Endobronchial ultrasound-transbronchial needle aspiration (EBUS/TBNA): a diagnostic challenge for mediastinal lesions
Introduction
Lung cancer treatment is closely related to the stage of the disease at the time of diagnosis (1,2). Mediastinal involvement radically modifies the therapeutic approach of pulmonary neoplasms, and it is therefore crucial to carry out a proper evaluation of lymph node stations at this point (3). Mediastinal invasive diagnostic methods, on the one hand, involve higher costs and disadvantages than imaging techniques, on the other hand, they provide material by which a diagnosis of certainty can be made (4,5). The usefulness of surgery in mediastinal staging is undeniable. VATS or thoracotomy allow extensive and accurate lymph node dissection especially on N2 lymph nodes (6,7). However, today there are alternative methods, such as video-assisted mediastinoscopy, with the same efficacy as conventional techniques but significantly less invasive (8). More recently, the introduction of endobronchial ultrasound/transbronchial needle aspiration (EBUS-TBNA) has been a turning point since, in the face of a minimal discomfort for the patient, and performing diagnostic levels of accuracy, sensitivity and specificity than more invasive methods (9). We analyzed the data of literature in order to evaluate the best method for the study of mediastinum in lung cancer patients.
Material and methods
We conducted a systematic review of the papers in literature by performing a search on the MEDLINE database through PubMed using the following criteria: “lung cancer AND lymph node AND mediastinal staging AND surgical AND invasive methods”. The selection of papers was made in double blind by two authors, including studies conducted over the last 5 years and excluding review articles; any discrepancies were then discussed and resolved. In addition, the risk of bias has been assessed following the Cochrane recommendations. The parameters taken into account in evaluating the methods include: sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy.
Results
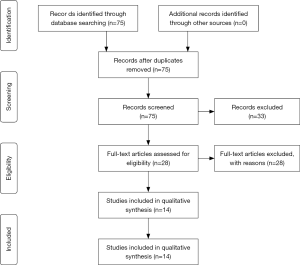
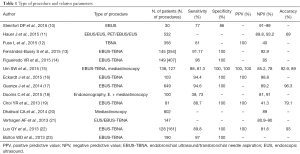
Figure 1 shows the flow diagram of the study selection process, according to preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. The search strategy identified 75 records. Records were screened at the title and abstract level, and 33 were excluded as irrelevant. The remaining 42 records were assessed in the full text. Of those, 14 were included as they corresponded to the search criteria (Table 1) (10-23). The size of the cohorts varied from 30 to 802 patients, with a total number of 3,550 patients. In all calculations, the invasive mediastinal staging was chosen as the reference. Lack of blinding was not considered likely to influence the primary outcome due to its objective nature. The parameters included are sensitivity, specificity, PPV, NPV, and diagnostic accuracy. However, it was not possible to evaluate all the parameters in each study. The results show that the most common techniques used in mediastinal invasive diagnosis are mediastinoscopy and EBUS-TBNA. These procedures are characterized by high sensitivity. In fact, the sensitivity of EBUS-TBNA is between 61% and 97% while for the mediastinoscopy it is between 73% and 81.3%. In addition, mediastinoscopy and EBUS-TBNA systematically reach a specificity and a PPV of 100% and 100% respectively. The NPV of EBUS-TBNA is between 81% and 98.8% although, in some studies considered (12,19), this method showed a very low NPV (40%, 41.3%) while the NPV of mediastinoscopy ranging from 78% to 91%. The diagnostic accuracy of EBUS-TBNA and mediastinoscopy were from 69% to 96.3% and 89% respectively.
