The outcomes of percutaneous kyphoplasty in treatment of the secondary osteoporotic vertebral compression factures: a case-control study
Introduction
Osteoporotic fracture is one of the major global burdens of diseases (1-3). Osteoporotic fractures could occur in hip, vertebrae, and limbs. Osteoporotic vertebral compression fractures are mostly caused by the lower energy trauma or without trauma (4), and commonly in the elderly population. It was estimated that there were approximately 1.5 million vertebral compression fractures in US population every year (5). The European prospective osteoporosis study (6) found that the incidence of morphometric vertebral fracture was 10.7/1,000 person years (pyr) in women and 5.7/1,000 pyr in men and vertebral fracture as assessed qualitatively by the radiologist was 12.1/1,000 pyr and 6.8/1,000 pyr, respectively.
Percutaneous kyphoplasty or vertebroplasty was reported had effective outcomes in treatment of osteoporotic vertebral compression fractures (7-10), had advantages of minimally invasive, quicker recovery and shortening the hospital stay (11).
However, some patients will have the secondary vertebral compression fracture after the initial treatment (12,13), the secondary vertebral fracture may associate with severe spinal deformity and worse bone quality. The aim of this study is to investigate the outcomes of using percutaneous kyphoplasty in the treatment of the secondary osteoporotic vertebral compression fractures.
Methods
Patient population
From August 2008 to December 2014, a total of 81 patients had the secondary single segmental osteoporotic vertebral compression fractures after the initial fractures and treated by percutaneous kyphoplasty from two medical centers were recorded and reviewed, the secondary multiple segmental vertebral fractures were excluded to avoid the mixed influence, 74 out of 81 patients with minimum 2 years follow-up were included in this study. Then, the 74 patients with primary osteoporotic vertebral compression fractures treated by percutaneous kyphoplasty at the same time period were matched as control group in 1:1 ratio, the matched principles include: (I) the same gender; (II) age difference to the matched case is less than 3 years old; (III) single segmental vertebral fracture; (IV) followed up more than 2 years; (V) the surgeries were performed by the same surgeon.
Operative procedure
The operative procedure was similar to the Wu et al. (14). Briefly, the patients were placed at prone position under local anesthesia or general anesthesia. C-arm X-ray fluoroscope was used to guide the pedicle punctures and cement injection. Balloon tamps were used to expand the compressed vertebral body, the inflation was stopped when the pressure reached 300 psi or when the balloon made contact with the endplate. Polymethylmethacrylate cement was injected when it reached the “toothpaste” viscosity. All patients were permitted to ambulate at 12–24 hours after operation.
Pain and functional outcomes
Visual Analogue Scales (VAS) was used to assess the back pain at pre-operation, post-operation, and final follow-up; Oswestry Disability Index (ODI) was used to assess the functional outcomes at pre-operation, 3 months after operation, and the final follow-up.
Radiographic images
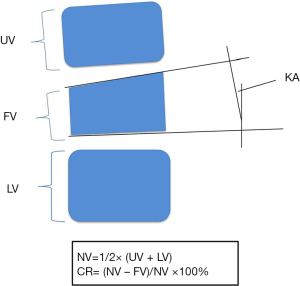
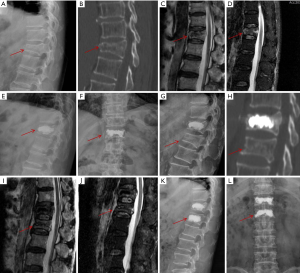
All of the radiographic images were assessed by two researchers for diagnosis (15) and measurement. The kyphotic angulation (KA) and anterior vertebral body height of fractured vertebrae, adjacent upper and lower vertebrae were measured on lateral X film at pre-operation, post-operation, and the final follow-up. The estimated normal anterior height of the fractured vertebra was calculated using the following formula: NV =1/2× (UV + LV), (NV: the estimated normal anterior height of the fractured vertebra; UV: the anterior height of the adjacent upper vertebrae above the fractured vertebra; LV: the anterior height of the adjacent lower vertebrae below the fractured vertebra). At the secondary fracture group, some patients had fracture of the adjacent vertebrae to initial fractured vertebrae, the UV and LV were measured at the second adjacent vertebrae. Then, the values of NV, UV and LV were used to calculate to the compression ratio (CR) of the anterior height of the fractured vertebra using following formula (16): CR = (NV − FV)/NV ×100% (FV: the anterior height of the fractured vertebrae) (Figure 1).
