Insight from a large real-world cohort of patients: does it confirm the results of the randomized trials?
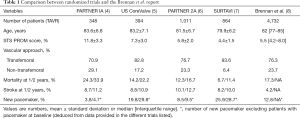
Since the first transcatheter aortic valve replacement (TAVR) in 2002, the procedure has become a routine treatment for symptomatic severe aortic valve stenosis (AS) with centers performing more than 600 procedures a year (1). Initially recommended for AS patients at prohibitive or high surgical risk, technological improvements (e.g., vascular access size, reduction of residual paravalvular leak) in addition to both greater operator experience and stepwise accumulation of data have allowed its extension to lower risk patients, with good clinical outcomes (2,3). To date, four major randomized trials (Table 1) have showed non-inferiority and even superiority for the US CoreValve Pivotal trial (5) of TAVR when compared to surgical valve replacement (SAVR) in regards to mortality and stroke at 2 years (4-7). The 2017 American Heart Association (AHA)/American College of Cardiology (ACC) guidelines update on valvular heart disease (9) now considers TAVR as a class IIa indication [Level of Evidence (LOE) B-R] for the treatment of symptomatic severe AS in intermediate risk patients whereas TAVR was allocated a class I indication (LOE B) in the latest guidelines from the European Society of Cardiology (ESC). Of note, emphasis is given to a heart team assessment and decision. The publication of Surgical Replacement and Transcatheter Aortic Valve Implantation (SURTAVI) between the releases of these two different guidelines has certainly contributed to the higher class in the ESC guidelines for TAVR in intermediate risk patients (10).
Full table
The article by Brennan et al. (8) published in the J Am Coll Cardiol earlier this year compared the results in the United States of America of the largest national representative real-world TAVR cohort, namely the Transcatheter Valve Therapy (TVT) registry to the Society of Thoracic Surgeons (STS) National Database for SAVR in a population of high and intermediate risk patients. From these 2 registries, patients considered eligible for both procedures were propensity-matched to assess mortality, stroke and days alive out of hospital at 1 year. Importantly, patients with characteristics that strongly favour one strategy over the other (including age <65 or >90 years, other major cardiac operations, history of endocarditis, emergency or salvage status, primary aortic insufficiency, hostile chest or porcelain aorta, moderate to severe mitral stenosis, and STS score <3%) were not considered for the propensity-matching. In the end, when respecting the inclusion criteria and the propensity matching, only 4,732 out of 17,910 patients in the TVT registry (26% of the population of interest) were analysed.
Does this analysis from Brennan et al. involving in total 9,464 patients (median age of 82 years, median STS score of 5.6%) confirm the results of the randomized trials?
Indeed, no difference in overall mortality at 1 year was observed between the groups (17.3% vs. 17.9%, P=0.4, respectively for TAVR vs. SAVR). However, in-hospital mortality was lower among TAVR vs. SAVR patients (respectively 3% vs. 5%, P<0.001). Mortality was similar among most sub-groups with the exception of patients with prior cardiac surgery who presented lower mortality at 1 year in the TAVR group. Interestingly when comparing the one year mortality of this population with the randomized trials, it appears higher than expected considering the mean age and STS score. Indeed, the US CoreValve pivotal trial (5) showed a mortality rate 3% lower than the Brennan et al. report despite higher STS scores and the PARTNER 2A study (6) with quite similar mean STS scores showed a mortality rate 5% lower.
Stroke rate was the highest during the first 30 days without any difference between both groups (respectively 2.8% vs. 2.8%, P=0.13). Even though the stroke event curve showed a slight divergence between 30 days and 1 year not in favour of TAVR patients, the overall difference in stroke rate was similar at 1 year (TAVR vs. SAVR hazard ratio: 1.18; 95% CI: 0.95–1.47). Importantly stroke rates for both TAVR and surgical patients (2.8% vs. 2.8%, P=0.13) are approximately 50% lower than in previous randomized trials (Table 1). This lower rate may be the reflection of routine clinical practice that does not include formal neurological assessment by a neurologist as is the case in the randomized trials (with the exception of PARTNER IA). Furthermore in the SENTINEL trial—assessing the benefit of cerebral protection device—the 30-day rate of stroke in the control group was as high as 9.1% and 5.6% in the device group, showing again higher stroke rates—90% being non-disabling strokes—when neurological exams are performed by confirmed neurologists (11).
