Physiologic assessment of moderate coronary lesions: a step towards complete revascularization in coronary artery bypass grafting
Introduction
Coronary artery disease (CAD) affects approximately 6.3% of the adult American population and is thought to be responsible for nearly one third of all deaths in adults over the age of 35 (1,2). In addition, 720,000 Americans will likely suffer their first myocardial infarction (MI) or death due to coronary artery disease in 2018, and 335,000 will have a recurrent event (1). The two major strategies for revascularization of CAD are percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). In 2014, an estimated 371,000 inpatient CABGs were performed in the USA (1). Notably, the average costs of CABG over the past 10 years in the USA range from roughly $28,000 to $38,000 with an average of 6.9 inpatient days required per procedure (1,3). Given the prevalence and costs associated with CAD, improving outcomes for patients undergoing CABG is important in managing the burden of CAD on the U.S. health care system (4).
Incomplete revascularization is an independent risk factor for adverse outcomes after CABG (5). On the other hand, complete revascularization reduces mortality, MI, and the need for repeat revascularization in patients with multi-vessel coronary artery disease (6-8). However, the definition of “complete revascularization” for patients undergoing CABG is inconsistent. Anatomic, functional, numeric, score-based, and physiology-based definitions have all been used (7,9,10). Regardless of the definition, any complete revascularization by CABG requires an accurate assessment of CAD. Accurate assessment of moderate coronary lesions is best achieved with physiologic measurements such as fractional flow reserve (FFR) or instantaneous wave-free ratio (iFR) (11-18). However, FFR and iFR are not routinely performed prior to CABG, and data supporting physiologic assessment to guide CABG are scarce (19,20). Neither FFR nor iFR has been adequately studied in a randomized controlled trial of CABG patients, although a physiology-based complete revascularization might lead to better outcomes. Thus, we compared an anatomic to a physiology-based assessment of moderate coronary lesions in patients referred for CABG.
Methods
Study population
We retrospectively reviewed medical records for patients who underwent CABG at Tulane Medical Center from April 1, 2014 to April 1, 2016. The inclusion criteria were all patients who underwent CABG during the above pre-specified time period. There were no exclusion criteria. Patients were divided into two groups: the FFR/iFR-guided group and the angiography-guided group. The FFR/iFR-guided group included patients who had at least 1 intermediate coronary stenosis (40–70%) measured by FFR or iFR. The angiography-guided group included patients who did not have any FFR or iFR measurement performed during the preoperative coronary angiogram.
Coronary angiography, FFR/iFR measurement, and CABG
Experienced operators performed all diagnostic angiography by either femoral or radial approach. All procedural and technical aspects of the diagnostic procedures were based on operator preference including diagnostic catheters, guiding catheters, dose of intracoronary adenosine, and pressure-monitoring guide wire systems. FFR value of ≤0.80 and iFR value of ≤0.89 was considered abnormal and diagnostic of an ischemic lesion. The same operator performed each CABG with all procedural and technical aspects of the procedure based upon the surgeon’s preference. Each CABG was on-pump.
Extracted clinical characteristics and outcomes
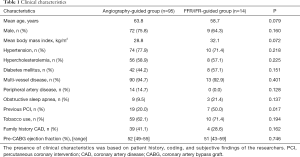
Extracted clinical characteristics for the FFR/iFR-guided and angiography-guided groups included age, sex, body mass index, hypertension, dyslipidemia, diabetes mellitus, multi-vessel coronary artery disease, peripheral vascular disease, obstructive sleep apnea, previous PCI, tobacco use, family history of cardiac disease, and preoperative left ventricular ejection fraction.
Procedural outcomes of CABG included number of anastomoses, grafted coronary artery distribution, and length of hospitalization associated with surgery. In addition, clinical outcomes for the study included the rate of major adverse cardiac events (MACEs), defined as the combination of overall death, MI, and target vessel revascularization (TVR), the individual MACE end points, time to MACE, and angina through an 18-month follow-up period. The Institutional review board at our institution approved the application and protocol for this research study, waiving the requirement for informed consent.
Statistical analysis
The statistical analysis was performed with SAS (SAS Institute Inc., Cary, NC, USA). All continuous variables are expressed as mean or median as appropriate, and categorical variables as frequencies and percentages. All comparisons between variables and outcomes were performed with the χ2 or the Fisher exact tests as appropriate. A P value of <0.05, two tailed, was considered statistically significant.
