, intradermal prick testing, LTT, and provocation testing excluded drug hypersensitivity in 56 of the patients and confirmed non-IgE-mediated drug hypersensitivity in 35 of the patients (positive predictive value of 40.7%). The authors concluded that histopathology is not useful in differentiating drug-mediated exanthems from non-drug-mediated exanthems. Thus, it is plausible that many of the participants we identified by dermatopathologic evaluation of skin biopsy specimens did not truly have a drug-mediated eczematous eruption.
Despite our negative findings, case reports and general clinical experience support the hypothesis that a number of drug classes are capable of inducing eczematous drug eruptions in all age groups. In addition, there is a growing body of evidence supporting the idea that different drug classes, including CCBs and HCTZ, can induce other T cell-mediated inflammatory dermatoses such as subacute cutaneous lupus erythematosus (13-16).
There are other ways to consider the negative results of our pilot study. Due to their pharmacologic effects on intracellular calcium signaling, at certain concentrations CCB are known to inhibit mitogen-induced T cell activation in vitro (17,18). Since in vitro mitogen-induced T cell proliferative responses are typically stronger/higher than antigen-induced T cell responses, it would seem safe to assume that drug antigen-specific T cell proliferative responses would also be suppressed at the same concentrations of CCB. Also, given that calcium flux is essential for lymphocyte proliferation and cytokine release, it is unlikely that CEEA from a CCB would be due to a T cell-mediated process.
CCB (and/or their metabolites) at therapeutic dosing levels are not known to be clinically immunosuppressive. That is to say, CCB at therapeutic doses in humans do not result in an observable decrease in resistance to opportunistic infection nor an increase in opportunistic malignancies. Supporting this is the fact that there are no warnings of immunosuppression as an adverse effect in the package inserts of the individual drugs in the CCB class. However, it has been suggested that CCBs used in conjunction with clinically significant immunosuppressives, such as cyclosporine, may provide a mild additive immunosuppressive effect (19,20).
The concentrations of CCB examined in our study subjects ranged from 31.25 to 1,000 ng/mL. Koike et al. reported that after oral administration of a therapeutic dose of verapamil in humans, the peak serum concentration was 219.09 ng/mL on average (21). Other pharmacokinetic studies have documented that steady-state blood levels of CCB after therapeutic dosing in humans is in the 100–300 ng/mL range (22-24). Our in vitro experimental conditions employed therapeutic concentrations of CCB and demonstrated inhibition of in vitro cell proliferation and cytokine responses only at the upper levels of physiological blood concentrations. Thus, our negative results were not entirely due to CCBs pharmacologically blocking in vitro T cell responses.
It has been suggested that topical application of pharmacological concentrations of CCB may have a local immunosuppressive effect in the skin (25). However, previous work has suggested that drug patch testing with CCBs is feasible. Girardi et al. reported a positive drug patch test to diltiazem in a patient with diltiazem-induced acute generalized exanthematous pustulosis (26). This argues against the possibility that percutaneous penetration of the CCB drug applied topically under occlusion in very high concentrations (10–30% in petrolatum) in the patch test protocol produced a local immunosuppressive effect on the cutaneous DTH response.
Given that CCBs are extensively metabolized by first pass hepatic metabolism, it is also possible that CCB metabolites are the pathogenic mediators responsible for drug-induced chronic eczematous reactions. In addition, CCB and HCTZ pills/capsules can contain dye chemicals that have been documented to be responsible for drug-induced hypersensitivity clinical phenomena. This hypothesis was not tested in our studies. Future studies in this area might include testing for dye hypersensitivity and utilize hepatic microsomal systems to “pre-metabolize” the parent drug in vitro prior to testing for drug antigen-specific T cell memory responses. We would propose that such studies exclude subjects having any evidence of prodromal/non-bullous bullous pemphigoid and aging-onset atopic dermatitis as reflected by elevated blood IgE levels.
