Abnormal chest X-ray leading to diagnosis of partial anomalous pulmonary venous connection
Introduction
Partial anomalous pulmonary venous connection (PAPVC) is a rare condition that often goes undiagnosed due to lack of symptoms and is sometimes diagnosed during cardiac work-up for other abnormalities or, like in our case, during radiologic examination for unrelated illness. However, depending on the number of pulmonary veins involved and the degree of left-to-right shunting, patients may develop serious complications including right-sided heart failure and cardiac arrhythmias. Maintaining clinical suspicion based on subtle clinical and radiologic findings is important as early recognition can prevent long-term complications such as pulmonary hypertension and heart failure. We present a case of PAPVC, which, like most cases, was discovered incidentally on imaging.
Case presentation
A 45-year-old man with a longstanding psychiatric history including schizophrenia, anxiety, and depression, was brought to the hospital after he attempted suicide via carbon monoxide poisoning by leaving his car running in his closed garage. He was found within minutes of his attempted suicide and remained conscious and alert throughout the initial examination. Vital signs were within normal limits. He was anxious but in no distress and denied any headache, dizziness, nausea, vomiting, chest pain, or difficulty breathing. Physical examination including cardiovascular examination was within normal limits except for bilateral lower extremity edema, which he reported as chronic. Routine complete blood count and comprehensive metabolic panel were normal. Urine drug screen was positive for benzodiazepine and phencyclidine. Arterial blood gas showed a carboxyhemoglobin level of 4.3%. He was admitted to the psychiatric unit for further management.
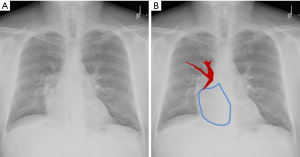
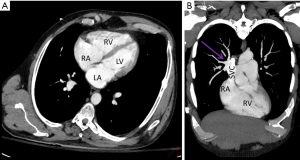
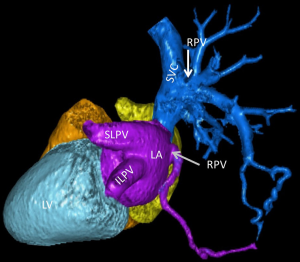
A routine chest X-ray revealed a slightly enlarged cardiac silhouette with right atrial enlargement, as well as an apparently enlarged right hilum (Figure 1). An electrocardiogram was normal. Due to the abnormal chest X-ray findings, the radiologist reviewed prior radiologic studies in the patient’s record and found a contrast-enhanced chest computer tomogram (CT) that was performed for an unrelated motor vehicle accident 3 years previously. His prior chest CT had been interpreted as Scimitar syndrome. However, our radiologist disputed this interpretation, suggesting isolated PAPVC without venous return to the inferior vena cava (IVC) (Figures 2,3). The patient was unaware of these previous findings and had never been seen by a cardiologist. A transthoracic echocardiogram showed right atrial and ventricular dilation with moderately reduced right ventricular (RV) systolic function and a pulmonary artery systolic pressure of 32.5 mmHg. He remained in the psychiatric unit with plans for outpatient cardiology follow-up and a cardiac magnetic resonance imaging (MRI) to further evaluate myocardial anatomy. To date, he has failed to follow up as an outpatient.
Discussion
The pulmonary venous system normally consists of four veins draining into the posterior wall of the left atrium. Embryologically, the common pulmonary vein (CPV) develops from the splanchnic plexus and grows toward the right and left lung buds before branching into two right and two left pulmonary veins. PAPVC occurs when one or more, but not all, pulmonary veins drain into the systemic circulation via either a direct connection to the right atrium or indirectly through a variety of venous connections such as the innominate vein or the superior vena cava (SVC) (1).
PAPVC has a reported incidence of 0.7%. However, as this congenital defect is commonly asymptomatic and only found during autopsy, the incidence is likely higher (2-4).
Generally, no hemodynamic abnormality or clinical symptoms are noted unless 50% or more of the pulmonary blood flow is re-directed to the pulmonary vasculature (5). Thus, individuals with a single anomalous pulmonary vein usually are asymptomatic and have a normal life span. Presentation in later life is often an incidental finding. However, PAPVC may also cause significant left-to-right shunting leading to RV dysfunction and pulmonary hypertension. Symptomatically, these patients present with dyspnea on exertion, and, more rarely, atrial arrhythmias, right heart failure and pulmonary hypertension. Diagnosis is confirmed with echocardiogram and cardiac CT. Cardiac MRI can further elucidate anatomy.