Results
The study population consisted of 109 patients: 14 patients in the FFR/iFR-guided group (12 FFR and 2 iFR) and 95 patients in the angiography-guided group. All clinical characteristics are listed in Table 1. In the overall study population, 50% of patients in the FFR/iFR group had undergone previous PCI compared to 20% in the angiography group (P<0.05), but otherwise no significant differences in baseline characteristics between groups were observed.
Full table
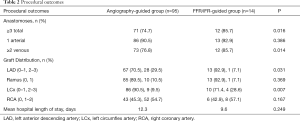
Table 2 displays the procedural outcomes of the comparison groups. After CABG, the number of total anastomoses per group was significantly different. In the FFR/iFR group 85.7% had ≥3 anastomoses compared to angiography group 74.7% (P<0.05). The rates of arterial grafts were not different between groups. The rates of venous grafts were significantly different with 85.7% receiving ≥2 grafts in the FFR/iFR group compared with 76.8% in the angiography group (P<0.05). There were also some differences in the coronary distribution of grafts. The FFR/iFR group had a lower rate of ≥2 grafts to the left anterior descending artery (LAD) distribution compared to the angiography group (7.1% vs. 29.5%, P<0.05). However, the FFR/iFR group had a higher rate ≥2 grafts to the left circumflex (LCx) distribution than the angiography group (28.6% vs. 9.5%, P<0.05). There were no significant differences in the graft distribution used for the RCA or the ramus. Additionally, rates were similar for mean length of hospitalization in both groups.
Full table
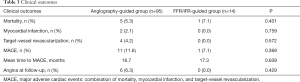
Clinical outcomes are listed in Table 3. There was only a trend toward reduction in MACE in the FFR/iFR group compared to the angiography group (7.1% vs. 11.6%, P=0.369). There were no significant differences in individual outcomes of mortality, MI, or revascularization between the groups, and mean time to MACE was similar. Nevertheless, there was also a trend toward lower rates of post-operative angina in the FFR/iFR group (0.0% vs. 6.3%, P=0.429). Of note, none of the patients included in this study underwent CABG for an acute coronary syndrome, nor did any of them have concomitant valve replacement or repair. All patients in this retrospective study were evaluated during outpatient follow-up.
Full table
Discussion
While only few previous studies have been published, our findings similarly suggest that a physiology-based assessment is feasible and can effectively achieve complete revascularization in CABG (19,20). Moreover, physiologic assessment can also influence the revascularization strategy as evidenced by the higher rate of patients who received at least three anastomoses or at least two venous grafts in the FFR/iFR group. The FFR/iFR group also received more grafts to the circumflex distribution. Additionally, we observed a trend toward reduced MACEs and the occurrence of post-operative angina.
For several decades, the benefits of complete revascularization have been established (5,6). Recently, there has been renewed interest in the importance of complete revascularization for multi-vessel coronary artery disease (21-24). In addition, for patients undergoing CABG, complete revascularization by placing at least three bypass grafts has been associated with improved survival compared to fewer grafts (6). However, the majority of prior CABG studies were based on an anatomic definition of complete revascularization rather than a physiologic assessment of coronary lesions. In contrast to the routine measurement of FFR in patients considered for PCI, physiologic assessment is rarely performed before surgical revascularization likely due to limited CABG data (11-20). Of note, there are data that nearly 20% of bypass grafts to angiographic diseased vessels do not appear to alter regional myocardial blood flow (25). Therefore, an FFR-based functional assessment to guide complete revascularization of multi-vessel disease should be considered (19,26).
To our knowledge, there are no published randomized clinical trials that have examined the dedicated use of FFR or iFR to guide CABG. For patients undergoing PCI, physiologic assessment by FFR leads to improved cardiac outcomes, and iFR has recently been shown to be non-inferior to FFR as a physiologic measurement (11-18). Observational data of CABG patients have suggested that the incidence of multi-vessel disease is decreased by FFR, resulting in fewer bypass grafts, reduced graft occlusion, and less angina (19,20). Downgrading of coronary lesion severity by FFR is commonly reported in most clinical studies (13-15,20,26). In our investigation, however, the number and distribution of bypass grafts were actually increased in the FFR/iFR group. While our findings are different from prior observational data, they actually support a similar concept: physiologic assessment influences CABG revascularization strategy on the whole.
