How to measure quality in endoscopic retrograde cholangiopancreatography (ERCP)
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is an endoscopic technique that was developed in the 1960’s to diagnose pancreatobiliary pathology. Since its introduction it has evolved from a purely diagnostic to predominately therapeutic procedure. It established as one of the most demanding and technically challenging procedures in gastrointestinal endoscopy, requiring a specific training and learning curve to master. In the recent years multiple guidelines on measuring quality in ERCP have been published. The internet era had made it widely available for patients to research and ask about the level of success of their operator in performing the procedure and complication rates. Until recently complication rate was the only measure to evaluate outcome, because ERCP is associated with greater morbidity and mortality when compared to other endoscopic procedures such as colonoscopy and gastroscopy. It shortly became obvious that additional measures must be established to evaluate quality in ERCP.
Following the necessity for additional measures American Society of Gastrointestinal Endoscopy (ASGE) held consensus conference in 2001 in attempt to identify measures that will be helpful in tracing the outcomes of endoscopists in everyday practice. They divided the measures into three groups structure, process and outcomes. Where structure represent pre-procedure patient-endoscopist characteristics, process represents the technical aspect of ERCP and outcome assesses the patient after the procedure. This conference was the benchmark for all later developed guidelines.
The most renown ASGE and European Society of Gastrointestinal Endoscopy (ESGE) guidelines on quality measures have as a back-bone the same measures divided to pre-procedure, intraprocedure and post procedure (1,2).
Pre-procedure period
Pre-procedure period includes the contact of the patients with endoscopy staff members before the admission of sedation. In this period patient must be informed about the risks and technical aspects of the procedure and sign an informed consent. This is the period when the team involved with the procedure establishes a plan for approximate duration appropriate sedation, and decision towards prophylactic antibiotics administration (3). Endoscopists and other staff members may discuss expected outcome from the procedure and assume about duration which may vary depending on procedure difficulty. Establishing a plan and communication in team is essential for sedation duration and improves quality.
Informed consent
Informed consent must focus on the risk associated with endoscopic procedures and ERCP in particular. Adverse events should be explained clearly and be focused on minimum of six possible outcomes: pancreatitis, hemorrhage, infection, cardiopulmonary events, allergic reaction and perforation. Patients should be informed about the adverse events of the procedure, that the procedure may not be successful, and may be a second procedure will be required. Furthermore, it should be made clear the adverse events of ERCP are sometimes different and unique from these in standard endoscopy.
Indications for ERCP and documentation of the procedure
It is well known and established rule that ERCP must be performed for appropriate indications (4-6). As general rule of thumb when performing ERCP without appropriate indications the risk for developing complications is significantly higher. An appropriate indication should be documented for each procedure, and when it is an uncommon indication the reasons for this should be made clear in the documentation. Table 1 contains a list of the vast majority of acceptable indications for ERCP.
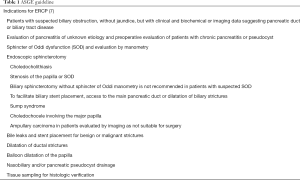
Full table
Clinical settings in which ERCP is generally not indicated include abdominal pain without clear evidence of pancreaticobiliary disease based on laboratory or noninvasive imaging studies (8,9). Routine ERCP prior to cholecystectomy without biliary obstruction, cholangitis and bile duct stones (7,10). Relief of malignant biliary obstruction in potentially resectable patients. Despite the evidence in literature that ERCP must be performed for appropriate indications and should not be performed in the abovementioned scenarios, the procedure is still widely used for diagnostic purposes and preoperative biliary drainage for biliary decompression, especially in developing countries where magnetic resonance cholangiopancreatography is not widely available and expensive (11). Preoperative drainage is warranted only in patients in whom surgery will be delayed due to neoadjuvant therapy or other preoperative assessment treatments. Those cases are considered as appropriate care.
Prophylactic antibiotics
Pre-procedure antibiotics should be considered in patients with clinical and/or laboratory signs of cholangitis or in those with suspected biliary obstruction in whom complete drainage of the biliary tree could not be achieved (12).
Finally, ERCP should be performed by an endoscopist who is fully trained and certified for the procedure. Case volume is directly associated with success rate and complications and must be recorded. Study from Austria showed that endoscopists with 50 annual ERCPs had lower success rates and more adverse events during ERCP than physicians with higher procedure volumes (13). However, results from the Rotterdam self-assessment form put that thesis in doubt (see below). Furthermore, a metanalysis including nine studies, 137 trainees and 17,100 ERCP procedures, concluded a vast difference in number of procedures needed for achieving competency. The numbers were between 79 and 400 procedures. Therefore, the structure of the advanced endoscopy training programs must be reassessed to ensure that procedural competency is being achieved (14).