In accordance to most of the recent trials, TAVR compared to SAVR is associated with higher major vascular complications (4.2% vs. 0.4%, P<0.001) but a lower rate of bleeding complications and acute renal failure requiring hemodialysis. Interestingly, patients in both groups had a similar proportion of days alive and out of hospital (rate ratio: 1.0; 95% CI: 0.98–1.02), whereas the less invasive approach namely TAVR was associated with more discharges home than SAVR (69.9% vs. 41.2% odds ratio: 3.19; 95% CI: 2.84–3.58). With respect to conduction disturbances the rate of new permanent pacemaker implantation was significantly higher after TAVR than SAVR (12.8% vs. 6.3%, P<0.001) similarly to most of the recent trials, especially when self-expanding valves are used (33% of Medtronic CoreValve bioprosthesis) (12).
In a population of intermediate- and high-risk patients from a large propensity-matched real-world population, Brennan et al. could confirm the absence of significant differences between the two therapeutic strategies when considering death and stroke at 1 year and also demonstrate similar days alive out of hospital at 1 year. These results were consistent across the spectrum of the different ranges of STS scores (3% to 5%, 5% to 8% and more than 8%). This report has several strengths. First it is the largest cohort of TAVR patients compared to propensity matched SAVR patients. Indeed, the largest TAVR cohort in a randomized trial included 1,011 patients, which is almost 5 times less than the Brennan report. In addition, the data were taken from the largest national registry of TAVR procedures which has an independent data auditing program contributing to increased data accuracy. Furthermore, we can consider that the rate of inclusion was high since in order to be reimbursed by Medicare, participants are required to submit 100% of their data to the TVT registry for TAVR and the STS national database for SAVR. Another criterion to be reimbursed is the existence of a heart team, which contributes to a structured and formal patient assessment process. Therefore, this report provides unique real-world data at a large scale.
On the other hand, this report has several limitations. The data are limited to a 1-year follow-up and for such a population eligible for both therapies and with a longer life expectancy than in the early days of TAVR, longer term data are essential. In addition, other important outcomes—either prognostic such as the degree of paravalvular leak and left ventricular function evolution or concerning the quality of life and functional class—for such a population are lacking.
Unfortunately, some aspects of this report do not correspond anymore to current practice even in the US. In this rapidly evolving field the valves implanted in this cohort—Edwards SAPIEN and Medtronic CoreValve prostheses in 67% and 33%, respectively are no longer used now that the latest generation prostheses (respectively the Edwards S3 and Evolut R and Pro) have shown their advantages (13-15). Furthermore, the rate of transfemoral approach (76.3%) was rather low considering that nowadays with the access size reduction more than 90% of procedures are performed by transfemoral approach in most centers. Since transfemoral TAVR in the PARTNER IIa trial showed lower mortality and stroke rates than surgery, whereas transthoracic access showed similar results than SAVR, the different guidelines favour TAVR in intermediate risk patients especially when transfemoral approach is feasible.
Finally, if we try to explain why the mortality rate at 1 year was higher than in the randomized trials, we can evoke several factors, such as the high rate of transthoracic access, an all-comer real-world patient population as opposed to the carefully selected population of randomized trials and potentially less operator experience in some of the participating centres. Indeed, since an inverse relationship between high volume centers and post-procedural adverse events does exist, the volume of procedures per operator and centers would have been valuable information. Even though the study by Brennan et al. excluded centers with very low volume, centers with as few as ten procedures during the study interval of 21 months still fulfilled the inclusion criteria. In a recent report from the Compulsory German Quality Assurance Registry on Aortic Valve Replacement (AQUA) of patients undergoing transfemoral TAVR, centers with <50 procedures per year had higher in-hospital mortality than those with >200 procedures per year. Moreover, there was a continuous statistically significant association between lower in-hospital mortality and increasing volume of procedures (16). Furthermore with the availability of a vast panel of different TAVR platforms, the ideal number of different prosthesis that should be used per operator/center is a matter of debate, but undoubtedly should be related to the number of procedures performed per center.
In conclusion, despite many European national registries (15,17-21) and randomized trials—for which direct translation of their results into a daily clinical practice may be limited by strict inclusion and exclusion criteria—the study by Brennan et al. provides unique data on TAVR outcomes derived from a large real-world cohort of patients and confirms the results of the major randomized trials. The propensity-matching was used to reduce selection bias and limit interpretation errors due to confounding factors. However, propensity matching is unable to correct for all confounding factors in a population. Randomized controlled trials are definitely the gold standard for limiting bias and to assess efficacy and safety of new procedures. Therefore to answer the remaining gaps in evidence (e.g., management of asymptomatic severe AS or low flow low gradient AS), randomized trials (EARLY-TAVR and TAVR-UNLOAD) are currently recruiting.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. S Noble is a proctor for Medtronic. Dr. Perrin has no conflicts of interest to declare.