Some cardiothoracic surgeons have supported a physiology-based complete revascularization, noting the positive impact of FFR on PCI outcomes, its ability to discern the risk of adverse cardiac events, and the recognition of FFR as a reference standard to assess the functional severity of moderate coronary lesions (27-29). However, a lack of randomized clinical data and several technical challenges have limited the standard adoption of a physiology-guided CABG. It is unknown how one graft in a specific arterial distribution might affect the FFR/iFR of a lesion in a different vessel, particularly if communicating collaterals are present. Additionally, difficulty in performing an accurate physiologic measurement in patients with left main or multi-segment disease can reduce the precision of FFR or iFR (29). The FFR of diffuse lesions or those in tandem sequence are likely to be inaccurate, and PCI of a primary lesion may be required to determine the true FFR of non-primary lesions (30-32). Also, micro-vascular dysfunction may result in a preserved FFR or iFR due to fixed micro-vascular resistance, thus limiting the usefulness of these measurements (33,34).
Our study has several notable limitations. This is a single-center, retrospective observational study and influenced by biases and confounders inherent to all retrospective analyses, particularly an inherent selection bias. The number of patients in the FFR/iFR group compared with the angiography group is relatively small and unbalanced between the groups. Half of the patients in the FFR/iFR group had prior PCI before undergoing CABG suggesting that FFR or iFR may have been performed in patients with complex-appearing disease where values were likely to be abnormal. Another consideration is physiologic measurements was possibly underutilized for patients with moderate-appearing disease who could have derived true benefit. In general, underutilization of coronary physiologic assessment is prevalent despite its endorsement from randomized clinical trials and guidelines. Overall, stenosis severity is perhaps still based on visual assessment about 70% of the time, resulting in discordance with FFR in almost 50% of cases (35). Although more experience with FFR correlates with higher utilization, the concordant decision rate based on either angiography or FFR still lies below 60% (35).
Conclusions
An FFR/iFR-guided CABG can effectively achieve complete revascularization in patients undergoing CABG. Notably, FFR/iFR-guided CABG was associated with higher rates of three-vessel anastomoses, venous grafting, and graft distribution to the circumflex system. A trend toward reduced rates of MACE and angina during an 18-month follow-up period were observed. Randomized controlled trials are needed to examine the appropriate application of a physiology-based complete revascularization in patients undergoing CABG. Given the high burden of CAD on morbidity, mortality, and costs, improving outcomes for patients undergoing CABG may help reduce the burden of CAD on the U.S. healthcare system.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. O Mogabgab reports consultant fees from Philips Corporation. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional review board of Tulane University School (IRB number: 1076086) and written informed consent was waived.
References
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67-e492. [Crossref] [PubMed]
- Sanchis-Gomar F, Perez-Quilis C, Leischik R, et al. Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med 2016;4:256. [Crossref] [PubMed]
- Osnabrugge RL, Speir AM, Head SJ, et al. Prediction of costs and length of stay in coronary artery bypass grafting. Ann Thorac Surg 2014;98:1286-93. [Crossref] [PubMed]
- Osnabrugge RL, Speir AM, Head SJ, et al. Cost, quality, and value in coronary artery bypass grafting. J Thorac Cardiovasc Surg 2014;148:2729-35.e1. [Crossref] [PubMed]
- Kleisli T, Cheng W, Jacobs MJ, et al. In the current era, complete revascularization improves survival after coronary artery bypass surgery. J Thorac Cardiovasc Surg 2005;129:1283-91. [Crossref] [PubMed]
- Bell MR, Gersh BJ, Schaff HV, et al. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation 1992;86:446-57. [Crossref] [PubMed]
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 2013;62:1421-31. [Crossref] [PubMed]
- Zimarino M, Ricci F, Romanello M, et al. Complete myocardial revascularization confers a larger clinical benefit when performed with state-of-the-art techniques in high-risk patients with multivessel coronary artery disease: A meta-analysis of randomized and observational studies. Catheter Cardiovasc Interv 2016;87:3-12. [Crossref] [PubMed]
