Occlusion of right coronary artery by microembolization caused by excessive diagnostic catheter manipulation
Introduction
Coronary angiography has always been the gold standard for diagnosis of coronary artery disease (CAD) (1). It is one of the most widely utilized procedure in modern cardiology (2). Coronary angiography has many diagnostic and therapeutic advantages, but due to its invasive nature, complications may occur (2-5). Of those complications, femoral artery access site complications, such as hematoma formation, pseudoaneurysm, and retroperitoneal bleeding are the most fraught (1,5,6). For so, there has been a recent paradigm shift towards radial artery access as an alternative to femoral access, due to its superficial location, ease of compressibility, decrease in recovery time, and reduced risk of distal ischemia (7). It also comes with its own challenges and complications. Excessive catheter manipulation, multiple catheter exchanges, radial artery spasm, and increased radiation time are more frequent in transradial catheterization (7,8). In this case report, we present a complication of right coronary artery (RCA) microembolization by endothelial debris following excessive catheter manipulation, due to tortuous right brachiocephalic artery.
Case presentation
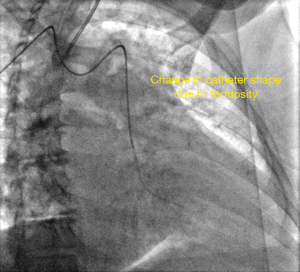
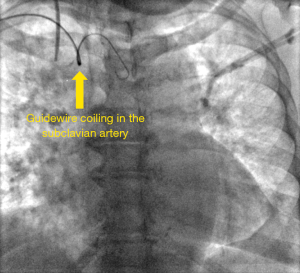
A 71-year-old African American woman presents with chest pain to outpatient cardiology clinic. Her chest pain was typical for angina pectoris. Due to her cardiovascular risk factors (age, essential hypertension, peripheral vascular disease, and diabetes mellitus), her pretest probability of CAD was determined to be high. She was referred for elective outpatient coronary angiography. On the day of her procedure, she had no symptoms. Her vital signs were normal, so was her electrocardiogram (EKG) on telemetry (Figure 1). The right radial artery was punctured without difficulty, followed by insertion of vascular sheath. A multi-purpose diagnostic catheter was utilized over a guide wire under fluoroscopic guidance through the right radial artery. It was smoothly advanced all the way to the right brachiocephalic artery without resistance. Further advance of the catheter beyond this point was met by resistance. Fluoroscopic imaging demonstrated coiling of the guide wire, confirming tortuosity of the brachiocephalic artery (Figure 2). After multiple attempts, the diagnostic catheter passed through the tortuous vessel, reaching the ascending aorta, but with deformed shape (Figure 3).
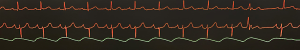
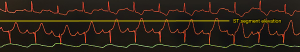
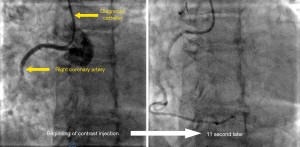
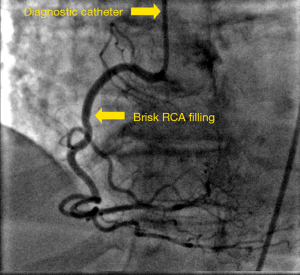
The left coronary artery was easily engaged first, but engaging the RCA required excessive manipulation of the catheter, further increasing procedure and fluoroscopy time. Repetitive sheath and catheter aspiration was performed multiple times to ensure patency. By the time RCA was engaged and contrast media injected, Patient started to complain of chest discomfort. Telemetry EKG showed ST segment elevation (Figure 4), followed by ventricular tachycardia (Figure 5), all consistent with myocardial ischemia. Angiography of the RCA revealed deep seated angiography catheter into the RCA, and very slow, intermittent and sluggish contrast flow that did not fully opacify the distal branches of the RCA. It took 11 seconds for the contrast to reach the distal end of the vessel (Figure 6). Soon after, Patient’s blood pressure and heart rate suddenly dropped, followed by increasing chest pain and mild confusion. Immediate right common femoral artery access was established, and Judkins Right 4 (JR4) catheter was used to engage the RCA, followed by intracoronary injection of 200 mcg of nitroglycerin. Patient’s chest pain started to improve, and vital signs stabilized shortly after. Multiple angiographic views of the RCA were obtained, showing brisk and complete opacification of the entire RCA course. It showed no angiographic evidence of CAD, or RCA dissection (Figure 7).