The intraprocedure period
The intraprocedure period of ERCP is the period from the beginning of the procedure and administration of the anesthetic to withdrawing the endoscope. This period includes documentation of technical aspects of the procedure and patient monitoring (3).
Sedation
The use of sedation for endoscopy is rapidly evolving in the recent years mainly because of the need to improve patient comfort, satisfaction and safety while improving efficiency of endoscopy. General rules when using sedation in endoscopy includes periodical assessment and documentation of vital signs at a frequency that depends on the administrated medication, duration of the procedure and condition of the patient. Equipment and medications for emergency resuscitation should be available. Patient monitoring requirements include electronic assessment of blood pressure, heart rate, pulse oximetry and visual assessment of ventilatory activity and consciousness by trained specialist.
Selected group of patients may be able to undergo endoscopic procedure without sedation. This group includes elderly people with comorbidities and contraindications for sedation, not anxious patients and without history of abdominal pain. Usually in these cases small diameter endoscopes (nasoendoscope or pediatric gastro/colonoscope) are used to improve tolerability and patient comfort. In addition, the use of water and CO2 insufflation may improve patients overall experience and reduce pain induced by the procedure (15,16). As a general rule even in unsedated endoscopy, a periphery venous way should be available in case cardiopulmonary unplanned event occur and sedation is required.
A significant factor facilitating sedation is introduction of new agents such as propofol which allows rapid induction of deep sedation and post procedural recovery (17). Recent metanalysis comparing propofol with other traditional sedation agents used in endoscopy, including 22 randomized control trials and 1,798 patients review its safety and effectiveness. The metanalysis concluded that propofol usage is associated with shorter recovery and discharge periods, better sedation and patient cooperation without un increase in cardiopulmonary complications. There was no difference in patient’s satisfaction compared with traditional sedative agents.
ERCP is a complex procedure that usually takes longer to perform than routine gastro/colonoscopy. Recent study evaluating patients undergoing ERCP under conscious sedation revealed that half of patients experienced pain and discomfort during the procedure and peri-procedural period (18). Other study showed that failure rate of ERCP was double (14% vs. 7% when conscious sedation was used compared to general anesthesia. This higher failure rate was due to premature termination caused by inadequate sedation (19). There is still an ongoing debate about the most appropriate sedative agent for complex endoscopic procedures such as ERCP. A recent Cochrane review identified four RCT comparing moderate sedation with midazolam and meperidine with propofol. There was no difference in mortality, serious cardiopulmonary complications or patient satisfaction between the two sedation techniques. The only difference was faster and better recovery in the propofol group (20).
Sedation for ERCP varies in different centers and between anesthesiologists. The options to choose from are deep sedation with propofol and general anesthesia. The decision is made based on procedural and patient characteristics. Some centers prefer to intubate only difficult cases which are expected to take longer time for completion. Others prefer to perform all ERCP under general anesthesia and there is a good reason for doing that although that approach is neither reasonable nor desirable. The main point in their defense is that anesthesiologist is not familiar to the endoscopy suite environment and potentially lack of all the equipment, medications and support personnel with whom they are accustomed in the operating room (21). Furthermore, there are older studies that indicate increased risk of complications and death if anesthesia is preformed outside of the operating room in so called remote places. These studies have become benchmark for establishing the rules sedation today.
The complexity of ERCP is variable, with a complexity scale from grades 1–4 proposed by the Quality Committee of the ASGE (22). Grades 1 and 2 are considered less challenging and are supposed to be completed in relatively shorter time compared to the more complex grades 3 and 4. The general opinion between centers is that unless patient characteristics dictates general anesthesia, usually ERCP grades 1 and 2 and even many grade 3 procedures may be done with deep propofol sedation without endotracheal intubation. Expected complex procedures which will require longer time for completion should be intubated in favor of patient safety and tolerance. Thus, for improving quality of ERCP it should be clearly stated and accepted as a routine practice, endoscopists to discuss each ERCP procedure with anesthesiologists to help guide decision making. It is important to communicate the expected complexity of the procedure and estimated time to perform it, together with any known gastrointestinal issues that might contribute to decision making such as increased aspiration risk related to known gastroparesis or gastric outlet obstruction.
