Paradoxical emboli following a pulmonary embolus in the presence of a patent foramen ovale
Introduction
Paradoxical embolism occurs when a venous thrombus passes through a patent foramen ovale (PFO) entering the arterial circulation and manifesting as an arterial embolus due to right-to-left shunting. The prevalence of PFO is estimated to be between 25–30% of the population based on an autopsy study and transesophageal echocardiogram (TEE) study (1,2). In patients with cryptogenic stroke, the prevalence of PFO is even higher at almost 40% as determined in the Patent Foramen Ovale with Cryptogenic Stroke Study (3). We describe a case of acute cerebral vascular accident (CVA) and right subclavian arterial embolus in the setting of pulmonary emboli and PFO.
Case presentation
A 74-year-old woman with multiple comorbidities; including coronary artery disease status post stenting, hypertension, hyperlipidemia, tachycardia-bradycardia syndrome status post permanent pacemaker, breast cancer status post left mastectomy, asthma, deep venous thrombosis, diabetes mellitus type 2, and hypothyroidism presented to the emergency department with complaints of acute onset of shortness of breath, weakness, and right arm pain. Her family history was remarkable for a daughter who passed away at the age of 42 from a massive cerebrovascular accident. The patient denied any tobacco, alcohol, or illicit drug use. She was hemodynamically stable on initial presentation. Physical examination was remarkable for an elderly appearing woman in moderate distress secondary to right upper extremity pain. Lungs were clear to auscultation bilaterally. Cardiovascular exam yielded a regular rate and rhythm, normal S1 and S2, and no murmurs. On neurological examination, patient was noted to be alert, awake, and oriented to self, place, and time. Her pupils were equally round and reactive to light and accommodation. Extraocular movements were intact, but she had right homonymous hemianopsia. The patient had a symmetric face, and her tongue was midline on protrusion. She moved all extremities equally, and strength was equal in bilateral upper and lower extremities. She had decreased sensation to light touch in the right upper extremity compared to the left upper extremity. She also had ataxia noted in the right lower extremity. In the right upper extremity, the brachial and radial pulses were non-palpable. There were no Doppler signals of the radial, brachial, or axillary arteries in the right upper extremity.
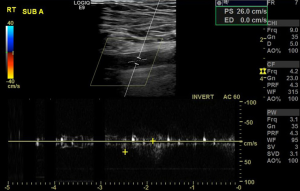
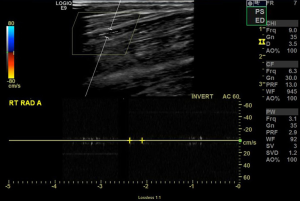
Computed tomography (CT) imaging of the head, chest, abdomen, and pelvis revealed bilateral pulmonary emboli, acute left occipital lobe CVA, and a right subclavian arterial embolus. CT angiography further showed occlusion of the distal left posterior cerebral artery. Doppler arterial ultrasound of the right upper extremity revealed occlusion of the right subclavian artery with absence of color flow and pulse Doppler signal distally (Figures 1 and 2). A continuous infusion of heparin was started. Vascular Surgery was consulted and performed an emergent embolectomy of the right subclavian artery. Orthopedic Surgery was consulted intraoperatively and performed preventative fasciotomy of the right upper extremity to prevent compartment syndrome. On repeat CT of the chest, a PFO was visualized. A transthoracic echocardiogram was performed, which revealed elevated pulmonary artery pressures.
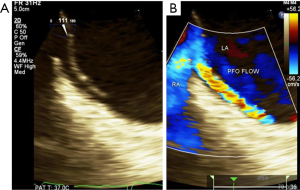
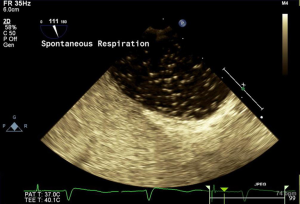
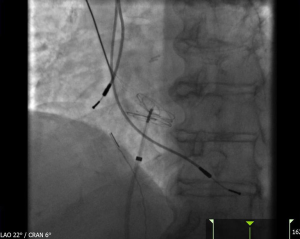
A TEE was performed and identified a large PFO with at least 3 mm primum/secundum separation and evidence of right to left shunting. An atrial septal aneurysm was also present (Figure 3). The TEE also revealed estimated left ventricular ejection fraction of 55–60%, normal right ventricular size and systolic function, and no visualization of a left atrial appendage thrombus. The passage of bubbles across the PFO was also visualized on TEE (Figure 4). A multidisciplinary evaluation including Cardiology and Neurology determined that the patient would benefit from closure of her PFO. After further discussions with the patient and her family, closure of the PFO was pursued. In the catheterization laboratory, a sizing balloon over a stiff wire was advanced to measure the size of the defect. With the use of intracardiac echocardiography, a 25-mm Cardioform device was successfully delivered across the defect (Figure 5). The patient tolerated the procedure well with no complications. Limited transthoracic echocardiogram post closure revealed no obvious evidence of PFO by color Doppler. She was started on oral anticoagulation in addition to aspirin and clopidogrel. She was subsequently discharged in stable condition.