Finally, it can be argued that by testing circulating T cells in our pilot study, we were not testing the most skin disease-relevant subpopulation of T cells. It has been reported that the human body contains 10–20 billion resident memory T cells having a skin-homing phenotype (CD45RO/CLA/CCR4) (27). There are 20-fold more T cells with this skin-homing phenotype in the skin than in blood. Skin-homing T cells consist of a mix of helper, cytotoxic, and regulatory subsets. It is quite possible that the subpopulation of memory T cells reactive with CCB and/or HCTZ antigens might be diluted beyond the point of detection with available clinical immunology techniques in peripheral blood. It is also not yet known whether the antigen-specific reactivity of such skin resident T memory cells can be assayed by conventional drug patch testing.
It was our hope that publication of the negative results of this pilot study might be of value in guiding others in the future who decide to try to move this important area of clinical research forward. As a note of caution, care should be taken in selecting the in vitro assay concentrations of CCB for T cell stimulating studies. CCB concentrations higher than therapeutic levels in human plasma (100–300 ng/mL) could be expected to have a broad inhibiting effect on T cell proliferation due to their impact on intracellular calcium signaling.
Porebski and colleagues have recently suggested that a single parameter of in vitro T cell activation may not be adequate in identifying a drug-induced DHR in human skin (28). In future studies of CCB-induced T cell activation within this context, appropriate care should be taken to examine in vitro CCB drug antigen concentrations within the in vivo CCB therapeutic blood level range.
Acknowledgements
The authors would like to express their appreciation to Dr. Gerald J. Gleich, M.D., University of Utah, Department of Dermatology and Dr. Douglas L. Powell, M.D., University of Utah, Department of Dermatology, for their thoughtful guidance on study methods at the beginning of this study. We also would like to thank Colby Bingham, M.D., University of Missouri, Department of Dermatology, for his assistance in acquisition of data. These individuals did not receive compensation for their help.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from the Institutional Review Board at the University of Utah for a single center (No. IRB_00044966), proof of concept pilot study.
References
- Hunziker T, Bruppacher R, Kuenzi UP, et al. Classification of ADRs: a proposal for harmonization and differentiation based on the experience of the Comprehensive Hospital Drug Monitoring Bern/St. Gallen, 1974-1993. Pharmacoepidemiol Drug Saf 2002;11:159-63. [Crossref] [PubMed]
- Summers EM, Bingham CS, Dahle KW, et al. Chronic eczematous eruptions in the aging: further support for an association with exposure to calcium channel blockers. JAMA Dermatol 2013;149:814-8. [Crossref] [PubMed]
- Joly P, Benoit-Corven C, Baricault S, et al. Chronic eczematous eruptions of the elderly are associated with chronic exposure to calcium channel blockers: results from a case-control study. J Invest Dermatol 2007;127:2766-71. [Crossref] [PubMed]
- Pichler WJ, Tilch J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy 2004;59:809-20. [Crossref] [PubMed]
- Kano Y, Hirahara K, Mitsuyama Y, et al. Utility of the lymphocyte transformation test in the diagnosis of drug sensitivity: dependence on its timing and the type of drug eruption. Allergy 2007;62:1439-44. [Crossref] [PubMed]
- Martins TB, Bandhauer ME, Bunker AM, et al. New childhood and adult reference intervals for total IgE. J Allergy Clin Immunol 2014;133:589-91. [Crossref] [PubMed]
- Martins TB, Pasi BM, Pickering JW, et al. Determination of cytokine responses using a multiplexed fluorescent microsphere immunoassay. Am J Clin Pathol 2002;118:346-53. [Crossref] [PubMed]
- Martins TB, Pasi BM, Litwin CM, et al. Heterophile antibody interference in a multiplexed fluorescent microsphere immunoassay for quantitation of cytokines in human serum. Clin Diagn Lab Immunol 2004;11:325-9. [PubMed]