Documentation of the technical aspects should include achieving deep cannulation of the desired duct, documenting stent insertion and stone extraction.
Cannulation rate
To succeed in ERCP the endoscopist should initially cannulate the desired duct, which is considered as one of the most challenging aspects of the whole procedure. That is why cannulation and failed attempts of cannulation should be recorded in all cases. Specific exclusion criteria for failed cannulation include inadequate sedation, retained gastric contents, prior abdominal surgeries such as pancreaticoduodenectomy, gastrojejunostomy, and hepaticojejunostomy, and obstruction of the antrum and the proximal duodenum. Successful cannulation should be measured on intact papilla and essentially means deep cannulation of the desired duct with the ability to inject contrast and facilitate insertion of various instruments.
A recent meta-analysis with a random-effects model suggests that cannulation rates in practice, even at tertiary-care centers, may be 90% (in the mid 80% range) and suggests significant difference in cannulation rates across the developed world (23). Some study groups have published data for successful cannulation in the range of 92–94% (15-17,24-26).
Based on the review of the literature ASGE/ACG task force suggests that physicians with consistently suboptimal cannulation rates (80% success) should consider undergoing further training or discontinuing their ERCP practices (1).
Stone extraction
Stone extraction should also be documented. The post-ERCP protocol should include data regarding size, number, location and whether complete extraction is achieved. Information about fluoroscopic anatomy of biliary tree- presence of strictures or abnormalities should also be included. According to one study expert endoscopy centers can achieve stone clearance irrespective of size in well over 90% of patients (27). Of course, this includes the use of additional techniques such as mechanical, laser, or electrohydraulic lithotripsy when standard techniques fail. Another study suggests that competent ERCP endoscopists can clear the duct of small to medium-sized common bile duct stones up to 1 cm in diameter in 90% of cases by using sphincterotomy and balloon or basket stone extraction in patients with normal biliary anatomy (28). Difficult large stones are usually tackled with a balloon sphincteroplasty. Main advantage of the procedure is the reduced risk for bleeding and perforation (29). However, the risk for post-ERCP pancreatitis (PEP) is higher if patients undergo balloon dilation without previously done sphincterotomy (29,30). Finally, ASGE states that successful stone extraction should be achieved in more than 85% of cases.
Stent placement
Documentation of stent placement should be included in every post-ERCP protocol. The documentation should include whether successful stent insertion is achieved and sufficient information about indication, stricture location, stent size and type, and the presence of post-surgical anatomy. This will facilitate comparisons and subsequent benchmark efforts. Review of the literature suggests that competent ERCP endoscopists should be able to place a biliary stent for relief of non-hilar biliary obstruction in more than 90% of patients (31,32).
Fluoroscopy
Fluoroscopy time and radiation dose should be measured and documented. Radiation exposure should be documented and reduced to the lowest possible level although some ERCP procedures are more difficult than others and require a longer overall fluoroscopy time. One study demonstrated that experienced endoscopists have significantly shorter radiation exposure time compared to the less experienced ones (15). Also, it should be noted that radiation dose varies depending on patient body habitus, use of copper filtration, distance of patient to the radiation source, magnification, oblique views, and spot images.
The post-procedure period
The post-procedure period is the time from removal of the endoscope to subsequent follow-up. In the post-procedure period endoscopist should prepare complete report of the procedure which describes the specific techniques performed, accessories used and overall outcome. The report should include documentation of adverse events if present. After the procedure endoscopist should explain to the patient the outcome and give appropriate instructions. Also, communication with the referring provider and follow-up of pathology is desirable to say the least.
ERCP report
ERCP report should include photo or video documentation of the procedure including fluoroscopic images, achievement of cannulation or failure to do so, clear depiction of the events in consecutive order and overall outcome. Unintended cannulation or injection with contrast of the pancreatic duct should also be reported. Clear and appropriate documentation of ERCP findings without concealing of facts, helps clinicians who are involved directly with patient medical care to make appropriate decisions on patient management.
Adverse events
Recognized adverse events such as bleeding, allergic reactions, cardiopulmonary events (including aspiration), perforation and PEP should be documented.