Statistical analysis
The data were analyzed with the software of IBM SPSS Statistics (Version 22.0, IBM Corp., Armonk, NY, USA). The data of pre-operation, post-operation (or 3 months after operation of ODI), and the final follow-up of VAS, ODI, KA, and CR were tested by the repeated-measures analyses of variance, and the comparison of two groups was tested by two independent-samples t-tests. The level of significance was set at P<0.05.
Results
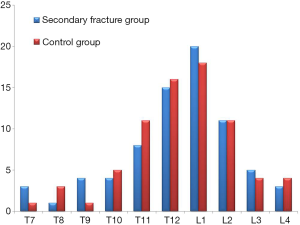
There were 26 males and 48 females at the secondary osteoporotic vertebral compression fractures groups, with the age of 74.3±10.8 years old, and followed up 37.5±12.9 months. Total 26 males and 48 females of primary osteoporotic vertebral compression fractures patients were matched as the control group, with the age of 74.6±10.4 years old, and followed up 40.9±16.3 months. No significant difference of age and follow up term between two groups (P=0.847 and 0.172, respectively). The segmental distribution of two groups was shown in Figure 2.
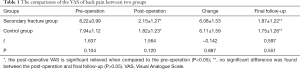
VAS and ODI outcomes
Both the secondary fracture group and control group had significantly relieved back pain after operation (P<0.05), with the changed VAS of 6.08±1.53 and 6.11±1.59, respectively. The relieved pain maintained at the final follow up, no significant difference was found between the post-operation and final follow up. No significant difference was found between two groups in VAS at pre-operation, post-operation and final follow-up either (Table 1).
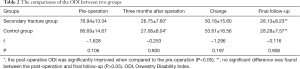
Full table
Both two groups had a significant improvement of ODI at 3 months after operation (P<0.05), with the changed values of 50.18±15.60 and 53.61±16.56, respectively. No significant difference was found between the post-operation and final follow up. No significant difference was found between two groups in ODI at pre-operation, post-operation and final follow-up either (Table 2).
Full table
Radiographic outcomes
Both two groups had significant corrections of KA and CR after operation (P<0.05) (Figure 3). The changed KA of secondary fracture group and control group was 8.29°±5.95° and 8.95°±7.22° (Table 3), respectively; the changed CR of secondary fracture group and control group was 25.59%±12.32% and 26.83%±13.44% (Table 4), respectively. No significant difference of KA and CR were found between the post-operation and the final follow-up. And no significant difference between two groups in KA and CR at pre-operation, post-operation and final follow-up either.
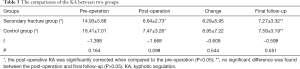
Full table

Full table
Discussion
Secondary osteoporotic vertebral compression fractures after the initial fractures are not rare condition (17). Lee et al. (18) followed up 198 patients for 4-year, found 34 (17.2%) of them had secondary osteoporotic vertebral compression fractures. Lindsay et al. (12) analyzed data of four large 3-year osteoporosis treatment trials that conducted at 373 centers in North America, Europe, Australia, and New Zealand; they found that the incidence of secondary vertebral fractures of the participants who had developed an initial incident vertebral fracture was 19.2% in the subsequent year.
Many factors may contribute to the secondary vertebral fractures, including age, lower bone mineral density, lower activity level after the first operation, and bone cement distribution (19-21). The finite element analysis showed cement augmented vertebral bodies had more than 12 times stiffer and 35 times stronger than the un-augmented level, therefore, increasing the pressure of adjacent levels (22), however, there is still no high quality evidence supporting vertebroplasty would increase the risk of secondary vertebral fracture, neither adjacent nor total vertebral fracture (23). Lin et al. (24) reported that the cement leakage into the disc would increase the risk of secondary fracture of the adjacent vertebral body, maybe it is also associated with the increased pressure on adjacent levels, to avoid the disc cement leakage may decrease the incidence of secondary vertebral fractures.
The prevention of secondary fractures after initial operation is also important. Black et al. (25) suggested that women with low bone mass and existing vertebral fractures, alendronate can reduce the frequency of morphometric and clinical vertebral fractures. The hormone-replacement therapy and parathyroid hormone (PTH) also can increase vertebral bone-mineral density (26). Proper intake of vitamin D, vitamin A, vitamin K, calcium and protein may also improve the bone-mineral density and reduce the risk of fracture (3,27-29).
