The potential detrimental effects of calcium channel blockers’ overdose and current available management
Introduction
Amlodipine is a commonly used vasodilator for the management of cardiovascular conditions such as hypertension, angina. Interestingly, almost 18% of cardiovascular drug toxicity related annual deaths are due to amlodipine. We present a case of amlodipine toxicity causing intractable acidosis, cardiovascular decompensation and eventual death. We aim to describe the clinical implications of the amlodipine related toxic dose effects, underlying pathophysiology, and treatment strategies.
Case presentation
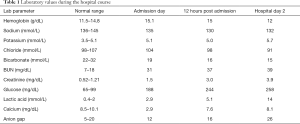
A 51-year-old Caucasian male with past medical history of hypertension presented to our hospital after an intentional overdose of 50 10-mg tablets of amlodipine (total of 500 mg) and a self-inflicted abdominal knife wound in an apparent suicide attempt. He was intubated in the field and at the time of presentation his vitals were significant for temperature of 96 F, pulse of 68 beats/minutes, blood pressure 84/49 mmHg and he was on invasive mechanical ventilatory support (assist control mode) with pulse oxygen saturation 100%. Pertinent physical examination findings included a superficial knife wound in the left lower abdominal quadrant, non-reactive pupils, cool extremities and bilateral rhonchi and rales. The rest of the physical examination was negative. A CT scan with contrast of the abdomen and pelvis revealed that the knife wound did not penetrate the peritoneum and the patient was cleared from a trauma perspective. The patient’s hemoglobin remained relatively stable over the subsequent hours despite aggressive fluid resuscitation (Table 1). Imaging which demonstrated no significant intraabdominal trauma and hemoglobin levels remaining stable both argued against the self-inflicted knife wound as an explanation for hemodynamic instability.
Full table
Initial diagnostic work up revealed multiple metabolic and electrolyte abnormalities (Table 1). Chest X-ray showed bilateral pulmonary edema. Transthoracic echocardiogram was consistent with global hypokinesis and left ventricular dysfunction with ejection fraction 25–30%. His vitals and labs continued to deteriorate despite use of multiple pressors and critical care medications including sodium bicarbonate, dobutamine, dopamine, epinephrine, norepinephrine, vasopressin, lipid emulsion, insulin with dextrose infusion, calcium chloride, hydrocortisone and electrolytes correction (Table 1). A left ventriculogram was consistent with the echocardiogram findings and even after placement of a ventricular assist device (VAD)—Impella CP 4.0 [delivering 4 liters of cardiac output (CO) per minute], the patient’s clinical condition continued to worsen. Further hospital course was complicated with critical limb ischemia (distal to Impella site) and worsening of multi-organ system dysfunction. Eventually, the patient’s family opted for Do Not Resuscitate (DNR) orders and unfortunately after all aggressive critical interventions and complicated hospital course, the patient expired.
Discussion
Amlodipine, a dihydropyridine calcium channel blocker (CCB), exerts its vasodilator effect through its ability to bind and block the alpha-1 submit of L-type calcium channel. This results in reduced calcium influx and thus reduced stimulation of the ryanodine receptor on the sarcoplasmic reticulum, leading to smooth muscle relaxation and vasodilation. It has a half-life of 30–50 hours and a large volume of distribution (21 L/kg). Usually, it has a minimal influence on myocardial contractility, however at toxic dosage (5–10 times usual dosage) pharmacological selectivity is lost and hypotension, bradycardia, and signs of heart failure can be seen (1,2). Pre-capillary vasodilatation results in excessive pulmonary capillary transudation leading to non-cardiogenic pulmonary edema. It interferes with glucose metabolism by inhibition of calcium-stimulated mitochondrial activity and ATP hydrolysis resulting in lactic acidosis. Additionally, it inhibits calcium-mediated insulin release, leading to hyperglycemia. Tissue hypo-perfusion is often complicated with renal failure and end-organ ischemia.
The treatment algorithm of CCB toxicity involves the traditional measures of airway and circulatory support, followed by use of medications for correction of metabolic and cardiovascular abnormalities. In our case, the clinical course was unmanageable with all traditional treatment measures and to address the refractory shock, we utilized Impella cardiac assist device without any significant improvement in tissue perfusion or hemodynamics. Recently, an expert consensus has suggested use of devices such as venoarterial extracorporeal membrane oxygenation (VA-ECMO) as a rescue measure in CCB toxicity with shock presentation due to the possible benefits outweighing the risks such as limb ischemia, bleeding, or thrombosis (3). A practical limitation with VA-ECMO use is need for high expertise and limited center availability, which is less required with other VADs such as Impella catheter. While theoretically, VADs mediated ventricular unloading and increased CO should improve circulation at both organ and tissue levels, recommendations are neutral with regards to Impella use due to lack of clinical or research experience.
Conclusions
With the rising prevalence of cardiovascular disease burden and an emphasis on primary and secondary disease prevention, use of medications such as CCBs will continue to increase. Although CCB toxicity is associated with significant morbidity and fatal outcomes, surprisingly no formal guidelines exist with respect to in-hospital management. As hemodynamic compromise is commonly seen in this scenario, further research is needed to define a clear treatment approach including the role of mechanical circulatory devices in these critically sick patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bronstein AC, Spyker DA, Cantilena LR Jr, et al. 2010 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila) 2011;49:910-41. [Crossref] [PubMed]
- Ghosh S, Sircar M. Calcium channel blocker overdose: experience with amlodipine. Indian J Crit Care Med 2008;12:190-3. [Crossref] [PubMed]
- St-Onge M, Anseeuw K, Cantrell FL, et al. Experts Consensus Recommendations for the Management of Calcium Channel Blocker Poisoning in Adults. Crit Care Med 2017;45:e306-15. [Crossref] [PubMed]


