A critical electrocardiographic pattern in the age of cardiac biomarkers
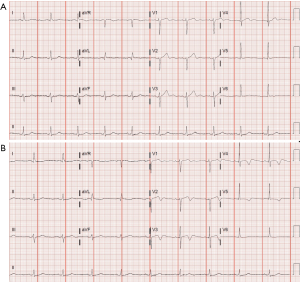
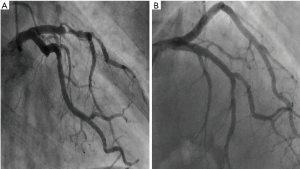
We have read with great interest the article by Abuarqoub et al., concerning an interesting finding associated with a Wellens’ pattern (1). Contemporary data highlights the importance of cardiac biomarkers in the assessment of individuals with suspected coronary artery disease, presenting to the emergency department (ED) (2). In addition to these biomarkers, however, certain electrocardiographic patterns may also be of great relevance in the management of these patients, allowing prompt identification of individuals at higher risk. We report the case of a 71-year-old man who presented to the ED due to oppressive chest pain. He reported recurrent bouts of paroxysmal chest pain with 1 month evolution, without a clear association with physical effort. He was a current smoker, had arterial hypertension and a prior history of cerebrovascular disease, but no record of previous cardiac events. At admission he was symptomatic, hemodynamically and electrically stable, and his physical examination was unremarkable (showing no signs of pulmonary or peripheral congestion). His admission electrocardiogram (ECG; Figure 1A) showed sinus rhythm and unspecific ST-T changes, and he became asymptomatic after administration of lysine acetylsalicylate. His blood tests were unremarkable, except for a mildly elevated high-sensitivity cardiac troponin T (36 ng/L, with a reference value of 5–14 ng/L). Two hours after admission, he remained asymptomatic and clinically stable, and a second ECG was taken (Figure 1B). Given the history and cardiac biomarker elevation this was a case consistent with an acute coronary syndrome. This patient’s ECG, however, was typical of a Wellens’ syndrome (3,4). This classical pattern, first described by de Zwaan et al. is highly associated with a left anterior descending (LAD) artery stenosis (3). Given this data, this patient was admitted to a coronary care unit for early invasive stratification. In the first hours after admission he developed recurring chest pain and was referred for emergent cardiac catheterization, which documented a 90% stenosis in the mid portion of the LAD (Figure 2A). The lesion was treated with a drug-eluting stent (Figure 2B), and the patient was subsequently asymptomatic. His remaining hospitalization was uneventful, and his echocardiogram (prior to discharge) showed a preserved left ventricular systolic function.
This case illustrates the importance of recognizing a specific ECG pattern. In the case presently reported cardiac troponin was mildly elevated (reaching a peak of 98 ng/L during hospitalization), but this pattern has also been described in individuals with different patterns of cardiac biomarker expression (including normal levels) (3,5). Also, as described in the recent article by Abuarqoub et al., clinical presentation may be protean, thus rendering knowledge of this pattern paramount for the clinician involved in emergency care (1,6).
In conclusion, the presence of a Wellens’ pattern is highly suggestive of LAD disease. The early identification of these patients can allow timely and adequate therapeutic strategies, thus greatly improving their clinical course.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abuarqoub A, Naranjo M, Shamoon F. Myocardial bridging with left ventricular hypertrophy presenting as Wellens pattern. Ann Transl Med 2017;5:401. [Crossref] [PubMed]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315. [Crossref] [PubMed]
- de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J 1982;103:730-6. [Crossref] [PubMed]
- Ayer A, Terkelsen CJ. Difficult ECGs in STEMI: lessons learned from serial sampling of pre- and in-hospital ECGs. J Electrocardiol 2014;47:448-58. [Crossref] [PubMed]
- Coutinho Cruz M, Luiz I, Ferreira L, et al. Wellens' Syndrome: A Bad Omen. Cardiology 2017;137:100-3. [Crossref] [PubMed]
- Yasin OZ, Rubio-Tapia A, Sarano ME. Wellens Syndrome with Syncope but Not Chest Pain. Cardiology 2017;137:9-13. [Crossref] [PubMed]