Management of ruptured liver segment IV hepatocellular carcinoma: is transarterial embolization (TAE) superior to chemoembolization (TACE)?—the jury is still out
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer worldwide and the second most common cause of cancer-related death (1). Presentation of patients with HCC varies from early stage, asymptomatic patients to advanced infiltrative lesions that may cause symptoms (1,2). It is true that incidence of HCC correlates with that of chronic hepatitis B and C that quite often lead to the development of cirrhosis, a well-known risk factor for HCC (3).
Spontaneous rupture of HCC is a feared complication of HCC with a variable reported incidence worldwide; less than 3% in Western world and up to 26% of patients in the East. Owing to a possible HCC-related vascular dysfunction and coagulopathy, ruptured HCC (rHCC) should be considered a potentially life-threatening complication. Several treatment approaches have been suggested, namely transarterial embolization (TAE)/transarterial chemoembolization (TACE), emergent hepatectomy, staged hepatectomy and conservative methods, each decided upon according to the status of the patient (4,5).
Nevertheless, no strict guidelines have been developed to date for the implementation of the appropriate treatment plan on each occasion. Herein, we present a 66-year-old woman with a 7.6-cm maximum diameter HCC that ruptured freely in the peritoneal cavity and caused acute abdominal pain. The purpose of this report is to present the advantages of TAE in treating huge rHCC; TAE effectively stopped the hemorrhage and tumor showed an impressive response to TAE; significant, gradual HCC necrosis that permitted an uneventful resection of liver segment IV at a later stage.
Case presentation
A 66-year-old woman of Greek origin was admitted to our department with sudden right upper quadrant abdominal pain and dizziness. Her past medical history included diagnosis of chronic hepatitis B and cirrhosis ten years ago, smoking, hypertension and paroxysmal supraventricular tachycardia, whereas she had undergone an open right oophorectomy for pelvic inflammatory disease 10 years ago. On arrival, the patient was alert, with a heart rate of 115 bpm and a blood pressure of 100/65 mmHg. Physical examination revealed guarding of epigastrium with the following laboratory values: Hb: 6.8 g/dL, WBCs: 9,310 k/µL, PLT: 166 k/µL, serum total bilirubin: 0.49 mg/dL, INR: 1.08 and serum albumin: 4 (Child-Pugh class A liver function). The levels of carcinoembryonic antigen (CEA), carcinoma 19-9 and A-fetoprotein (AFP) were 4.1 ng/dL, 13.7 U/mL and 12.2 ng/mL, respectively.
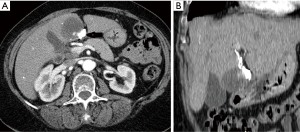
The contrast enhanced computer tomography (CT) of the abdomen revealed a large exophytic heterogeneously attenuating mass with a maximum-diameter of 7.6 cm arising from segment IV (Figure 1). Tumor vascular supply was mainly by one left hepatic artery main branch. There was focal discontinuity of the hepatic surface and a hyper-intense perihepatic hematoma. Collectively, these findings suggested a spontaneous rupture of a possible HCC.

After consensus of a multidisciplinary team, primary interventional hemostasis was decided by TAE. A catheter was introduced into the celiac trunk via the right transfemoral approach and selective celiac angiogram revealed one feeder vessel arising from the left hepatic artery that was eventually embolized using microspheres. The patient remained stable after the procedure.
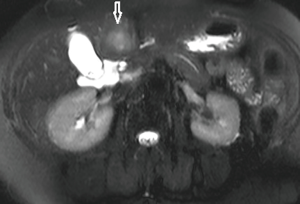
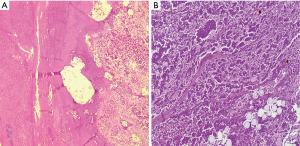
One month after embolization, contrast-enhanced abdominal CT showed disappearance of the intratumoral arterial enhancement and reduction of the mass to 5.3 cm maximum diameter (Figure 2) There was no evidence of metastatic disease. Six months after embolization, upper abdominal MRI showed a smaller (m.d. 4.3 cm) hypo-intense lesion on both T1 and T2-weighted images (Figure 3). A formal resection of segment IV was planned. There was an extensive and very obvious necrosis of the tumor macroscopically. The histopathological examination showed replacement of the HCC by a necrotic material that was surrounded by a fibrous tissue (Figure 4).
Her postoperative recovery was complicated with a small abscess on the resection bed that was treated conservatively. One year after the operation, she is still alive, in good condition with no evidence of residual disease. She is monitored at the hepatologic clinic of our hospital because she was diagnosed with chronic hepatitis B.
Discussion
To date, no strict guidelines have been proposed regarding the management of rHCC. Therefore, rHCC apart from being a life-threatening condition, poses significant dilemmas concerning the appropriate therapeutic approach. It is imperative that all patients initially receive intravenous fluid resuscitation, supportive care and blood products after their admission (6). Hemostasis may be achieved in different ways. Conservative treatment, which is applied in 22.6% of rHCCs, increases the risk of recurrent bleeding but can be useful in hemodynamically stable patients or those with a prohibitively poor prognosis that can only receive palliative care. Thirty two percent (32%) of patients are treated with emergency TACE and only 4% with emergency TAE. The rates of emergency surgical treatment have been reduced to 10% due to massive blood loss and poor oncological results (5).