Post-ERCP pancreatitis is defined as abdominal pain after ERCP accompanied by serum amylase and lipase level three times the upper limit of normal (33). Review of the literature shows that rates of PEP are in the range of 1% to 7%. Some high-risk groups are excluded from these statistics. These are patients with known or suspected sphincter of Oddi dysfunction and those undergoing pancreatic endotherapy, who may warrant special prophylaxis for PEP including pancreatic stent placement or prophylactic use of nonsteroidal anti-inflammatory drugs (8,34-37).
Frequency of perforation occurring during ERCP is between 0.1% and 0.6% (34). Perforation may result from mechanical rupture of the esophagus, stomach, or duodenum from instrument passage, from sphincterotomy or passage of guidewires. Perforation may be intra-abdominal or retroperitoneal. Well established risk factors for perforation during ERCP include Billroth II or Roux-en-Y anatomy, presumed sphincter of Oddi dysfunction, intramural contrast material injection, sphincterotomy, biliary stricture dilatation and prolonged procedures (38,39). In patients undergoing ERCP who have normal anatomy, the expected perforation rate is less than 1%.
Bleeding related to ERCP is due to the use of electrocautery and sphincterotomy in majority of cases. Rate of clinically significant hemorrhage related to ERCP is approximately 1%, with most cases involving mild, intraluminal bleeding (40). Bleeding is usually divided to immediate bleeding during the procedure or delayed bleeding which can occur as far as 10 days after the procedure. Delayed bleeding is recognized by clinical evidence such as melena, with a drop-in hemoglobin level or need of blood transfusion within 10 days after ERCP (41). The expected rate of major post-sphincterotomy bleeding can be as high as 2% (42). Risk factors for post-sphincterotomy bleeding include coagulopathy, cholangitis, anticoagulant therapy within 3 days after the procedure, and low endoscopist case volume (<1 per week) (43). However, the risk of post-procedure bleeding is higher when other therapeutic maneuvers are performed, such as ampullectomy and transmural pseudo-cyst drainage (44,45).
Delayed adverse events should be documented by contacting the patients within 14 days after the procedure if possible.
ERCP quality network
A pilot project named ERCP quality network was established in 2013 in United States attempting to better assess quality in ERCP. The idea is to collect and compare data on the practice and quality of ERCP by individual endoscopists. This data is than uploaded onto a secure website, analyzed automatically and the results are posted immediately. Data points include above mentioned criteria like indications, complexity grade, sedation, fluoroscopy times, success rates of deep cannulation, stenting, etc. Additional benefit is that each endoscopist may view a summary of its own performance and compare it with other participants. In the first 6 months of the study 2,300 ERCP procedures were entered by 24 United States endoscopists and the results were similar to the ASGE recommended standards. The deep biliary cannulation rate averaged 95%, success rates for biliary stones below 10 mm was 97%, falling to 89% for stones above 10 mm. and overall reported complication rate was 3% mild, and 1% moderate (46).
Self-assessment program
Recently a study group from Erasmus medical center in Rotterdam, The Netherlands proposed a self-assessment program to better measure quality in endoscopy. The Rotterdam Assessment Form for ERCP (RAF-E) was based on a form filled by each endoscopist who participated in the research. The form was filled upon completion of the procedure and included objective a subjective criterion. Despite some drawbacks that the study had, like it was performed in a single tertiary center, not national wide and the impact of trainees was not established, it had very interesting results. Despite the relatively small volume of ERCP procedures included—1,651, it concluded that there is no correlation between volume and performance of the practicing endoscopists. The one with the lowest volume was not the worst performer and vice versa. Overall it proved that a simple self-assessing form can be a valuable method to gain insight in ERCP performance (47).