However, once the secondary vertebral fractures happened, positive treatments would conduct. Conservative treatments have long-term bed rest, may induce further bone mineral loss, and high risk of deep vein thrombosis, pneumonia, urinary tract infection and pressure sores. Percutaneous vertebroplasty or kyphoplasty yielded faster, better pain relief and earlier ambulance (30-32). A prospective randomized controlled study conducted by Yang et al. (31), comparing the percutaneous vertebroplasty with the conservative treatment in treatment of the acute osteoporotic vertebral compression fractures, found that percutaneous vertebroplasty had much greater pain relief after operation, and fewer complications. Another randomized controlled study by Wardlaw et al. (10), found percutaneous kyphoplasty had better improvements in quality of life, disability measures and reduction of back pain than conservative treatment in follow-up time points <1 year, and trend to similar at 1 year, suggested percutaneous kyphoplasty is an effective and safe procedure and it could be considered as an early treatment option.
In our present study, all patients were permitted to ambulate at 12–24 hours after operation, the VAS of back pain was significantly relieved and the functional outcome was significantly improved after operation, the results were similar to the secondary fracture group and control group, we suggest the percutaneous kyphoplasty also has high-effective outcome for secondary vertebral fractures.
Both of percutaneous vertebroplasty and percutaneous kyphoplasty can significantly relieve the back pain and improve the function, however, percutaneous kyphoplasty with ball inflation may have a better correction of kyphosis. A systematic review and a meta-analysis (33) showed the kyphoplasty had lower risk of cement extravasation and greater correction of kyphosis than vertebroplasty. Since the secondary vertebral fracture associated with severe spinal deformity, therefore, we choose percutaneous kyphoplasty and hope it would be a better correction of kyphosis.
The limitations of this study include the nature of retrospective study, and non-randomized. All of the involved patients were single segmental vertebral fractures; therefore the results and conclusion of this study should be limited to interpret the secondary single segmental vertebral fractures. Moreover, the control patients were treated by percutaneous kyphoplasty too, therefore, we still cannot conclude the percutaneous kyphoplasty had a better correction of kyphosis than the percutaneous vertebroplasty; further percutaneous kyphoplasty vs. percutaneous vertebroplasty in the treatment of secondary vertebral fractures may need to be conducted.
Conclusions
Our findings suggest that percutaneous kyphoplasty is an effective and safe procedure for patients with secondary single segmental osteoporotic vertebral compression fractures; it can achieve similar clinical outcomes to the primary osteoporotic vertebral compression fractures.
Acknowledgements
Funding: This work was funded by the National Natural Science Foundation of China (81501933), Zhejiang Provincial Medical and Health Technology Foundation of China (2018KY129), Wenzhou leading talent innovative project (RX2016004) and Wenzhou Municipal Science and Technology Bureau (Y20170389).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by Institutional Review Board (IRB) (No. 2015-30) of Ninth People’s Hospital Shanghai Jiaotong University School of Medicine and The Second Affiliated Hospital and Yuying Children’s Hospital of the Wenzhou Medical University. Informed consent was obtained from all participants.