Full table
Discussion
In the diagnosis and treatment of lung cancer, the mediastinal study plays a key role. Imaging surveys play a very important role in the diagnostic and preoperative phase as they are not invasive and characterized by good levels of sensitivity and specificity. Zhang et al. (24) compared the performance of the 18Fluorine-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG-PET/CT) in the preoperative phase with histologic findings obtained through invasive mediastinal staging techniques (mediastinoscopy or thoracotomy) related to 83 patients with non-small cell lung cancer (NSCLC). The data showed that PET/CT in the analysis of lymph node strains aggravated by mediastinoscopy has achieved good results in terms of sensitivity, specificity and NPV (respectively: 80%, 86% and 96%), while in terms of PPV, PET/CT they provided correct information only in 47% of cases; the data are worse if we compare the results of the mediastinal lymph nodes available only through thoracotomy access, in these cases PET sensitivity and specificity fall to 42% and 88% respectively. The comparison between imaging techniques and invasive methods in the mediastinal study causes controversy. According to Schonewolf et al. (25) there would be no obvious advantages in invasive methods compared to the use of 18F-FDG-PET/CT alone in the evaluation of mediastinal lymph nodes. In their experience, 236 patients were affected by NSCLC (a total of 257 lesions); of these, 180 patients were staged by single 18F-FDG-PET/CT (199 lesions) while the other 56 patients (58 lesions) were subjected to invasive mediastinal nodal staging (IMNS), of which patients 52 underwent EBUS and 4 to mediastinoscopy. Four parameters were considered: local recurrence-free survival (LRFS), nodal recurrence-free survival (NRFS), distant metastasis-free survival (DMFS), and overall survival (OS). According to the authors, the results obtained by 18F-FDG-PET/CT alone were not very far from those obtained by the 18F-FDG PET/CT + IMNS association: LFRS =37 vs. 47 months respectively; NFRS =34 vs. 42 months respectively; DMFS =36 vs. 47 months respectively and OS =37 vs. 47 months respectively. It should be considered, however, that if imaging techniques are characterized by greater execution speed and discomfort for the patient, on the other hand, they do not allow providing a diagnosis of certainty that can only be obtained through more invasive methods. Hauer et al. (11) compared histologic findings with preoperative results using 18F-FDG-PET/CT and EBUS-TBNA/endoscopic ultrasound/fine needle aspiration (EUS-FNA) in 532 patients who underwent surgery and lymphadenectomy for NSCLC. Authors demonstrated that the combined use of these techniques allowed a high NPV (93.2%). In addition, the cytological sampling reduced the risk of false positive outcomes while 18F-FDG-PET/CT alone was characterized by a PPV of 21%. Based on the combined use of 18F-FDG-PET/CT and the eco-guided techniques, the Authors concluded that in patients with no evidence of lymph node involvement it is not necessary more invasive diagnostic methods. From the analysis of the data in the literature, we have seen how the modern techniques of invasive mediastinal staging, especially mediastinoscopy and EBUS-TBNA, are characterized by high levels of sensitivity, specificity, accuracy, PPV and NPV. Mediastinoscopy is probably the most widely used technique since its introduction in 1959, and was routinely used in mediastinal staging in the event of neoplastic diseases. It allows us to reach the pretracheal lymph nodes (stations 1, 3), high and low paratracheal nodes (stations 2R, 2L, 4R, 4L) and anterior subcarinal nodes (station 7) (26). In 2007, the guidelines published by The European Society of Thoracic Surgeons (ESTS) concerning lymph node staging before their review in 2013, indicated mediastinoscopy as a gold standard in diagnosing upper mediastinal lymph nodes, and recourse was not advised solely in the presence of peripheral injuries or in case of 18F-FDG-PET/CT negativity (27). Despite the levels of invasiveness, this method is now considered by many to be an indispensable test in the study of the mediastinum; however, it does not allow for the study of the subcarinal nodes (station 7), inferior mediastinal node (stations 8, 9), aorto-pulmonary window node (station 6) and anterior mediastinal node (station 6) (26,27). In 2015 Chabowski et al. (28) reported their experience in the use of mediastinoscopy on a sample of 54 patients with radiological evidence of mediastinal pathology (lymph nodes >1 cm or mediastinal mass). Mediastinoscopy gave positive results in 32 cases (59.2%), allowing identifying 10 NSCLC, 2 small-cell lung cancers (SCLC), 11 sarcoidosis, 2 B cell lymphomas, 4 thymic neoplasms and 3 metastases. Negative outcomes were noted in the remaining 22 patients (40.8%), although 12 patients had metastatic dissemination diagnosed with other methods. The author concludes by saying that with a 72% sensitivity level