Surgical management is reserved for persons with a hemodynamically significant left-to-right shunt (a ratio of pulmonary to systemic flow greater than 2:1), those with recurrent pulmonary infections, or during surgical repair of other major cardiac lesions (6-8).
The Scimitar syndrome is a variant of PAPVC in which part or even the entire right lung is drained by right pulmonary veins that connect anomalously to the IVC and comprises 3–5% of all cases of PAPVC (9,10). Findings on chest radiography include a hypoplastic lung with ipsilateral mediastinal shift and the anomalous draining vein, which may resemble the characteristic shape of a “scimitar” as it takes a curvilinear course towards the IVC (11).
There are multiple published single-institution reviews that analyzed the accuracy of CT in detecting anomalous pulmonary venous connection. Jujo et al. (12) retrospectively analyzed patients who had PAPVC diagnosed after right heart catheterization for pulmonary hypertension. Many of these patients had chest CTs performed as part of the work-up for their pulmonary hypertension. While CT was found to be useful in characterizing the anatomy, the number of variants in pulmonary venous drainage and rare nature of the findings may be a cause of misinterpretation (12). Unfortunately, the exact rate at which anomalous pulmonary veins are overlooked is unknown, and there is little information on this in the literature.
With the growing use of imaging to both aid in diagnosis and treatment in patients with multiple comorbidities, it is important for clinicians and radiologists to become familiar with finding and evaluating congenital anomalies in adults. This case demonstrates the importance of accurately diagnosing anomalous venous connections on imaging, as they are primarily incidental findings but can have significant clinical impact. It is, therefore, crucial that once diagnosed, patients maintain follow-up with a cardiologist to monitor for signs of cardiac dysfunction.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent cannot be obtained from this patient because his location is unknown and is not indicated. There is no possible way that this patient could be identified by reading the case report or by looking at the three figures.
References
- Najm HK, Williams WG, Coles JG, et al. Scimitar syndrome: twenty years' experience and results of repair. J Thorac Cardiovasc Surg 1996;112:1161-8; discussion 1168-9. [Crossref] [PubMed]
- Lapa T, Vedelgo J, Kim H, et al. An unusual constellation of congenital malformations in a single patient including partial anomalous venous return, persistent left superior vena cava, aberrant pulmonary fistula, anomalous aortic arch, tracheal diverticulum and annular pancreas. BMJ Case Rep 2014;2014. [Crossref] [PubMed]
- Healey JE Jr. An anatomic survey of anomalous pulmonary veins: their clinical significance. J Thorac Surg 1952;23:433-44. [PubMed]
- Garduno C, Chew S, Forbess J, et al. Persistent left superior vena cava and partial anomalous pulmonary venous connection: incidental diagnosis by transesophageal echocardiography during coronary artery bypass surgery. J Am Soc Echocardiogr 1999;12:682-5. [Crossref] [PubMed]
- Chemin A, Bonnet D, Le Bourgeois M, et al. Respiratory outcome in children with scimitar syndrome. J Pediatr 2013;162:275-9.e1. [Crossref] [PubMed]
- Miwa K, Takamori S, Hayashi A, et al. Incidental partial anomalous pulmonary venous connection in left lung cancer. Jpn J Thorac Cardiovasc Surg 2004;52:189-90. [Crossref] [PubMed]
- Brody H. Drainage of the pulmonary veins into the right-side of the heart. Arch Pathol 1942;33:130.
- Sasaki H, Naka N, Kitahara N, et al. Right partial anomalous pulmonary venous connection found during lobectomy for coexisting lung cancer and tuberculosis: report of a case. Clin Lung Cancer 2006;7:350-2. [Crossref] [PubMed]
- Weiman DS, Lee K, Levett JM, et al. Partial anomalous pulmonary venous return: a ten-year experience. Tex Heart Inst J 1985;12:239-43. [PubMed]
- Huddleston CB, Exil V, Canter CE, et al. Scimitar syndrome presenting in infancy. Ann Thorac Surg 1999;67:154-9; discussion 160. [Crossref] [PubMed]
- Sobrinho G, Salcher J. Partial anomalous pulmonary vein drainage of the left lower lobe: incidental diagnostic after central venous cannulation. Crit Care Med 2003;31:1271-2. [Crossref] [PubMed]
- Jujo T, Tanabe N, Sugiura T, et al. Importance of carefully interpreting computed tomography images to detect anomalous pulmonary venous return. Respir Investig 2016;54:69-74. [Crossref] [PubMed]