- Ong AT, Serruys PW. Complete revascularization: coronary artery bypass graft surgery versus percutaneous coronary intervention. Circulation 2006;114:249-55. [Crossref] [PubMed]
- Sandoval Y, Brilakis ES, Canoniero M, et al. Complete versus incomplete coronary revascularization of patients with multivessel coronary artery disease. Curr Treat Options Cardiovasc Med 2015;17:366. [Crossref] [PubMed]
- Uren NG, Melin JA, De Bruyne B, et al. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med 1994;330:1782-8. [Crossref] [PubMed]
- Di Carli M, Czernin J, Hoh CK, et al. Relation among stenosis severity, myocardial blood flow, and flow reserve in patients with coronary artery disease. Circulation 1995;91:1944-51. [Crossref] [PubMed]
- Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105-11. [Crossref] [PubMed]
- Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213-24. [Crossref] [PubMed]
- De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991-1001. [Crossref] [PubMed]
- De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 2014;371:1208-17. [Crossref] [PubMed]
- Davies JE, Sen S, Dehbi HM, et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med 2017;376:1824-34. [Crossref] [PubMed]
- Götberg M, Christiansen EH, Gudmundsdottir IJ, et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med 2017;376:1813-23. [Crossref] [PubMed]
- Botman CJ, Schonberger J, Koolen S, et al. Does stenosis severity of native vessels influence bypass graft patency? A prospective fractional flow reserve-guided study. Ann Thorac Surg 2007;83:2093-7. [Crossref] [PubMed]
- Toth G, De Bruyne B, Casselman F, et al. Fractional flow reserve-guided versus angiography-guided coronary artery bypass graft surgery. Circulation 2013;128:1405-11. [Crossref] [PubMed]
- Buda AJ, Macdonald IL, Anderson MJ, et al. Long-term results following coronary bypass operation. Importance of preoperative factors and complete revascularization. J Thorac Cardiovasc Surg 1981;82:383-90. [PubMed]
- Jones EL, Craver JM, Guyton RA, et al. Importance of complete revascularization in performance of the coronary bypass operation. Am J Cardiol 1983;51:7-12. [Crossref] [PubMed]
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011;124:e574-651. [Crossref] [PubMed]
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg 2014;46:517-92. [Crossref] [PubMed]
- Ferguson TB Jr, Chen C, Babb JD, et al. Fractional flow reserve-guided coronary artery bypass grafting: can intraoperative physiologic imaging guide decision-making? J Thorac Cardiovasc Surg 2013;146:824-35.e1. [Crossref] [PubMed]
- Nam CW, Mangiacapra F, Entjes R, et al. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J Am Coll Cardiol 2011;58:1211-8. [Crossref] [PubMed]
- Casselman F, Van der Merwe J, Ferrara A, et al. The present day potential role of fractional flow reserve-guided coronary artery bypass graft surgery. J Thorac Cardiovasc Surg 2016;151:926-32. [Crossref] [PubMed]
- Boyd JH. FFR 4 CABG: More than a vanity plate. J Thorac Cardiovasc Surg 2016;151:933-4. [Crossref] [PubMed]
- Shah T, Geleris JD, Zhong M, et al. Fractional flow reserve to guide surgical coronary revascularization. J Thorac Dis 2017;9:S317-26. [Crossref] [PubMed]
- Pijls NH, De Bruyne B, Bech GJ, et al. Coronary pressure measurement to assess the hemodynamic significance of serial stenoses within one coronary artery: validation in humans. Circulation 2000;102:2371-7. [Crossref] [PubMed]
- De Bruyne B, Pijls NH, Heyndrickx GR, et al. Pressure-derived fractional flow reserve to assess serial epicardial stenoses: theoretical basis and animal validation. Circulation 2000;101:1840-7. [Crossref] [PubMed]
- Kim HL, Koo BK, Nam CW, et al. Clinical and physiological outcomes of fractional flow reserve-guided percutaneous coronary intervention in patients with serial stenoses within one coronary artery. JACC Cardiovasc Interv 2012;5:1013-8. [Crossref] [PubMed]
- Johnson NP, Kirkeeide RL, Gould KL. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc Imaging 2012;5:193-202. [Crossref] [PubMed]
- van de Hoef TP, Nolte F. Impact of hyperaemic microvascular resistance on fractional flow reserve measurements in patients with stable coronary artery disease: insights from combined stenosis and microvascular resistance assessment. Heart 2014;100:951-9. [Crossref] [PubMed]
- Toth GG, Toth B, Johnson NP, et al. Revascularization decisions in patients with stable angina and intermediate lesions: results of the international survey on interventional strategy. Circ Cardiovasc Interv 2014;7:751-9. [Crossref] [PubMed]