Conclusions
ERCP is one of the most technically demanding procedures in gastroenterology, with an obligatory learning curve to master and a certain level of procedures to maintain proficiency. The clinical benefits of ERCP are very firmly established, but in recent years there is a rising concern regarding procedural quality and how exactly it should be measured. Various endoscopic organizations have published their guidelines and suggestions for quality measures, but they are somewhat difficult to apply in everyday practice. Possibly a united international program for assessing quality containing the abovementioned parameters is the way for achieving quality assessment of ERCP. Therefore, the newly established ERCP quality network and self-assessment program may give the most accurate insight of the problem, although further research must be conducted.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- ASGE Quality Indicators for ERCP guideline 2015. Available online: https://www.nature.com/articles/ajg2014386
- Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA 1998;280:1000-5. [Crossref] [PubMed]
- Rizk MK, Sawhney MS, Cohen J, et al. Quality indicators common to all GI endoscopic procedures. Gastrointest Endosc 2015;81:3-16. [Crossref] [PubMed]
- Jowell PS, Baillie J, Branch MS, et al. Quantitative assessment of procedural competence. A prospective study of training in endoscopic retro- grade cholangiopancreatography. Ann Intern Med 1996;125:983-9. [Crossref] [PubMed]
- Hawes RH. Diagnostic and therapeutic uses of ERCP in pancreatic and biliary tract malignancies. Gastrointest Endosc 2002;56:S201-5. [Crossref] [PubMed]
- Adler DG, Baron TH, Davila RE, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc 2005;62:1-8. [Crossref] [PubMed]
- Nathan T, Kjeldsen J, Schaffalitzky de Muckadell OB. Prediction of therapy in primary endoscopic retrograde cholangiopancreatography. Endoscopy 2004;36:527-34. [Crossref] [PubMed]
- Pasricha PJ. There is no role for ERCP in unexplained abdominal pain of pancreatic or biliary origin. Gastrointest Endosc 2002;56:S267-72. [Crossref] [PubMed]
- Imler TD, Sherman S, McHenry L, et al. Low yield of significant findings on endoscopic retrograde cholangiopancreatography in patients with pancreatobiliary pain and no objective findings. Dig Dis Sci 2012;57:3252-7. [Crossref] [PubMed]
- Cohen S, Bacon BR, Berlin JA, et al. National Institutes of Health State- of-the-Science Conference Statement: ERCP for diagnosis and therapy, January 14-16, 2002. Gastrointest Endosc 2002;56:803-9. [Crossref] [PubMed]
- van der Gaag NA, Rauws EA, van Eijck CH, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 2010;362:129-37. [Crossref] [PubMed]
- Alkhatib AA, Hilden K, Adler DG. Comorbidities, sphincterotomy, and balloon dilation predict post-ERCP adverse events in PSC patients: operator experience is protective. Dig Dis Sci 2011;56:3685-8. [Crossref] [PubMed]
- ASGE Standards of Practice Committee, Banerjee S, Shen B, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 2008;67:791-8. [Crossref] [PubMed]
- Shahidi N, Ou G, Telford J, et al. When trainees reach competency in performing ERCP: a systematic review. Gastrointest Endosc 2015;81:1337-42. [Crossref] [PubMed]
- Wu J, Hu B. The role of carbon dioxide insufflation in colonoscopy: asystematic review and meta-analysis. Endoscopy 2012;44:128-36. [Crossref] [PubMed]
- Cadoni S, Falt P, Gallittu P, et al. Water exchange is the least painfulinsertion technique and increases completion of unsedated colonoscopy. Clin Gastroenterol Hepatol 2015;13:1972-80.e1. [Crossref] [PubMed]
- Cohen LB, Wecsler JS, Gaetano JN, et al. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol 2006;101:967-74. [Crossref] [PubMed]
- Jeurnink SM, Steyerberg E, Kuipers E, et al. The burden of endoscopic retrograde cholangiopancreatography (ERCP) performed with the patient under conscious sedation. Surg Endosc 2012;26:2213-9. [Crossref] [PubMed]
- Raymondos K, Panning B, Bachem I, et al. Evaluation of endoscopic retrograde cholangiopancreatography under conscious sedation and general anesthesia. Endoscopy 2002;34:721-6. [Crossref] [PubMed]
- Tsujino T, Isayama H, Komatsu Y, et al. Risk factors for pancreatitis in patients with common bile duct stones managed by endoscopic papillary balloon dilation. Am J Gastroenterol 2005;100:38-42. Erratum in: Am J Gastroenterol 2005;100:507. [Crossref] [PubMed]
- Cook T, Behringer EC, Benger J. Airway management outside the operating room: hazardous and incompletely studied. Curr Opin Anaesthesiol 2012;25:461-9. [Crossref] [PubMed]
- Cotton PB, Eisen G, Romagnuolo J, et al. Grading the complexity of endoscopic procedures: results of an ASGE working party. Gastrointest Endosc 2011;73:868-74. [Crossref] [PubMed]
- DeBenedet AT, Elmunzer BJ, McCarthy ST, et al. Intraprocedural quality in endoscopic retrograde cholangiopancreatography: a meta-analysis. Am J Gastroenterol 2013;108:1696-704; quiz 1705.