After this complicated procedure, the patient continues to complain of chest pain in the recovery area, similar in quality to the pain experienced during the procedure that was relieved by sublingual nitroglycerin. She was admitted to the hospital for supportive care. She was discharged the next morning in a good condition.
Discussion
Transradial coronary angiography has gained popularity over the past decade (6). According to the Cath-PCI National Cardiovascular Data Registry (NCDR), 36% of all cardiac catheterization performed in the US in 2016 were performed using transradial approach, compared to 16% in 2012, and 3% in 2007 (6). One of the most fraught challenges of transradial coronary angiography is tortuosity of brachiocephalic artery (6). This case report demonstrates that excessive catheter manipulation to overcome the tortuosity of the brachiocephalic artery can be associated with significant adverse outcomes.
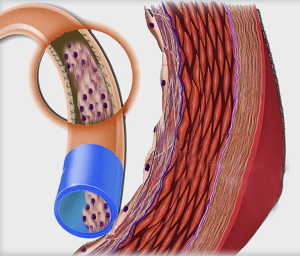
In this patient, the tortuous course of the right brachiocephalic artery increased procedure and fluoroscopy time. Vasospasm of the radial artery added up to the total resistance of catheter manipulation. As the catheter’s course became longer and more tortuous, catheter behavior and response to manipulation became less predictable. Manipulation of the catheter at the radial artery site did not get transmitted to the catheter tip as expected. Engagement of RCA was not optimal. Moreover, catheter tip interaction with the intimal wall of the brachiocephalic artery and ascending aorta caused accumulation of microcellular debris, fibrin, activated platelets, and cholesterol from shearing of the intimal endothelial cells and atherosclerotic plaques (Figure 8). Those debris can consolidate into large particulate clumps that adhere firmly to the luminal walls of the catheter. Particulate clumps are dependent on the duration and force of the catheter manipulation, the profile of the catheter, and use of guidewires. Routine flushing and aspiration may not clear the catheter from some particulate clumps. On the other hand, contrast injection at higher pressure and velocity can dislodge large amounts of those particulate clumps, causing clinically significant microemboli (9).
In 1967, when Judkins introduced transfemoral percutaneous coronary angiography technique, He recommended repetitive catheter aspiration and flushing in the descending aorta (9). However, with transradial cardiac catheterization gaining popularity, descending aorta is no longer a mandatory route for percutaneous coronary angiography. Recent prospective studies with diffusion-weighted magnetic resonance imaging have detected new small ischemic cerebral lesions after coronary angiography, with the incidence ranging between 5–22% (9-13). Most catheters nowadays are designed in less traumatic way, with the tip of the catheter angled in a way to minimize shearing the intimal wall (14). However, multipurpose catheter is a straight catheter that directly interacts with intimal wall. Use of straight catheters is associated with higher incidence of particulate cerebral or myocardial microembolization than angled catheters (12). Pre-shaped and angled catheters can also behave like a straight catheter if introduced over a guidewire, which straighten the catheter at its tip.