and 100% specificity, mediastinoscopy should be used routinely in the diagnosis of mediastinal disease. In recent years, the need for complete lymph node dissections and not just lymph node sampling has led to an evolution of mediastinoscopic approaches. Currently, the two main techniques are transcervical extended mediastinal lymphadenectomy (TEMLA) and video-assisted mediastinoscopy lymphadenectomy (VAMLA) (29). In a 2010 work, Zieliński (30) reports the results of 587 NSCLC patients who underwent TEMLA between 2004 and 2009, for diagnostic and stage-based purposes. Thigh sensitivity for N2-N3 lymph nodes was 95.6%, specificity was 100%, accuracy of 98.8% while NPV and PPV were 98.4% and 100% respectively—considerable results when considering a rate of complications of 6.8% (40 out of 587 patients). The idea of using a video-camera in mediastinoscopy to improve imaging of the mediastinal structures dates back to 1989. Witte et al. (31) reported a retrospective study of 226 patients submitted to video-assisted mediastinoscopic surgery (VAMS); of these, 186 patients (82.3%) had a lung cancer, 34 patients (15%) a mediastinal lymphoma, 5 patients (2.2%) enlarged mediastinal lymph nodes in lung metastases and 1 patient (0.5%) a suspected mediastinal tumor. Of 186 patients with lung cancer, 144 had a resectable lung cancer and were submitted to VAMLA for mediastinal staging. According to authors, VAMLA allows dissection and sampling of the pretracheal and paratracheal compartments, of the subcarinal lymph nodes, of the right and left tracheobronchial nodes. One hundred and twenty-five of 144 procedures were complete, and 130 of 144 patients were first subjected to VAMLA for mediastinal staging and subsequently to open surgical staging. By analyzing the results, the sensitivity of all VAMLA procedures was 88.2%, the specificity was 100%, the false-negative rate was 1.7%, and the false-positive rate was 0%; for completed VAMLA procedures, sensitivity and specificity is 100% and 93.75% respectively, associated with a false negative of 0.9%. Recently, Onat et al. (32) have shown that mediastinoscopy is also effective in the diagnosis of non-neoplastic pulmonary disease. In 229 patients with mediastinal lymphadenopathy, mediastinoscopy identified sarcoidosis (n=100), tuberculous lymphadenitis (n=66) anthracosis lymphadenitis (n=44), lymphoma (n=11), metastatic carcinoma (n=5), silicosis (n=1), thymoma (n=1), and Castleman’s disease (n=1). In our analysis, mediastinoscopy showed sensitivity values ranging from 73% to 81.3%, associated with a 100% specificity. A particularly important aspect emerging from data analysis is the high NPV associated with this method, ranging from 78% to 91%, indicating a poor chance of obtaining false negative results (Table 1). With the introduction of the new map of mediastinal lymph nodes in 2009 by the International Association for the Study of Lung Cancer (IASLC) (33), ESTS proposed in 2014 a revision of the guidelines (34) for lymph nodes in the advent of new less invasive diagnostic techniques. EBUS-TBNA and EUS-FNA become (when possible) the first-case studies of radiological evidence of TC and/or PET mediastinal involvement. EBUS is particularly indicated in the detection of 2R, 2L, 4R, 4L, 7, 10, 11 and 12 lymph node stations, while EUS also allows us to reach stations 8 and 9, some of which are difficult to discover with mediastinoscopy. In view of the low invasiveness, EBUS-TBNA may be recommended as a complementary examination to the imaging study. Lilo et al. (35) reported the results of EBUS-TBNA on 70 patients previously subjected to 18F-FDG-PET/CT for the study of lymph nodes. Of 140 lymph nodes considered, 54 were negative to 18F-FDG-PET/CT while the subsequent use of EBUS-TBNA allowed identifying 4 (7%) lymph nodes that possessed signs of malignancy. This demonstrates how the use of invasive methods significantly improves diagnostic accuracy since false 18F-FDG-PET/CT negativity is explained by the presence of micrometastases that can only be detected by a lymph node biopsy. Thanks to the high levels of diagnostic accuracy, before resorting to more invasive techniques, Cetinkaya et al. (36) consider EBUS-TBNA very useful also in the stages of restaging after chemotherapy and radiotherapy. Of the 73 lymph nodes N2 analyzed by EBUS-TBNA, 25 (34.2%) were positive and 48 (65.8%) were negative of which only 6 (12.5%) were metastasis sites that could only be detected using surgical procedure techniques. In our analysis, EBUS-TBNA showed very high efficacy, achieving sensitivity ranges from 77% to 97%, specificities ranging from 86% to 100%, a 100% PPV, a NPV from 41% to 98.8% and an accuracy of between 79% and 96%, demonstrating a useful, safe and reliable examination in the diagnosis and staging of the mediastinum (Table 1). In fact, the subcarinal (75.0% vs. 82.5%) and 4L (52.4% vs. 81%) lymph nodes are studied more easily with the EBUS-TBNA than the mediastinoscopy. Moreover, EBUS-TBNA allows to study N3 lymph nodes.