Discussion
PFO has been demonstrated to be a significant risk factor for paradoxical embolization (4). This case represents a unique example of a patient with bilateral pulmonary emboli, acute CVA, and a right upper extremity embolus who was found to have a large PFO. As there is no definitive answer, the therapeutic options for this patient included medical therapy with antiplatelet and anticoagulants, percutaneous closure, or surgical repair of the PFO. After a comprehensive and multidisciplinary review, percutaneous repair of the PFO in addition to medical therapy with antiplatelets and anticoagulants were recommended to the patient.
Previously, evidence from clinical trials was conflicting in regard to the effectiveness of PFO closure. However, recent results from randomized clinical trials revealed that PFO closure is effective in reducing the risk of stroke in specific groups of patients. In the REDUCE trial, median follow-up of 3.2 years of patients randomly assigned to PFO closure combined with antiplatelet therapy or treatment with antiplatelet therapy alone revealed that clinical ischemic stroke occurred in less patients in the PFO closure group compared with the antiplatelet-only group (1.4% versus 5.4%, HR 0.23, 95% CI: 0.09–0.62) (5). The CLOSE trial randomized patients with cryptogenic stroke and PFO to antiplatelet therapy alone, oral anticoagulation, or PFO closure and antiplatelet therapy. The results revealed that at a mean follow-up of 5.3 years, there were no recurrent strokes among the patients in the PFO closure group compared to six percent among the patients in the antiplatelet-only group (HR 0.03, 95% CI: 0.0–0.26) (6). A median follow-up of 5.9 years of patients enrolled in the RESPECT trial showed that recurrent ischemic stroke occurred less frequently in the closure group compared with the medical therapy group (0.58% vs. 1.07% events per 100 patient-years, HR 0.55, 95% CI: 0.31–0.99) (7). Given the results from recent randomized controlled trials, percutaneous closure of a PFO is effective in reducing the risk of recurrent stroke. Our patient required treatment with anticoagulant therapy in addition to antiplatelet therapy given the presence of bilateral pulmonary emboli. The effectiveness of PFO closure in the setting of acute CVA, peripheral arterial embolus, and bilateral pulmonary emboli is to be determined.
Conclusions
In summary, increase in right-sided pressures from pulmonary embolus can cause right to left shunting and lead to a paradoxical embolus. Our patient presented with more than one paradoxical embolus including acute CVA and right subclavian embolus. Assessment of patients who present with acute CVA or arterial embolus in the setting of pulmonary emboli with elevated right atrial pressures should include a search for a PFO. Consideration of percutaneous PFO closure in this patient population should be of additive benefit to antiplatelets and anticoagulant therapy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc 1984;59:17-20. [Crossref] [PubMed]
- Meissner I, Whisnant JP, Khandheria BK, et al. Prevalence of potential risk factors for stroke assessed by transesophageal echocardiography and carotid ultrasonography: the SPARC study. Stroke Prevention: Assessment of Risk in a Community. Mayo Clin Proc 1999;74:862-9. [Crossref] [PubMed]
- Homma S, Sacco RL, Di Tullio MR, et al. Effect of medical treatment in stroke patients with patent foramen ovale: patent foramen ovale in Cryptogenic Stroke Study. Circulation 2002;105:2625-31. [Crossref] [PubMed]
- Foster PP, Boriek AM, Butler BD, et al. Patent foramen ovale and paradoxical systemic embolism: a bibliographic review. Aviat Space Environ Med 2003;74:B1-64. [PubMed]
- Søndergaard L, Kasner SE, Rhodes JF, et al. Patent Foramen Ovale Closure or Antiplatelet Therapy for Cryptogenic Stroke. N Engl J Med 2017;377:1033-42. [Crossref] [PubMed]
- Mas JL, Derumeaux G, Guillon B, et al. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med 2017;377:1011-21. [Crossref] [PubMed]
- Saver JL, Carroll JD, Thaler DE, et al. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. N Engl J Med 2017;377:1022-32. [Crossref] [PubMed]