Mechanical and susceptibility factors are responsible for RCA microembolization in this patient. Tortuous right brachiocephalic artery, utilization of straight diagnostic catheter and use of guidewire to overcome tortuosity, excessive and prolonged catheter manipulation are all mechanical factors. Susceptibility factors include age, male gender, hypertension, diabetes, peripheral vascular disease, and high likelihood of aortic atherosclerosis. Certain precautionary measures should be taken to minimize the risk of microembolization. Using “the right catheter for the right patient” is important to minimize microembolization, and risk of arterial dissection. Frequent catheter aspiration and flushing, and avoiding excessive or forceful manipulation further reduce chance of debris build up inside the catheter, or around its tip, further minimizing the risk of embolization. Finally, early recognition of difficult transradial cardiac catheterization should be followed by early conversion to transfemoral route
Conclusions
Transradial cardiac catherization is now becoming the access route of choice for many cardiologists due to ease of access and compressibility, reduced cost and complication rate. However, tortuosity of the right brachiocephalic artery may result in difficulties passing the catheter through. Forceful and excessive manipulation of the diagnostic catheter to bypass brachiocephalic tortuosity is not recommended. Worsening arterial spasm, arterial dissection, and increased risk for cardiac or cerebral embolization are all fraught complications. Switching to transfemoral access is always recommended when transradial access is met by increased resistance due to tortuosity.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Louvard Y, Lefevre T, Allain A, et al. Coronary angiography through the radial or the femoral approach: The CARAFE study. Catheter Cardiovasc Interv 2001;52:181-7. [Crossref] [PubMed]
- Jolly SS, Amlani S, Hamon M, et al. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J 2009;157:132-40. [Crossref] [PubMed]
- Choussat R, Black A, Bossi I, et al. Vascular complications and clinical outcome after coronary angioplasty with platelet IIb/IIIa receptor blockade. Comparison of transradial vs transfemoral arterial access. Eur Heart J 2000;21:662-7. [Crossref] [PubMed]
- Esente P, Giambartolomei A, Simons AJ, et al. Overcoming vascular anatomic challenges to cardiac catheterization by the radial artery approach: specific techniques to improve success. Catheter Cardiovasc Interv 2002;56:207-11. [Crossref] [PubMed]
- Mann T, Cowper PA, Peterson ED, et al. Transradial coronary stenting: comparison with femoral access closed with an arterial suture device. Catheter Cardiovasc Interv 2000;49:150-6. [Crossref] [PubMed]
- Som S, Patel AK, Sethi V, et al. Barriers for transradial coronary angiography and interventions in 2016. Cardiovasc Revasc Med 2017;18:221-5. [Crossref] [PubMed]
- Cantor WJ, Mehta SR, Yuan F, et al. Radial versus femoral access for elderly patients with acute coronary syndrome undergoing coronary angiography and intervention: insights from the RIVAL trial. Am Heart J 2015;170:880-6. [Crossref] [PubMed]
- Carrillo X, Mauri J, Fernandez-Nofrerias E, et al. Safety and efficacy of transradial access in coronary angiography: 8-year experience. J Invasive Cardiol 2012;24:346-51. [PubMed]
- Judkins MP. Selective coronary arteriography. I. A percutaneous transfemoral technic. Radiology 1967;89:815-24. [Crossref] [PubMed]
- Busing KA, Schulte-Sasse C, Fluchter S, et al. Cerebral infarction: incidence and risk factors after diagnostic and interventional cardiac catheterization--prospective evaluation at diffusion-weighted MR imaging. Radiology 2005;235:177-83. [Crossref] [PubMed]
- Hamon M, Gomes S, Clergeau MR, et al. Risk of acute brain injury related to cerebral microembolism during cardiac catheterization performed by right upper limb arterial access. Stroke 2007;38:2176-9. [Crossref] [PubMed]
- Hamon M, Gomes S, Oppenheim C, et al. Cerebral microembolism during cardiac catheterization and risk of acute brain injury: a prospective diffusion-weighted magnetic resonance imaging study. Stroke 2006;37:2035-8. [Crossref] [PubMed]
- Lund C, Nes RB, Ugelstad TP, et al. Cerebral emboli during left heart catheterization may cause acute brain injury. Eur Heart J 2005;26:1269-75. [Crossref] [PubMed]
- Jurga J, Tornvall P, van der Linden J, et al. Guidewire withdrawal in ascending aorta increases cerebral microembolism during coronary angiography: a randomized comparison of two guidewire techniques. J Invasive Cardiol 2014;26:1-6. [PubMed]