TAE or TACE of the bleeding tumor seems to be a life-saving method for stabilization of patient. The success rates of TAE for hemostasis in a very recent review by Yoshida et al. ranges from 53% to 100%. Despite the temporary stabilization, 30-days mortality rates overcome 25%. The stage of cirrhosis, severity of shock and cancer stage are some of the crucial predictors of survival (4). Given that rHCC practically means dissemination of the tumor burden, the American Joint Committee on Cancer/Union for International Cancer Control (AJCC/UICC) has staged rHCC as T4 lesion, similar to tumors with vascular or bile duct invasion (7).
The definite treatment of HCC after addressing the urgency of the situation will be decided after re-evaluating the patient’s condition and restaging of the disease (6). Elective hepatectomy may be considered an effective strategy with improved long-term survival, for patients with ruptured resectable HCC after determining the effectiveness of the above methods and represents the 16% of therapeutic strategies (4-6).
During the reevaluation period of our patient, it was found that TAE had resulted in significant tumor necrosis, disappearance of any intratumoral arterial enhancement and 4-fold volume decrease. It is an original report of histologically confirmed complete response after TAE, according to modified RECIST assessment for HCC (8). In a recent clinical study, technical success and complete response after bland embolization in patients with unresectable HCC were achieved only at a percentage of 7% (9). On the other hand, in a cohort study of 176 consecutive cirrhotic patients with single HCC, TAE/TACE achieved a complete necrosis at a rate of 13% for lesions of 6 cm and above (10).
Bibliography stands equivocal about the differences in the efficacy of TAE versus TACE with regard to tumor response and survival rates. A metanalysis with three RCTs demonstrated no difference in survival between TAE and TACE for HCC, despite the absence of statistical heterogeneity among the studies (11). A more recent metanalysis from seven trials with low risk of bias showed no significant effect of either TACE or TAE on survival but was not considered possible to compare the tumor response (12). No difference in complete response was found in a single tertiary randomized trial of Hepatic Artery Embolization for HCC using Doxorubicin-Eluting microspheres compared with TAE with microspheres alone (13). It is, therefore, evident that no definite conclusions can be drawn from the results of the aforementioned studies and meta-analyses given the risks of biases, different methodology and different assessment of response to therapy of each individual study. Thus, there is a great need for the conduction of future multicenter studies in the field comparing the two methods aiming at the formulation of strict guidelines pertaining to all scenarios.
Conclusions
In conclusion, the advantage of TAE over TACE for ruptured HCC has not yet been determined. Ischemic effect of the treatment itself seems to be responsible for tumor response. Our experience suggests that TAE followed by elective hepatectomy could be an efficient approach for patients with Child-Pugh class A liver function and adequate liver remnant. More studies are needed in order to construct specific guidelines for the treatment of rHCC that will be based on the disease severity and the patient status.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Choo SP, Tan WL, Goh BK, et al. Comparison of hepatocellular carcinoma in Eastern versus Western populations. Cancer 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Benson AB 3rd, D'Angelica MI, Abbott DE, et al. NCCN Guidelines Insights: Hepatobiliary Cancers, Version 1.2017. J Natl Compr Canc Netw 2017;15:563-73. [Crossref] [PubMed]
- Kudo M. Surveillance, diagnosis, treatment, and outcome of liver cancer in Japan. Liver Cancer 2015;4:39-50. [Crossref] [PubMed]
- Yoshida H, Mamada Y, Taniai N, et al. Spontaneous ruptured hepatocellular carcinoma. Hepatol Res 2016;46:13-21. [Crossref] [PubMed]
- Moris D, Chakedis J, Sun SH, et al. Management, outcomes, and prognostic factors of ruptured hepatocellular carcinoma: A systematic review. J Surg Oncol 2018;117:341-53. [Crossref] [PubMed]
- Zhong F, Cheng XS, He K, et al. Treatment outcomes of spontaneous rupture of hepatocellular carcinoma with hemorrhagic shock: a multicenter study. Springerplus 2016;5:1101. [Crossref] [PubMed]
- American Joint Committee on Cancer. Cancer Staging Manual. New York: Springer, 2009.
- Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 2010;30:52-60. [Crossref] [PubMed]
- Bonomo G, Pedicini V, Monfardini L, et al. Bland embolization in patients with unresectable hepatocellular carcinoma using precise, tightly size-calibrated, anti-inflammatory microparticles: first clinical experience and one-year follow-up. Cardiovasc Intervent Radiol 2010;33:552-9. [Crossref] [PubMed]
- Miraglia R, Pietrosi G, Maruzzelli L, et al. Efficacy of transcatheter embolization/chemoembolization (TAE/TACE) for the treatment of single hepatocellular carcinoma. World J Gastroenterol 2007;13:2952-5. [Crossref] [PubMed]
- Marelli L, Stigliano R, Triantos C, et al. Transarterial therapy for hepatocellular carcinoma: which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc Intervent Radiol 2007;30:6-25. [Crossref] [PubMed]
- Oliveri RS, Wetterslev J, Gluud C. Transarterial (chemo)embolization for unresectable hepatocellular carcinoma. Cochrane Database Syst Rev 2011. [PubMed]
- Brown KT, Do RK, Gonen M, et al. Randomized trial of hepatic artery embolization for hepatocellular carcinoma using doxorubicin-eluting microspheres compared with embolization with microspheres alone. J Clin Oncol 2016;34:2046-53. [Crossref] [PubMed]