- Colton JB, Curran CC. Quality indicators, including complications, of ERCP in a community setting: a prospective study. Gastrointest Endosc 2009;70:457-67. [Crossref] [PubMed]
- Enochsson L, Swahn F, Arnelo U, et al. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCP. Gastrointest Endosc 2010;72:1175-84, 1184.e1-3.
- Suissa A, Yassin K, Lavy A, et al. Outcome and early complications of ERCP: a prospective single center study. Hepatogastroenterology 2005;52:352-5. [PubMed]
- Jorgensen JE, Rubenstein JH, Goodsitt MM, et al. Radiation doses to ERCP patients are significantly lower with experienced endoscopists. Gastrointest Endosc 2010;72:58-65. [Crossref] [PubMed]
- Lauri A, Horton RC, Davidson BR, et al. Endoscopic extraction of bile duct stones: management related to stone size. Gut 1993;34:1718-21. [Crossref] [PubMed]
- Garewal D, Powell S, Milan SJ, et al. Sedative techniques for endoscopic retrograde cholangiopancreatography Cochrane Database Syst Rev 2012;6. [PubMed]
- Feng Y, Zhu H, Chen X, et al. Comparison of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for retrieval of choledocholithiasis: a meta-analysis of randomized controlled trials. J Gastroenterol 2012;47:655-63. [Crossref] [PubMed]
- Carr-Locke DL. Therapeutic role of ERCP in the management of suspected common bile duct stones. Gastrointest Endosc 2002;56:S170-4. [Crossref] [PubMed]
- Cotton PB. Income and outcome metrics for the objective evaluation of ERCP and alternative methods. Gastrointest Endosc 2002;56:S283-90. [Crossref] [PubMed]
- Banerjee N, Hilden K, Baron TH, et al. Endoscopic biliary sphincteroto- my is not required for transpapillary SEMS placement for biliary obstruction. Dig Dis Sci 2011;56:591-5. [Crossref] [PubMed]
- Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991;37:383-93. [Crossref] [PubMed]
- Cotton PB. ERCP is most dangerous for people who need it least. Gastrointest Endosc 2001;54:535-6. [Crossref] [PubMed]
- Cotton PB, Garrow DA, Gallagher J, et al. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 2009;70:80-8. [Crossref] [PubMed]
- Elmunzer BJ, Scheiman JM, Lehman GA, et al. U.S. Cooperative for Out- comes Research in Endoscopy (USCORE). A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med 2012;366:1414-22. [Crossref] [PubMed]
- Elmunzer BJ, Higgins PD, Saini SD, et al. United States Cooperative for Outcomes Research in Endoscopy. Does rectal indomethacin eliminate the need for prophylactic pancreatic stent placement in patients undergoing high-risk ERCP? Post hoc efficacy and cost-benefit analyses using prospective clinical trial data. Am J Gastroenterol 2013;108:410-5. [Crossref] [PubMed]
- Williams EJ, Taylor S, Fairclough P, et al. Risk factors for complication following ERCP: results of a large-scale, prospective multicenter study. Endoscopy 2007;39:793-801. [Crossref] [PubMed]
- Faylona JM, Qadir A, Chan AC, et al. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy 1999;31:546-9. [Crossref] [PubMed]
- Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post- ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 2007;102:1781-8. [Crossref] [PubMed]
- Tenca A, Pugliese D, Consonni D, et al. Bleeding after sphincterotomy in liver transplanted patients with biliary complications. Eur J Gastroenterol Hepatol 2011;23:778-81. [Crossref] [PubMed]
- Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med 1996;335:909-18. [Crossref] [PubMed]
- Cheng CL, Sherman S, Fogel EL, et al. Endoscopic snare papillectomy for tumors of the duodenal papillae. Gastrointest Endosc 2004;60:757-64. [Crossref] [PubMed]
- Baron TH, Harewood GC, Morgan DE, et al. Outcome differences after endoscopic drainage of pancreatic necrosis, acute pancreatic pseudocysts, and chronic pancreatic pseudocysts. Gastrointest Endosc 2002;56:7-17. [Crossref] [PubMed]
- Cotton PB, Romagnuolo J, Faigel DO, et al. The ERCP quality network: a pilot study of benchmarking practice and performance. Am J Med Qual 2013;28:256-60. [Crossref] [PubMed]
- Ekkelenkamp VE, Koch AD, Haringsma J, et al. Quality evaluation through self-assessment: a novel method to gain insight into ERCP performance. Frontline Gastroenterol 2014;5:10-6. [Crossref] [PubMed]