References
- Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009;301:513-21. [Crossref] [PubMed]
- Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002;359:1761-7. [Crossref] [PubMed]
- Wu AM, Huang CQ, Lin ZK, et al. The relationship between vitamin a and risk of fracture: meta-analysis of prospective studies. J Bone Miner Res 2014;29:2032-9. [Crossref] [PubMed]
- Ruiz Santiago FR, Tomás Muñoz PT, Moya Sánchez E, et al. Classifying thoracolumbar fractures: role of quantitative imaging. Quant Imaging Med Surg 2016;6:772-84. [Crossref] [PubMed]
- Alexandru D, So W. Evaluation and management of vertebral compression fractures. Perm J 2012;16:46-51. [Crossref] [PubMed]
- European Prospective Osteoporosis Study (EPOS) Group, Felsenberg D, Silman AJ, et al. Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 2002;17:716-24. [Crossref] [PubMed]
- Masoudi MS, Haghnegahdar A, Ghaffarpasand F, et al. Functional Recovery Following Early Kyphoplasty Versus Conservative Management in Stable Thoracuolumbar Fractures in Parachute Jumpers: A Randomized Clinical Trial. Clin Spine Surg 2017;30:E1066-73. [PubMed]
- Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 2010;376:1085-92. [Crossref] [PubMed]
- Wu AM, Chi YL, Ni WF. Vertebral compression fracture with intravertebral vacuum cleft sign: pathogenesis, image, and surgical intervention. Asian Spine J 2013;7:148-55. [Crossref] [PubMed]
- Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016-24. [Crossref] [PubMed]
- Phillips FM. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2003;28:S45-53. [Crossref] [PubMed]
- Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001;285:320-3. [Crossref] [PubMed]
- Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J 2010;19:1907-12. [Crossref] [PubMed]
- Wu AM, Lin ZK, Ni WF, et al. The existence of intravertebral cleft impact on outcomes of nonacute osteoporotic vertebral compression fractures patients treated by percutaneous kyphoplasty: a comparative study. J Spinal Disord Tech 2014;27:E88-93. [Crossref] [PubMed]
- Wáng YX, Santiago FR, Deng M, et al. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 2017;7:555-91. [Crossref] [PubMed]
- Wu AM, Ni WF, Weng W, et al. Outcomes of percutaneous kyphoplasty in patients with intravertebral vacuum cleft. Acta Orthop Belg 2012;78:790-5. [PubMed]
- Harrop JS, Prpa B, Reinhardt MK, et al. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty. Spine (Phila Pa 1976) 2004;29:2120-5. [Crossref] [PubMed]
- Lee DG, Park CK, Park CJ, et al. Analysis of risk factors causing new symptomatic vertebral compression fractures after percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures: a 4-year follow-up. J Spinal Disord Tech 2015;28:E578-83. [Crossref] [PubMed]
- Liu WG, He SC, Deng G, et al. Risk factors for new vertebral fractures after percutaneous vertebroplasty in patients with osteoporosis: a prospective study. J Vasc Interv Radiol 2012;23:1143-9. [Crossref] [PubMed]
- Bae JS, Park JH, Kim KJ, et al. Analysis of risk factors for secondary new vertebral compression fracture following percutaneous vertebroplasty in patients with osteoporosis. World Neurosurg 2017;99:387-94. [Crossref] [PubMed]
- Oei L, Koromani F, Rivadeneira F, et al. Quantitative imaging methods in osteoporosis. Quant Imaging Med Surg 2016;6:680-98. [Crossref] [PubMed]
- Baroud G, Nemes J, Heini P, et al. Load shift of the intervertebral disc after a vertebroplasty: a finite-element study. Eur Spine J 2003;12:421-6. [Crossref] [PubMed]
- Han SL, Wan SL, Li QT, et al. Is vertebroplasty a risk factor for subsequent vertebral fracture, meta-analysis of published evidence? Osteoporos Int 2015;26:113-22. [Crossref] [PubMed]
- Lin EP, Ekholm S, Hiwatashi A, et al. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 2004;25:175-80. [PubMed]
- Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 1996;348:1535-41. [Crossref] [PubMed]
- Lindsay R, Nieves J, Formica C, et al. Randomised controlled study of effect of parathyroid hormone on vertebral-bone mass and fracture incidence among postmenopausal women on oestrogen with osteoporosis. Lancet 1997;350:550-5. [Crossref] [PubMed]
- Lv QB, Gao X, Liu X, et al. The serum 25-hydroxyvitamin D levels and hip fracture risk: a meta-analysis of prospective cohort studies. Oncotarget 2017;8:39849-58. [Crossref] [PubMed]
- Cockayne S, Adamson J, Lanham-New S, et al. Vitamin K and the prevention of fractures: systematic review and meta-analysis of randomized controlled trials. Arch Intern Med 2006;166:1256-61. [Crossref] [PubMed]
- Wu AM, Sun XL, Lv QB, et al. The Relationship between Dietary Protein Consumption and Risk of Fracture: a subgroup and dose-response meta-analysis of prospective cohort studies. Sci Rep 2015;5:9151. [Crossref] [PubMed]
- Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1408-16. [Crossref] [PubMed]
- Yang EZ, Xu JG, Huang GZ, et al. Percutaneous vertebroplasty versus conservative treatment in aged patients with acute osteoporotic vertebral compression fractures: a prospective randomized controlled clinical study. Spine (Phila Pa 1976) 2016;41:653-60. [Crossref] [PubMed]
- Farrokhi MR, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine 2011;14:561-9. [Crossref] [PubMed]
- Papanastassiou ID, Phillips FM, Van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 2012;21:1826-43. [Crossref] [PubMed]