Conclusions
Currently, the most used techniques for mediastinal staging are mediastinoscopy and EBUS-TBNA. Mediastinoscopy is characterized by high levels of sensitivity, specificity and significantly reduces the risk of false negatives, allowing in most cases a diagnosis of certainty and a proper staging; on the other hand, it is a fairly sensible technique that also involves risks for the patient. The advent of EBUS-TBNA has allowed, with very low invasiveness, results comparable to those of the most invasive methods, enabling study with relative ease and safety for the patient.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wakeam E, Byrne JP, Darling GE, et al. Surgical Treatment for Early Small Cell Lung Cancer: Variability in Practice and Impact on Survival. Ann Thorac Surg 2017;104:1872-80. [Crossref] [PubMed]
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-e313S.
- Krantz SB, Lutfi W, Kuchta K, et al. Improved Lymph Node Staging in Early-Stage Lung Cancer in the National Cancer Database. Ann Thorac Surg 2017;104:1805-14. [Crossref] [PubMed]
- Brunelli A. European Society of Thoracic Surgeons preoperative mediastinal staging guidelines: From face validity to external validity. J Thorac Cardiovasc Surg 2018;155:796-7. [Crossref] [PubMed]
- Liu H, Zhou J, Feng QL, et al. Minimally invasive endoscopic staging for mediastinal lymphadenopathy in lung cancer: a systematic review protocol. BMJ Open 2014;4:e005707. [Crossref] [PubMed]
- Zhang W, Wei Y, Jiang H, et al. Thoracotomy is better than thoracoscopic lobectomy in the lymph node dissection of lung cancer: a systematic review and meta-analysis. World J Surg Oncol 2016;14:290. [Crossref] [PubMed]
- Reichert M, Steiner D, Kerber S, et al. A standardized technique of systematic mediastinal lymph node dissection by video-assisted thoracoscopic surgery (VATS) leads to a high rate of nodal upstaging in early-stage non-small cell lung cancer. Surg Endosc 2016;30:1119-25. [Crossref] [PubMed]
- Cho JH, Kim J, Kim K, et al. A comparative analysis of video-assisted mediastinoscopy and conventional mediastinoscopy. Ann Thorac Surg 2011;92:1007-11. [Crossref] [PubMed]
- Ge X, Guan W, Han F, et al. Comparison of Endobronchial Ultrasound-Guided Fine Needle Aspiration and Video-Assisted Mediastinoscopy for Mediastinal Staging of Lung Cancer. Lung 2015;193:757-66. [Crossref] [PubMed]
- Steinfort DP, Siva S, Leong TL, et al. Systematic Endobronchial Ultrasound-guided Mediastinal Staging Versus Positron Emission Tomography for Comprehensive Mediastinal Staging in NSCLC Before Radical Radiotherapy of Non-small Cell Lung Cancer: A Pilot Study. Medicine (Baltimore) 2016;95:e2488. [Crossref] [PubMed]
- Hauer J, Szlubowski A, Żanowska K, et al. Minimally invasive strategy for mediastinal staging of patients with lung cancer. Pol Arch Med Wewn 2015;125:910-3. [PubMed]
- Fuso L, Varone F, Smargiassi A, et al. Usefulness of Conventional Transbronchial Needle Aspiration for Sampling of Mediastinal Lymph Nodes in Lung Cancer. J Bronchology Interv Pulmonol 2015;22:294-9. [Crossref] [PubMed]
- Fernández-Bussy S, Labarca G, Canals S, et al. Diagnostic yield of endobronchial ultrasound-guided transbronchial needle aspiration for mediastinal staging in lung cancer. J Bras Pneumol 2015;41:219-24. [Crossref] [PubMed]
- Figueiredo VR, Cardoso PF, Jacomelli M, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for lung cancer staging: early experience in Brazil. J Bras Pneumol 2015;41:23-30. [Crossref] [PubMed]
- Um SW, Kim HK, Jung SH, et al. Endobronchial ultrasound versus mediastinoscopy for mediastinal nodal staging of non-small-cell lung cancer. J Thorac Oncol 2015;10:331-7. [Crossref] [PubMed]
- Eckardt J, Licht PB. Endobronchial ultrasound-guided transbronchial needle aspiration is a sensitive method to evaluate patients who should not undergo pulmonary metastasectomy†. Interact Cardiovasc Thorac Surg 2015;20:482-5; discussion 485. [Crossref] [PubMed]