References
- Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 2002;106:3006-8. [Crossref] [PubMed]
- Thourani VH, Kodali S, Makkar RR, et al. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet 2016;387:2218-25. [Crossref] [PubMed]
- Kodali S, Thourani VH, White J, et al. Early clinical and echocardiographic outcomes after SAPIEN 3 transcatheter aortic valve replacement in inoperable, high-risk and intermediate-risk patients with aortic stenosis. Eur Heart J 2016;37:2252-62. [Crossref] [PubMed]
- Kodali SK, Williams MR, Smith CR, et al. Two-Year Outcomes after Transcatheter or Surgical Aortic-Valve Replacement. N Engl J Med 2012;366:1686-95. [Crossref] [PubMed]
- Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Prosthesis. N Engl J Med 2014;370:1790-8. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609-20. [Crossref] [PubMed]
- Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2017;376:1321-31. [Crossref] [PubMed]
- Brennan JM, Thomas L, Cohen DJ, et al. Transcatheter Versus Surgical Aortic Valve Replacement: Propensity-Matched Comparison. J Am Coll Cardiol 2017;70:439-50. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;70:252-89. [Crossref] [PubMed]
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease: The Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2017;38:2739-86. [PubMed]
- Kapadia SR, Kodali S, Makkar R, et al. Protection Against Cerebral Embolism During Transcatheter Aortic Valve Replacement. J Am Coll Cardiol 2017;69:367-77. [Crossref] [PubMed]
- Noble S, Burri H, Roffi M. Surgical or Transcatheter Aortic-Valve Replacement. N Engl J Med 2017;377:196-7. [PubMed]
- Binder RK, Stortecky S, Heg D, et al. Procedural Results and Clinical Outcomes of Transcatheter Aortic Valve Implantation in Switzerland. An Observational Cohort Study of Sapien 3 Versus Sapien XT Transcatheter Heart Valves. Circ Cardiovasc Interv 2015;8:e002653. [Crossref] [PubMed]
- Perrin N, Roffi M, Frei A, et al. Thirty-day Outcome Following CoreValve Evolut R Transcatheter Aortic Valve Implantation: An All-comers Prospective Study. Rev Esp Cardiol (Engl Ed) 2017;70:713-9. [Crossref] [PubMed]
- Noble S, Stortecky S, Heg D, et al. Comparison of procedural and clinical outcomes with Evolut R versus Medtronic CoreValve: a Swiss TAVI registry analysis. EuroIntervention 2017;12:e2170-6. [Crossref] [PubMed]
- Bestehorn K, Eggebrecht H, Fleck E, et al. Volume-Outcome Relationship with Transfemoral Transcatheter Aortic Valve Implantation (TAVI) - Insights from the Compulsory German Quality Assurance Registry on Aortic Valve Replacement (AQUA). EuroIntervention 2017;13:914-20. [Crossref] [PubMed]
- Beckmann A, Hamm C, Figulla HR, et al. The German Aortic Valve Registry (GARY): a nationwide registry for patients undergoing invasive therapy for severe aortic valve stenosis. Thorac Cardiovasc Surg 2012;60:319-25. [Crossref] [PubMed]
- Gilard M, Eltchaninoff H, Iung B, et al. Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med 2012;366:1705-15. [Crossref] [PubMed]
- Ludman PF, Moat N, de Belder MA, et al. Transcatheter aortic valve implantation in the United Kingdom: temporal trends, predictors of outcome, and 6-year follow-up: a report from the UK Transcatheter Aortic Valve Implantation (TAVI) Registry, 2007 to 2012. Circulation 2015;131:1181-90. [Crossref] [PubMed]
- Ussia GP, Barbanti M, Petronio AS, et al. Transcatheter aortic valve implantation: 3-year outcomes of self-expanding CoreValve prosthesis. Eur Heart J 2012;33:969-76. [Crossref] [PubMed]
- Wenaweser P, Stortecky S, Heg D, et al. Short-term clinical outcomes among patients undergoing transcatheter aortic valve implantation in Switzerland: the Swiss TAVI registry. EuroIntervention 2014;10:982-9. [Crossref] [PubMed]