- Martins TB, Anderson JL, Muhlestein JB, et al. Risk factor analysis of plasma cytokines in patients with coronary artery disease by a multiplexed fluorescent immunoassay. Am J Clin Pathol 2006;125:906-13. [Crossref] [PubMed]
- Lochmatter P, Zawodniak A, Pichler WJ. In vitro tests in drug hypersensitivity diagnosis. Immunol Allergy Clin North Am 2009;29:537-54. [Crossref] [PubMed]
- Sachs B, Erdmann S, Malte Baron J, et al. Determination of interleukin-5 secretion from drug-specific activated ex vivo peripheral blood mononuclear cells as a test system for the in vitro detection of drug sensitization. Clin Exp Allergy 2002;32:736-44. [Crossref] [PubMed]
- Seitz CS, Rose C, Kerstan A, et al. Drug-induced exanthems: Correlation of allergy testing with histologic diagnosis. J Am Acad Dermatol 2013;69:721-8. [Crossref] [PubMed]
- Srivastava M, Rencic A, Diglio G, et al. Drug-induced Ro/SSA-positive cutaneous lupus erythematosus. Arch Dermatol 2003;139:45-9. [Crossref] [PubMed]
- Reed BR, Huff JC, Jones SK, et al. Subacute cutaenous lupus erythematosus associated with hydrochlorothiazide. Ann Intern Med 1985;103:49-51. [Crossref] [PubMed]
- Crowson AN, Magro CM. Diltiazem and subacute cutaneous lupus erythematosus-like lesions. N Engl J Med 1995;333:1429. [Crossref] [PubMed]
- Callen JP. Drug-induced subacute cutaneous lupus erythematosus. Lupus 2010;19:1107-11. [Crossref] [PubMed]
- Witkowski JM, Siebert J, Lukaszuk K, et al. Comparison of effect of a panel of membrane channel blockers on the proliferative, cytotoxic and cytoadherence abilities of human peripheral blood lymphocytes. Immunopharmacology 1993;26:53-63. [Crossref] [PubMed]
- Zanker B, Marx S, Strom TB, et al. The immunosuppressive effects of verapamil upon mitogen activated and allo-antigen inducible human cytotoxic T-lymphocytes. Int J Immunopharmacol 1994;16:507-17. [Crossref] [PubMed]
- Bruserud O. The additive effect of certain drugs on the cyclosporine A inhibition of human T-cell proliferation. Studies using theophyllamine, warfarin, verapamil and dipyridamol. APMIS 1990;98:1070-6. [Crossref] [PubMed]
- Weir MR, Peppler R, Gomolka D, et al. Additive inhibition of afferent and efferent immunological responses of human peripheral blood mononuclear cells by verapamil and cyclosporine. Transplantation 1991;51:851-7. [Crossref] [PubMed]
- Koike Y, Shimamura K, Shudo I, et al. Pharmacokinetics of verapamil in man. Res Commun Chem Pathol Pharmacol 1979;24:37-47. [PubMed]
- Chelly JE, Hill DC, Abernethy DR, et al. Pharmacodynamic and pharmacokinetic interactions between lidocaine and verapamil. J Pharmacol Exp Ther 1987;243:211-6. [PubMed]
- Mattila J, Mäntylä R, Taskinen J, et al. Pharmacokinetics of sustained-release verapamil after a single administration and at steady state. Eur J Drug Metab Pharmacokinet 1985;10:133-8. [Crossref] [PubMed]
- D’Agostino HJ Jr, Pritchett EL, Shand DG, et al. Effect of verapamil on left ventricular function at rest and during exercise in normal men. J Cardiovasc Pharmacol 1983;5:812-7. [Crossref] [PubMed]
- McFadden J, Bacon K, Camp R. Topically applied verapamil hydrochloride inhibits tuberculin-induced delayed-type hypersensitivity reactions in human skin. J Invest Dermatol 1992;99:784-6. [Crossref] [PubMed]
- Girardi M, Duncan KO, Tigelaar RE, et al. Cross-comparison of patch test and lymphocyte proliferation responses in patients with a history of acute generalized exanthematous pustulosis. Am J Dermatopathol 2005;27:343-6. [Crossref] [PubMed]
- Seneschal J, Clark RA, Gehad A, et al. Human epidermal Langerhans cells maintain immune homeostasis in skin by activating skin resident regulatory T cells. Immunity 2012;36:873-84. [Crossref] [PubMed]
- Porebski G, Pecaric-Petkovic T, Groux-Keller M, et al. In vitro drug causality assessment in Stevens-Johnson syndrome - alternatives for lymphocyte transformation test. Clin Exp Allergy 2013;43:1027-37. [Crossref] [PubMed]