- Guarize J, Pardolesi A, Donghi S, et al. Endobronchial ultrasound for mediastinal staging in lung cancer patients. Multimed Man Cardiothorac Surg 2014;2014:mmu021. [Crossref] [PubMed]
- Dooms C, Tournoy KG, Schuurbiers O, et al. Endosonography for mediastinal nodal staging of clinical N1 non-small cell lung cancer: a prospective multicenter study. Chest 2015;147:209-15. [Crossref] [PubMed]
- Choi YR, An JY, Kim MK, et al. The diagnostic efficacy and safety of endobronchial ultrasound-guided transbronchial needle aspiration as an initial diagnostic tool. Korean J Intern Med 2013;28:660-7. [Crossref] [PubMed]
- Dhaliwal CA, Andrews TD, Walker WS, et al. Histological evaluation of preoperative mediastinoscopy lymph node biopsies in non-small cell lung cancer. J Clin Pathol 2014;67:76-80. [Crossref] [PubMed]
- Verhagen AF, Schuurbiers OC, Looijen-Salamon MG, et al. Mediastinal staging in daily practice: endosonography, followed by cervical mediastinoscopy. Do we really need both? Interact Cardiovasc Thorac Surg 2013;17:823-8. [Crossref] [PubMed]
- Luo GY, Cai PQ, He JH, et al. Application of endobronchial ultrasound-guided transbronchial needle aspiration in the management of mediastinal and hilar lymphadenopathy without intrapulmonary mass: experience from the largest cancer center of southern China. Cell Biochem Biophys 2013;67:1533-8. [Crossref] [PubMed]
- Bolton WD, Johnson R, Banks E, et al. Utility and accuracy of endobronchial ultrasound as a diagnostic and staging tool for the evaluation of mediastinal adenopathy. Surg Endosc 2013;27:1119-23. [Crossref] [PubMed]
- Zhang Y, Elam Y, Hall P, et al. The Role of Fluorodeoxy-D-glucose Positron Emission Tomography/Computed Tomography in Nodal Staging of Nonsmall Cell Lung Cancer in Sequential Surgical Algorithm. World J Nucl Med 2017;16:281-5. [Crossref] [PubMed]
- Schonewolf CA, Verma V, Post CM, et al. Outcomes of invasive mediastinal nodal staging versus positron emission tomography staging alone for early-stage non-small cell lung cancer treated with stereotactic body radiation therapy. Lung Cancer 2018;117:53-9. [Crossref] [PubMed]
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-e50S.
- De Leyn P, Lardinois D, Van Schil PE, et al. ESTS guidelines for preoperative lymph node staging for non-small cell lung cancer. Eur J Cardiothorac Surg 2007;32:1-8. [Crossref] [PubMed]
- Chabowski M, Szymanska-Chabowska A, Skotarczak J, et al. The role of mediastinoscopy in the diagnosis of thoracic disease: one-year single center experience. Adv Exp Med Biol 2015;852:1-4. [PubMed]
- Yendamuri S, Demmy TL. Is VAMLA/TEMLA the new standard of preresection staging of non-small cell lung cancer? J Thorac Cardiovasc Surg 2012;144:S14-7. [Crossref] [PubMed]
- Zieliński M. Transcervical extended mediastinal lymphadenectomy. Thorac Surg Clin 2010;20:215-23. [Crossref] [PubMed]
- Witte B, Wolf M, Huertgen M, et al. Video-assisted mediastinoscopic surgery: clinical feasibility and accuracy of mediastinal lymph node staging. Ann Thorac Surg 2006;82:1821-7. [Crossref] [PubMed]
- Onat S, Ates G, Avcı A, et al. The role of mediastinoscopy in the diagnosis of non-lung cancer diseases. Ther Clin Risk Manag 2017;13:939-43. [Crossref] [PubMed]
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Lilo MT, Allison DB, Younes BK, et al. The critical role of EBUS-TBNA cytology in the staging of mediastinal lymph nodes in lung cancer patients: A correlation study with positron emission tomography findings. Cancer Cytopathol 2017;125:717-25. [Crossref] [PubMed]
- Cetinkaya E, Usluer O, Yılmaz A, et al. Is endobronchial ultrasound-guided transbronchial needle aspiration an effective diagnostic procedure in restaging of non-small cell lung cancer patients? Endosc Ultrasound 2017;6:162-7. [Crossref] [PubMed]


